“I love working together with my colleagues to ensure patients here in eastern North Carolina receive the best care possible – because all patients – no matter where, deserve the best care.”
The Brody School of Medicine at East Carolina University and ECU Health work together for a common mission, to improve the health and well-being of eastern North Carolina. Compared to the rest of North Carolina, patients in the 29-county region ECU Health serves experience greater systemic socioeconomic challenges, which have negative impacts on health outcomes, but team members across Brody School of Medicine and ECU Health are developing innovative solutions to ensure the best for patients and families.
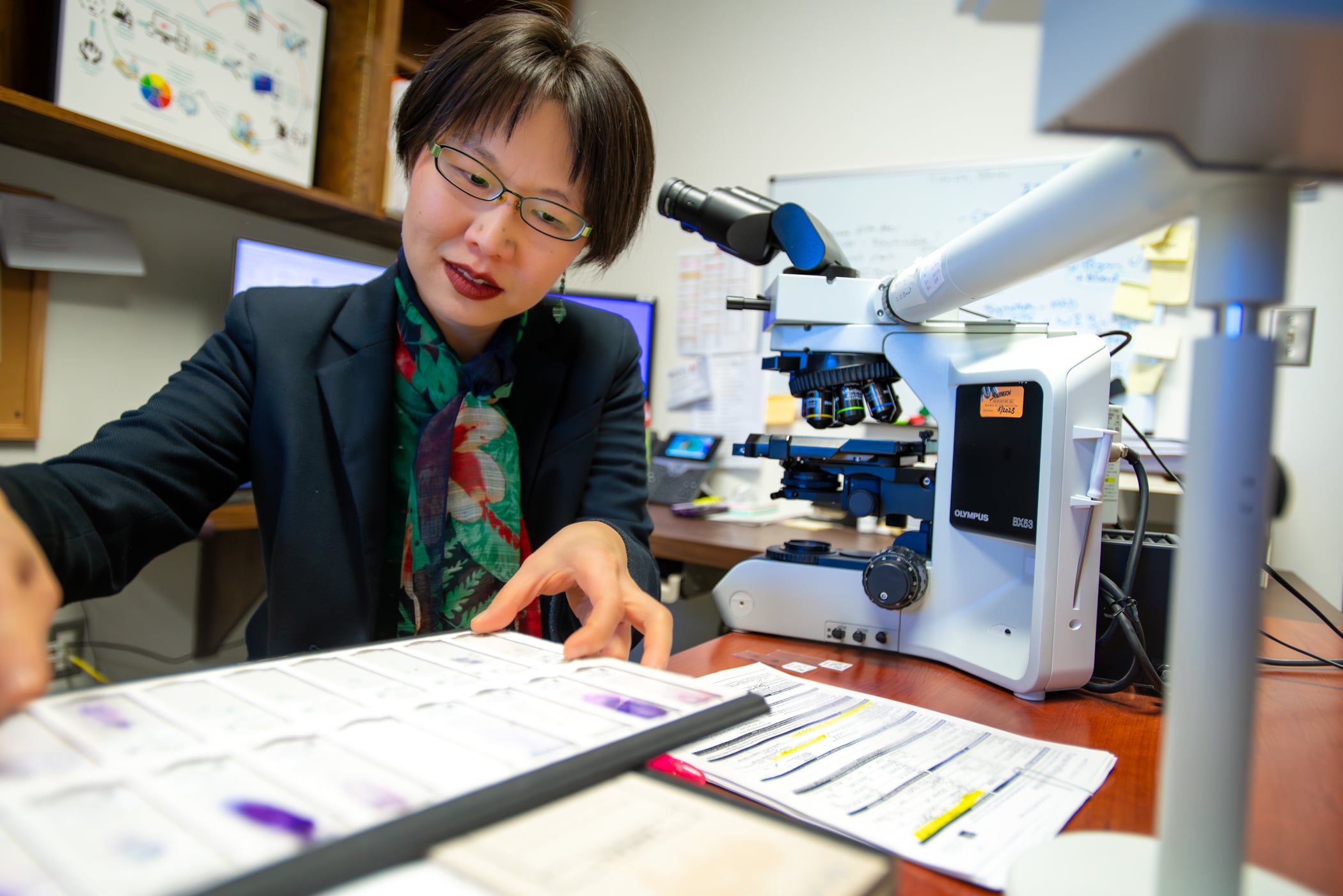
Dr. Yaolin Zhou, associate professor of pathology and laboratory medicine at Brody School of Medicine and head of molecular pathology at ECU Health, holds this mission close to her heart. She said her experience as a cancer patient inspired her personal mission of ensuring patients have the highest standard of care, no matter where they may live. Hear from Dr. Zhou below.
