John Core had never heard of pulmonary rehabilitation until he needed it.
“I went to urgent care with what I thought was a bad cold,” Core said. “But my heart was racing so they sent me to the hospital.”
Once in the ECU Health Medical Center emergency department, Core said they were unable to get his 144 beat-per-minute heart rate down with medications; the next step was to perform an electrical cardioversion, which is where the heart is shocked to restore a normal rhythm.
“I wound up in the ICU and stayed in the hospital for two weeks,” Core said. “When I got out, I had trouble breathing and had to be on oxygen, which I hated.”
After a six-week recovery, during which time Core said he could barely walk, his doctor recommended he try pulmonary rehabilitation.
“I was encouraged that my doctor thought I was strong enough to go,” Core said. Upon arriving, Core immediately felt comfortable in the rehab setting. “They were supportive and guiding. They were wonderfully attentive, and their sense of humor and generosity with their time made it the best experience I’ve ever had in health care.”
Pulmonary Rehabilitation helps reduce and control breathing difficulties and other symptoms of lung disease, including asthma, chronic obstructive pulmonary disease or pulmonary hypertension. ECU Health’s Pulmonary Rehabilitation team strives to help patients achieve their highest level of independence and physical ability.
Initially, Core could only walk one lap around the therapy track with the assistance of oxygen before needing a rest; but week by week, he increased his distance. He was impressed by the rehab team’s consistent regimen and organization.
“You had a set routine every visit: sign a form, get weighed, take your blood pressure and then start your program.” The planning and tracked improvement helped drive him to want to go to therapy his prescribed three times every week. “They made me like exercise, when I hated exercise before. I used to think exercise was a waste of heartbeats.”
Core was also impressed by the pulmonary rehab team’s rigorous standards and attention to detail.
“At first, I couldn’t go to the grocery store because I couldn’t walk the aisles,” Core said. “Then I got the idea that I could lean on the cart and put my oxygen tank in the cart. I was so proud of myself.”
The next day, Core said he told his rehab therapist what he’d done.
“She said, ‘That’s not good enough.’ At first that hurt my feelings, but she was right. It pushed me to walk longer and harder.” Any time Core showed signs of fatigue, he was made to rest so they could monitor his oxygen saturation, which should be above 90%. “When they saw I was throwing PVCs [premature ventricular contractions] during my walk, they stopped therapy until I was cleared by my cardiologist,” Core said.
PVCs are extra, abnormal heartbeats that disrupt a normal heart rhythm.
One day, Core asked the rehab team if he could try walking two laps without oxygen.
“They agreed but monitored me very closely. After my first lap, I was at 90-91% oxygen, thank the Lord.”
From there, Core worked his way up to 11 laps just prior to graduation. Now, Core said he is feeling better than he did before his stay in the hospital.
“After graduating from pulmonary rehab, I joined the ECU Health Wellness Center, and I really enjoy swimming. I’ve lost over 30 pounds, I exercise regularly and I’m overall trying to improve how I live my life. I like where I’m at,” he said.
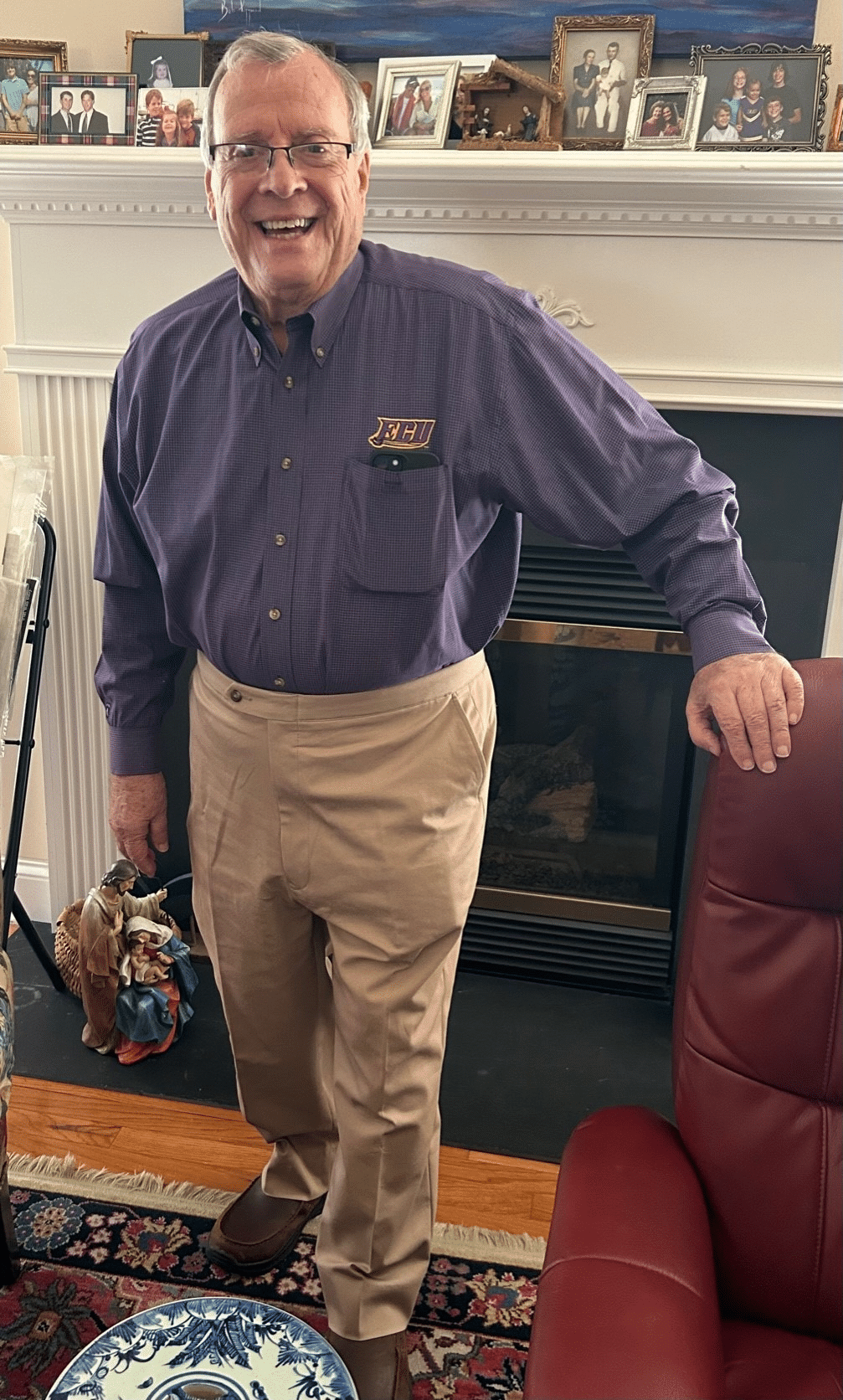
Core works at East Carolina University as a special assistant to the dean in the School of Dental Medicine, and he enjoys spending time with his wife of 32 years, his children and grandchildren. He’s also looking forward to a great grandchild on the way. This spring, he and his wife have plans to resume travel to visit his daughter and son-in-law in Charleston, South Carolina. Taking a trip like that wasn’t feasible prior to his experience with the amazing Pulmonary Rehab team.
“I had trouble walking; I couldn’t even walk a quarter of a mile,” Core said. “Pulmonary rehab helped me back. They know what they’re doing, and you can depend on them. To know that people care for you – it makes a difference. I can’t tell you how good they make you feel if you let them.”