Success stories start as dreams we harbor in our youth. Career days such as the third Future Health Professionals Conference Nov. 23 help fill in the critical details that make it believable.
Nearly 100 students from 11 counties in central and eastern North Carolina made the trip to Greenville and the Health Sciences Campus of East Carolina University for the event hosted by ECU Health and the university.
D.H. Conley senior Chance Frederick of Greenville was one such student, but one of only a handful who had taken part in the very same event last year.
“I was really amazed the first time by everything they offered me, especially the hands-on experience in the dental clinic. It really made me want to come back,” he said. “And just being able to network and meet people, to see these faces that I just know will be really beneficial for my future, I can’t get that anywhere else.”
Investing in the Future of Health Care
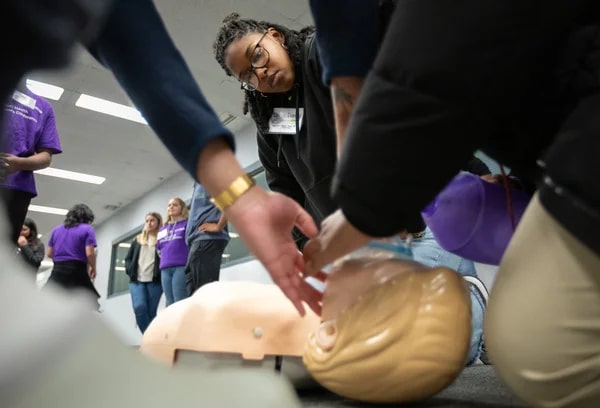
Students listened to medical professionals speak about their career arcs, then walked to nearby schools of medicine, dental medicine and nursing to tour facilities and experience hands-on curriculum at training stations and simulations.
“Engaging high school students early is crucial to addressing the national health care shortage, especially in rural areas like eastern North Carolina,” said Koai Martin, an equity and special projects consultant for ECU Health.
Both the health system and the medical school have a demonstrated history and mission of training and employing health care professionals to work in underserved areas of the state. Efforts such as the Future Health Professionals Conference help “create a pipeline of providers and health care professionals who understand the unique challenges of rural health care,” she said.
“Ultimately, it’s about investing in the future of health care while uplifting the region our ECU Health and ECU medical school proudly serve,” Martin said.
Several students from the Brody School of Medicine led hands-on life support demonstrations and Stop the Bleed simulations. Dr. Calvin Blocker, a resident physician at the school and ECU Health, discussed the epidemiology and pathophysiology of strokes and methods for detecting and identifying stroke symptoms that concluded with an interactive experience involving the examination of brain models and specimens to show areas commonly affected.
“The Future Health Professionals Conference gives high school students insight into the daily lives of our students and the responsibilities of practicing professionals,” said Milton Bond, who directs the medical school’s Pathways to Health Careers Program. “It is important for ECU to commit resources to support initiatives like this to invest in building the future health care workforce.”
In the Middle of the Journey
“I knew I wanted to be a dentist from about 10 years old, but I didn’t get to do anything like this, and no one in my family was in the medical or dental field,” said Dr. Scarlett Walston, a clinical assistant professor in the School of Dental Medicine. “I think it’s really cool just for them to be able just to explore. Maybe one of them falls in love with dentistry, and maybe we’ll see them in the application cycle in a few years.”

Walston said preparing for the DAT — the Dental Admissions Test — is something some committed students begin even in high school. Outreach such as the conference can give young students a shot of hope at a time when they might feel bewildered and disadvantaged navigating such a competitive track.
“Helping the next generation find their path is always important,” she said.
Jennifer Kovacs is a career nurse and health sciences high school teacher who brought eight students to the conference from Dare County. She says health care is a wide-ranging industry that employs trades and hourly workers alongside highly trained specialists.
“There are so many opportunities. If blood and sickness are too much, there’s a cubicle you can sit in and be by yourself and still contribute to health care,” Kovacs said. “There’s a microscope; be a researcher developing a new drug or running lab tests. You can sterilize surgical equipment — another surgery cannot begin until you’ve sterilized from the last one.”
Her students, she says, are weighing careers on several factors. Passion is one, but years spent in college and student debt factor into plans.
“Health care is not just doctors and nurses. It is other clinicians. It is secretaries. It is custodial, meal services, environmental services. And it is a family. … and therefore you can get students involved in any of those aspects,” she said.
Frederick, the 17-year-old senior, put his statistical chance of eventually becoming a dentist at the dizzying tip of the range, 99%.
“I’ve wanted to be a dentist ever since I was 3 years old,” he said. “That was the age of my first dental appointment. If I’ve been into it for 14 years at this point, I think I can take the next 14 to make it happen.”
And he expects to make this dream a reality right in his hometown, at East Carolina University.
“Today, I got to meet with a bunch of second- and third-year dental students. I got to walk right into the lab and immerse myself, and they made me feel included,” he said. “So even though I haven’t started, I saw what it was like to be in the middle of the journey, and it makes me feel like, you know what, I can really do this.”
Greenville, N.C. – Trish Baise, ECU Health chief nursing executive, was recently honored as one of Becker’s Hospital Review’s 2024 Chief Nursing Officers (CNOs) to know. Since stepping into the role in 2022, Baise has cultivated a dynamic nursing environment that drives innovations to enhance patient care quality and elevate patient experiences across eastern North Carolina.