Dr. Zhou’s leadership and focus on quality improvement landed her on the 2023 Becker’s Hospital Review “Emerging Leaders: Provider Organization Leaders Under 40” list. Learn more here.
“I was born in communist China, and my parents survived the Cultural Revolution, which disrupted their education. Neither of my parents ever had a chance to complete middle school or high school. My dad came to the United States in the late 1980s because he was accepted into a doctoral program at the University of Texas at Austin. When I was four years-old, my mom and I joined him. In 1989, Tiananmen Square happened and my parents and I, with other Chinese graduate students, carpooled together to Houston to protest at the Chinese Consulate General against the injustice. My parents taught me to fight for what’s right and protect the vulnerable. That’s something I have carried with me all my life; it’s just how I was raised.
When it came time for college, I decided to go to Duke University, where I was selected as a Robertson Scholar and provided numerous leadership opportunities and funding for international service work. I was additionally attracted to Duke’s interdisciplinary public policy program because I knew that in order for me to become an effective physician, I would need to understand the context under which we practice medicine. My formal studies reinforced my belief that health care systems should be structured to ensure equitable access for all members of society.
As a senior student already accepted into medical school, I was diagnosed with cancer. My surgery was at Duke, and four months later, I started at Mayo Clinic School of Medicine. Recurrence occurred during my second year. My Mayo Clinic doctors referred me to MGH (Harvard) for further treatment. After graduating from Mayo Clinic, I continued to receive outstanding medical care at my residency and fellowship training institutions (University of Alabama at Birmingham and Cleveland Clinic). Although I was fortunate to receive top-notch medical care, I felt a sense of injustice for my patients who were not always as fortunate.
My research interest became: How do you ensure that all patients everywhere, despite differences in their culture, context, and resources, can access the same guideline-recommended standard of care? I received the best care possible, but everybody deserves to receive the best care. It shouldn’t matter if it’s me, or you, your child or your grandma.
By the time I met my current department chair, Dr. John T. Fallon, in early 2020, I had become somewhat of a national leader in molecular test utilization, which combines my love for molecular diagnostics and quality improvement.
Dr. Fallon was very intrigued by the work I was doing and I ended up formally applying for a faculty position at ECU. Then COVID hit so I couldn’t come and visit, but he gave me an offer that I was very interested in. In addition to several personal reasons, such as closer proximity to my family, Brody and ECU Health were particularly attractive because of its mission and underserved patient population. How do you reach the patients who are out in rural eastern North Carolina? To answer my burning question of how to provide the best care for all patients, regardless of culture, context and resources, I need to be on the ground. I can’t do that in the ivory tower. I need to be among the patients we are seeking to serve.
Because of COVID, I accepted this job sight unseen, bought a house sight unseen, and moved across the country because my dream had always been to treat the underserved.
Today, as a molecular pathologist and medical school professor, I spend my time performing clinical work, research, teaching, professional service, and administrative duties. I am the Director of Quality and Test Utilization, and Head of Molecular Pathology at ECU Health. My clinical service is often intertwined with research and teaching. I direct two different pathology residency rotations – the molecular rotation and the test utilization rotation. Test utilization addresses, ‘how do you decide what tests to order for your patients?’ As a molecular pathologist, I focus most of my attention on the pre-test and post-test steps of molecular testing. I love working together with my colleagues to ensure patients here in eastern North Carolina receive the best care possible – because all patients – no matter where, deserve the best care.”