Transplantation provides hope for new life and renewed health for those with kidney failure.
Chronic kidney disease is a major health concern affecting more than eight million Americans. When kidney function declines beyond a certain level, patients have end-stage kidney disease and require either dialysis or transplantation to sustain life. A kidney transplant is one of the most common organ transplant surgeries performed today. Kidneys that aren’t working well are replaced with a donor kidney from a living or deceased donor.
What is a Kidney Transplant?
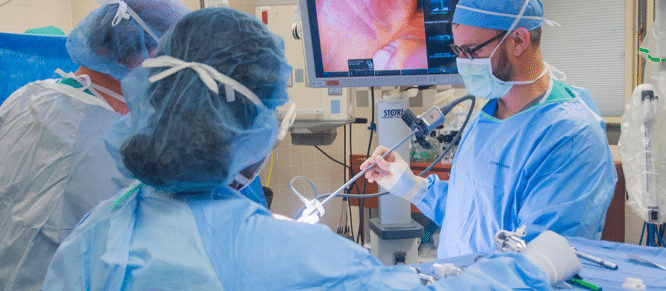
Kidney transplantation is a surgical procedure to replace a diseased or low-functioning kidney with a healthy kidney from another person. The kidney may come from a deceased donor or from a living donor.
Typically, the transplanted kidney is implanted in the lower abdomen on the right or left of the body. Most recipients usually receive one kidney. In rare situations, the patient may receive two kidneys. In most cases, diseased kidneys are left in place during and following the transplant procedure.
Types of Kidney Transplant
The ECU Health care team will partner with you to determine the best treatment option based on your unique needs.
Living Donor Transplant

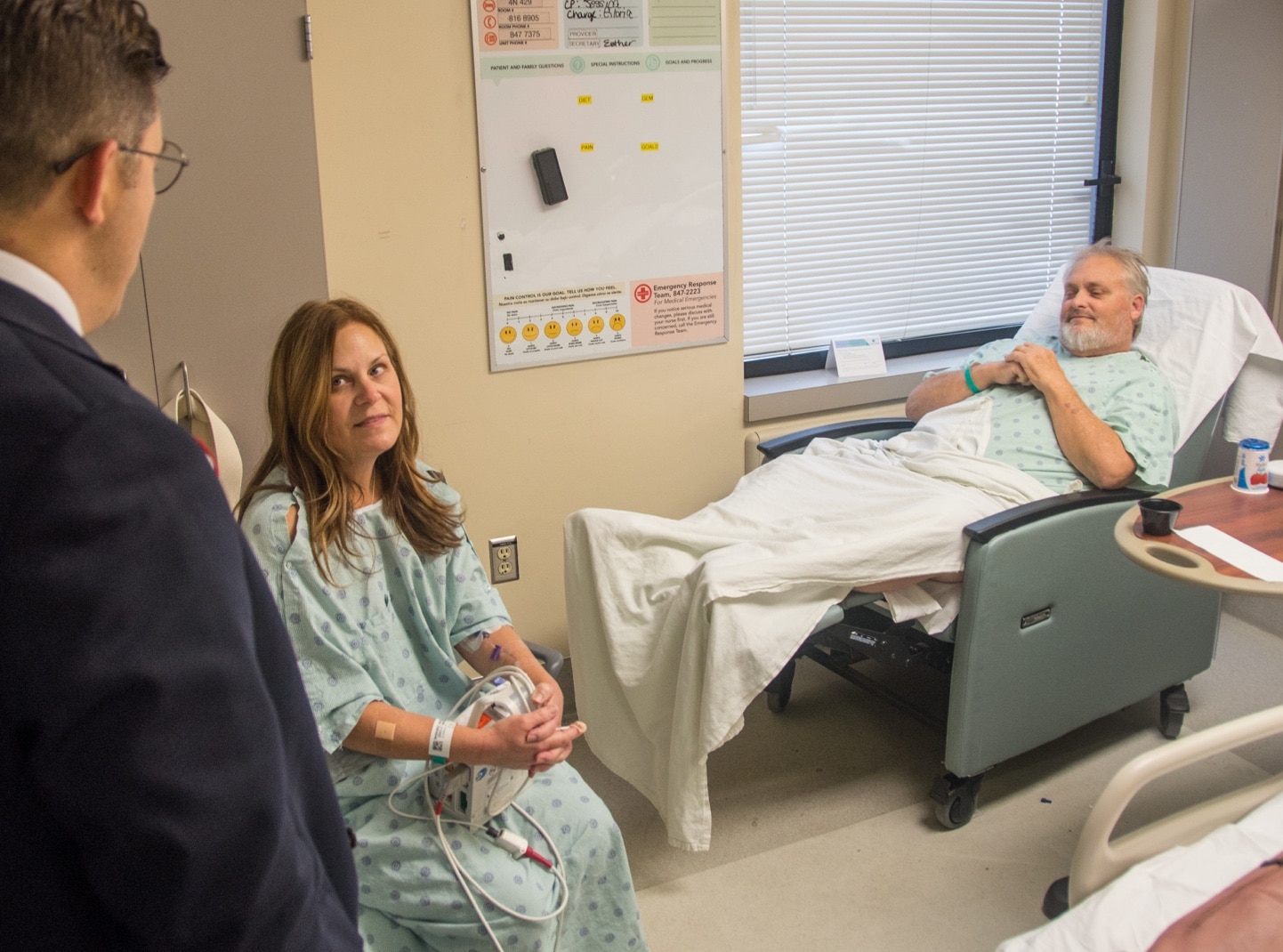
Often, organs used for transplant surgeries originate from another person’s death. Some organs and tissues, however, can be donated by someone who is living – a living donor transplant. ECU Health offers both deceased and living donor kidney transplants.
Your potential living donor might be a family member, friend or a Good Samaritan. Ideally, you and he/she have compatible blood types. If your potential donor is not compatible to donate to you, there is a process called paired exchange donation wherein your potential donor may match and donate to someone else in need, and the kidney you need is identified and assigned through a registry of matched possibilities. We are members of the National Kidney Registry.
Deceased Donor Transplant

The majority of transplanted kidneys and pancreas come from deceased organ donors – adults or children who have become critically ill and die as a result of their illness or injury.
Adults may have agreed to be an organ donor before becoming ill. Parents or spouses can also agree to donate a relative’s organs.
