Health care faces evolving challenges
National landscape
COVID-19 changed the way we live, work and play in ways both big and small. There may be no better example of this change than in health care, where an entire industry shifted the way it operates to ensure communities had high-quality care. From delaying elective procedures at the outset of the pandemic, to investing in testing and vaccine capabilities, COVID-19 drastically altered the way hospitals and health care providers operate. Health care as a whole is still grappling with that transformation.
 Labor shortages, a long-standing issue in health care, were worsened by COVID-19. Nationwide, many health care providers became burned out because of the pandemic and some have left the field entirely, leaving a larger-than-anticipated void in doctors, providers and nurses. According to Kaufman Hall’s 2022 Workforce Report, during the pandemic, almost one in five health care workers quit their jobs. According to the Association of American Medical Colleges, there is an estimated shortage of between 37,800 and 124,000 physicians across the nation by 2034, including shortfalls in both primary and specialty care.
Labor shortages, a long-standing issue in health care, were worsened by COVID-19. Nationwide, many health care providers became burned out because of the pandemic and some have left the field entirely, leaving a larger-than-anticipated void in doctors, providers and nurses. According to Kaufman Hall’s 2022 Workforce Report, during the pandemic, almost one in five health care workers quit their jobs. According to the Association of American Medical Colleges, there is an estimated shortage of between 37,800 and 124,000 physicians across the nation by 2034, including shortfalls in both primary and specialty care.
 The report found that nationally, hospital labor expenses increased by more than one-third from pre-pandemic levels. The largest increases were in the South and West. Contract labor as a percentage of total labor expenses increased more than five times the rate from pre-pandemic levels. As of March 2022, the median wage rate for contract nurses had risen to more than three times that of employed nurses.
The report found that nationally, hospital labor expenses increased by more than one-third from pre-pandemic levels. The largest increases were in the South and West. Contract labor as a percentage of total labor expenses increased more than five times the rate from pre-pandemic levels. As of March 2022, the median wage rate for contract nurses had risen to more than three times that of employed nurses.
In 2022, hospitals saw dramatic declines in operating margin in a perfect storm of expense, volume and revenue pressures.
North Carolina hospitals are not immune to the national reality
These national issues are not unique to a single state or health system. North Carolina hospitals are at risk, and the state’s safety net is in danger of unraveling because of the immense cost, and the environmental and policy pressures placed on hospitals and health systems. Right now, more than 60 percent of North Carolina hospitals have a negative operating income, and the 2022 projected losses for all NC Hospitals combined are estimated at over $2 billion.
National labor shortages have forced hospitals to utilize more contract labor, which is up 100 percent over the previous year. Additionally, Medicaid Managed Care has reduced reimbursement for services significantly. All in all, hospital expenses have grown significantly with no opportunity for additional revenue.
These challenges present a very significant threat to health systems’ ability to provide high-quality care in communities across the state.
Rural health care in crisis
Rural health care has long been overburdened and under-resourced. ECU Health’s 29-county service area is one of the largest rural regions in the entire country, with more than 1.4 million people.
A disproportionate number of eastern North Carolinians are underinsured and suffer from higher rates of chronic diseases like heart disease, stroke and diabetes. This means many in our region require care after their conditions have worsened, resulting in a higher level of needed care at a larger expense.
This reality is not confined to eastern North Carolina. In rural areas across the country, health care is simply unsustainable. According to UNC Sheps Center, 181 rural hospitals have closed across the country since 2005, 11 of which were right here in North Carolina.
ECU Health is acting to solve these challenges…
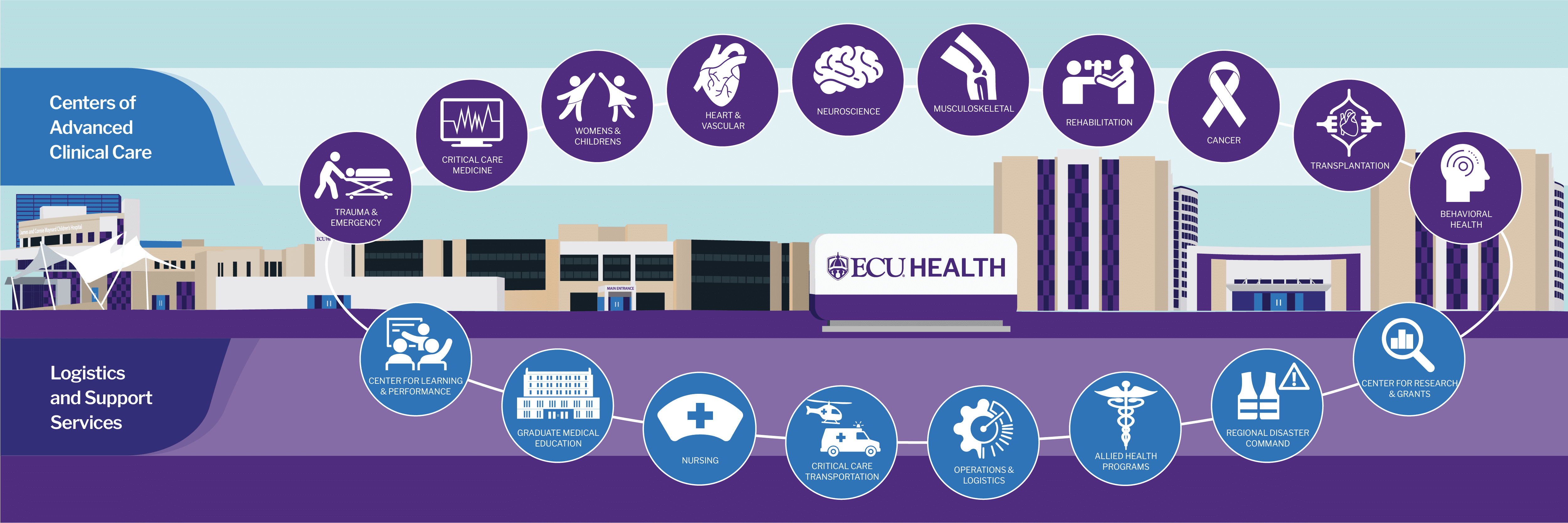
Transforming the health system
ECU Health represents a never-before-seen level of collaboration among regional leaders who are all committed to delivering upon the mission of improving the health and well-being of eastern North Carolina. The health system, alongside its partner, the Brody School of Medicine at East Carolina University, is a nationally recognized academic rural health brand. The health system and the Brody School of Medicine have been closely aligned for decades, working together to solve the complex challenges of rural health care. As ECU Health, the two organizations are working in tandem to bring clinical and academic excellence to the region.
Recruitment and retention
ECU Health is committed to recruiting the best providers, nurses and care teams for the region. The ongoing labor shortage makes it more important than ever to have a strong brand that attracts a talented workforce. ECU Health is uniquely positioned to attract mission-oriented health care workers who have the opportunity to serve in a large academic medical center, or in other hospitals and clinics located in communities across the region.
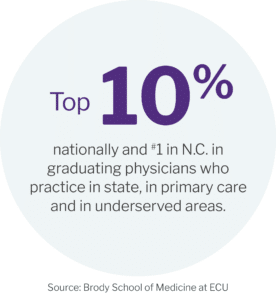 Academic mission
Academic mission
The Brody School of Medicine at East Carolina University’s success with training the next generation of rural health providers for North Carolina is vital to not only the state, but to eastern North Carolina. This success is highlighted by the Rural Family Medicine Residency Program, which places residents in practices across eastern North Carolina where they can have a higher impact in a smaller community. At a time when primary care providers are in high demand and short supply, Brody is helping produce graduates that practice primary care thanks to efforts like the Rural Family Medicine Residency Program. As of 2019, more than half of East Carolina University’s medical school graduates were practicing in North Carolina and more than half of those graduates were in primary care practice.
Nursing
ECU Health’s partnership with ECU is crucial to recruiting nurses. The College of Nursing at East Carolina University prepares more new nurses for North Carolina than any other four-year institution.
The health system recently launched a travel staffing program with the goal of attracting, retaining and developing team members. The program offers staffing options, decreases dependency on external travelers and provides unique, flexible options for the ECU Health team.
Community Outreach
ECU Health invested tremendous energy during COVID to connect with our community where they live using grassroots efforts to inform and engage those in need. These lessons and new innovations are now being used to provide health screenings in the community in an effort to prevent and catch disease early.
Partnerships
ECU Health is committed to developing partnerships to solve the complex challenges of providing care in rural eastern North Carolina. ECU Health is more than a health system and school of medicine, it is a collaboration with business partners, not for profits, elected and appointed government officials, education institutions and so many more. Partnership is how we solve the unique challenges of providing high-quality care and helping to sustain the economic engine for the region. Healthy community members are necessary for the region to thrive.
… and we continue to advocate for rural health care
ECU Health continues to advocate in Raleigh and Washington D.C. for various policies that will support rural health care.
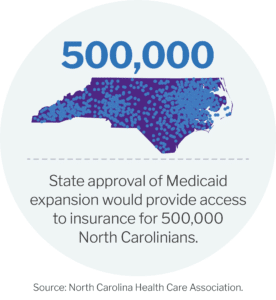
In March 2023, North Carolina Gov. Roy Cooper signed Medicaid expansion into law. For more than six years, ECU Health advocated Medicaid expansion as the health system serves a vast rural region with a large number of uninsured patients. Medicaid expansion is a vital initiative that will help improve access to care for people across the state and better health systems to provide high-quality care to all. More than 500,000 North Carolinians – more than 100,000 of whom live in the east – will now become eligible for the coverage they need to get care for chronic conditions, prevent illness and disease progression and live healthy, productive lives.