Organs for deceased donor transplants are sourced and matched by the United Network for Organ Sharing (UNOS). UNOS maintains waiting lists of people in need of organ transplants, exchanging data with hospitals across the country to ensure that all people on the waiting list are triaged fairly based on the severity of their illness and associated urgency of the need for transplantation.
Become a Kidney Donor

You can make a difference by joining over 50,000 living donors who have donated a kidney to people facing kidney failure, enabling them to live longer, healthier lives. There are different types of living kidney donation, including direct, paired exchange and Good Samaritan donations.
Becoming a living donor is not a decision to be made lightly, however. You want to fully consider how it may impact your physical and emotional health, as well as your family life and financial situation. Living donation involves significant invasive medical procedures after extensive evaluation with lab tests, a physical exam and a psychosocial exam to ensure your health status and an informed decision.
Individuals with a history of diabetes, kidney disease, some previous cancers, heart disease or liver disease cannot be considered as donors because of the potential health risks to themselves and the kidney recipient. Obesity and previous surgeries may also exclude a donor because of the increased surgical risk.
For more information or interest in becoming a donor, visit the National Kidney Registry.
Kidney Transplant FAQs
A kidney transplant is recommended for people who have end-stage kidney disease and will not be able to live without dialysis or a transplant. In the U.S., the most common cause of end-stage kidney disease are diabetes and high blood pressure. There are also many other causes of end-stage kidney disease. Always talk with your healthcare provider for a diagnosis.
Visit United Network for Organ Sharing (UNOS) for statistics of patients awaiting a kidney transplant, and the number of patients who underwent a transplant this year.
An extensive evaluation must be completed before you can be placed on the transplant list. Testing includes:
- Blood tests
- Diagnostic tests- such as cardiac tests and CT scans
- Psychological and social evaluation
Some of the tests you may already be familiar with, since they evaluate the health of your kidney and other organs. These tests may include:
- Blood chemistries. These may include serum creatinine, electrolytes (such as sodium and potassium), cholesterol, and liver function tests.
- Clotting studies, such as prothrombin time (PT) and partial thromboplastin time (PTT). Tests that measure the time it takes for blood to clot.Your blood type. Each person has a specific blood type: type A+, A-, B+, B-, AB+. AB-, O+, or O-. When receiving a transfusion, the blood received must be a compatible type with your own, or an allergic reaction will happen. The same allergic reaction will happen if the blood contained within a donor organ enters your body during a transplant. Allergic reactions can be avoided by matching the blood types of you and the donor.
- Human leukocyte antigens (HLA ) and panel reactive antibody (PRA). These tests help determine the likelihood of success of an organ transplant by checking for antibodies in your blood. Antibodies are made by the body’s immune system in reaction to a foreign substance, such as a blood transfusion or a virus. Antibodies in the bloodstream will try to attack transplanted organs. Therefore, people who receive a transplant will take medicines that decrease this immune response. The higher your PRA, the more likely that an organ will be rejected.
- Viral studies. These tests determine if you have viruses that may increase the likelihood of rejecting the donor organ, such as cytomegalovirus (CMV). Many other infectious diseases are also tested for, including HIV and hepatitis.
Diagnostic tests that are performed are necessary to understand your complete medical status. The following are some of the other tests that may be performed. Many of these tests are decided on an individual basis:
- Renal ultrasound. A noninvasive test in which a transducer is passed over the kidney producing sound waves that bounce off the kidney, transmitting a picture of the organ on a video screen. The test is used to determine the size and shape of the kidney, and to find a mass, kidney stone, cyst, or other obstruction or abnormalities.
- Intravenous pyelogram (IVP). A series of X-rays of the kidney, ureters, and bladder with the injection of a contrast dye into the vein to find tumors, abnormalities, kidney stones, or any obstructions.
The transplant team will consider all information from interviews, your medical history, physical exam, and diagnostic tests in determining whether you can be a candidate for kidney transplantation. After the evaluation has been completed, your transplant coordinator will present the results of your tests to the transplant team. The team will decide if you are an acceptable candidate for transplant and you will be placed on the United Network for Organ Sharing (UNOS) wait list, if additional testing is needed to make a decision or if you are not a candidate for transplant at this time. If you are deemed not a candidate, we will discuss with you if there is anything that you can do to become eligible for transplant at ECU Health.
Examples of reasons people are deemed not a candidate for transplant: (not inclusive)
- BMI greater than 42
- Non-adherence with dialysis treatments- skipping or ending treatments early
- Smoking when you have heart or lung problems, or diabetes
- Lack of Insurance Coverage
- Lack of social support
If you are receiving a kidney donated by a living donor, the donor will undergo a similar evaluation.
There is no definite answer to this question. If you have a compatible and healthy living donor, you may be able to get a transplant within a few weeks or months.
If no living-related donor is available, it may take months or years on the waiting list before a suitable donor organ is available. During this time, you will receive close follow-up with your healthcare providers and the transplant team. Various support groups are also available to assist you during this waiting time. Link to our support group.
When a kidney or pancreas becomes available for you, we will notify you by phone. It is VERY important that you answer your phone when contacted by the transplant center. If we are unable to reach you after approximately 20-30 minutes we may have to decline the organ. If you get a new phone number, are going out of town, or will be unavailable for an extended period of time, please let your coordinator know so that we can update your records. We will make every effort to reach you and will call any and all numbers you chose to provide us with during your evaluation.
Living with a transplant is a lifelong process. Medicines must be given that trick the immune system so it will not attack the transplanted organ. Other medicines must be given to prevent side effects of the antirejection medicines, such as infection. Frequent visits to and contact with the transplant team are essential. Knowing the signs of organ rejection and watching for them on a daily basis are critical.
Every person is different, and every transplant is different. The new antirejection medicines that are being approved are very exciting. Results improve continually as healthcare providers and scientists learn more about how the body deals with transplanted organs and search for ways to improve the success of transplantation.