“This recognition by Becker’s reflects the collective efforts of the incredible nurses across ECU Health, all of whom are dedicated to creating an environment where nurses and patients alike can thrive,” said Baise. “Together, we are driving innovative approaches in rural health care, committed to excellence in all we do and enhancing patient care across eastern North Carolina. I am honored that ECU Health has been recognized for this commitment.”
Tasked with addressing nurse staffing shortages, managing budgets and fostering growth opportunities for emerging nurses, the nursing leaders recognized by Becker’s play a crucial role in shaping the future of nursing.

Beyond leading nursing departments, CNOs drive innovative initiatives that uphold high patient care standards. Their roles demand a unique blend of clinical expertise and executive leadership. This list honors CNOs for their commitment to optimizing health care.
Baise has led efforts to establish a supportive environment where both nurses and patients can thrive. Under her leadership, ECU Health has achieved its third Magnet recognition, underscoring a commitment to nursing excellence. The Advancing Nursing Practice and Excellence (APEX) initiative has been foundational to this strategy, focusing on innovation, research and collaborative efforts to advance nursing in rural health care. Through partnerships with East Carolina University and local colleges, ECU Health also invests in the future of nursing, offering residency programs to equip new nurses with essential skills. This vision represents ECU Health’s dedication to defining a new standard for patient care and nursing excellence in eastern North Carolina.
“As the region’s largest health care provider and educator, ECU Health has a unique role in shaping community health, and Trish understands that our mission’s success depends on attracting the best providers, nurses and care teams to our health system,” said Dr. Michael Waldrum, CEO of ECU Health and Dean of the Brody School of Medicine at East Carolina University. “Trish’s dedication to service and our mission aligns with ECU Health’s work to build the model for rural academic health care. ECU Health is proud to lead the way in defining the future of nursing in our region.”
Resources
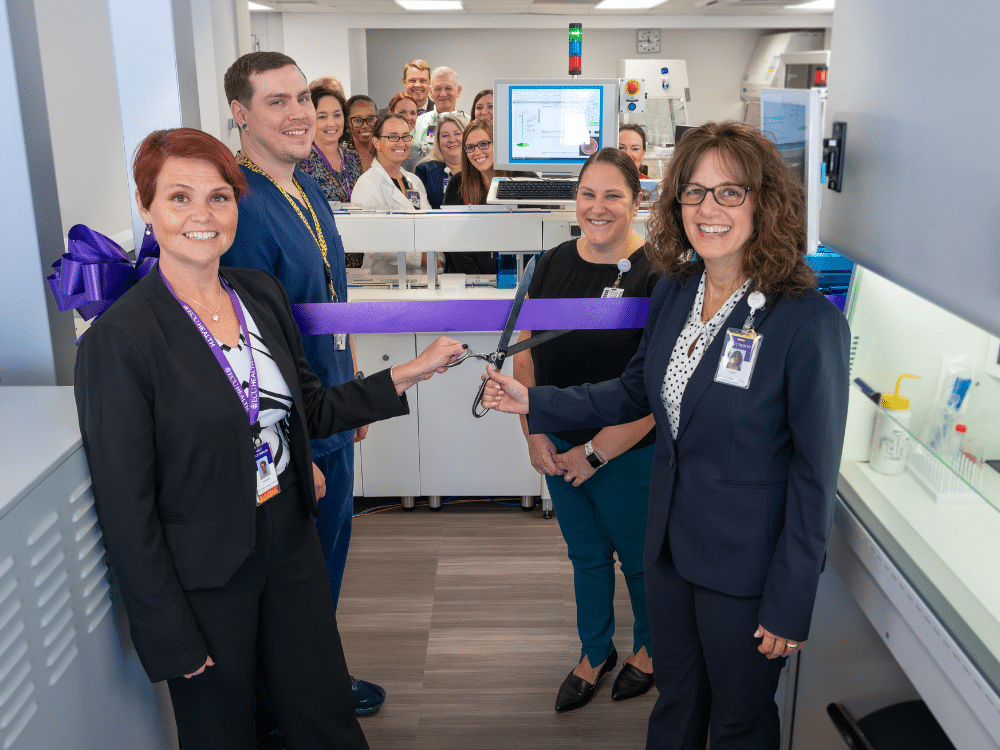
This year, the ECU Health Medical Center’s microbiology laboratory upgraded its technology by adding the BD Kiestra Total Lab Automation (TLA) system. The new equipment improves standardization in laboratory processes, enhances lab efficiency and centralizes microbiology testing. This automated solution to laboratory challenges represents ECU Health’s ongoing pursuit of innovation, efficiency and process improvement.
The Kiestra TLA system is an end-to-end automated lab culture workflow from plate labeling, inoculation, incubation, plate reading, imaging, reading and follow up work, to maximizing staff productivity. “Previously, after incubating cultures, you took the plates out and read each one from the oldest to the newest, but if the culture wasn’t robust enough, the plate had to go back in the incubator,” Caryl Havasy, the system administrator of laboratory service lines, said.
Heather Duncan, the director of ECU Health Medical Center’s laboratory services, further explained the challenge. “Think about incubating plates like baking a cake in the oven,” she said. “The whole time the plate is out of the incubator, it’s not growing the organism, just like a cake stops baking once you take it out of the oven. This can delay an organism’s growth and delay the test results.”
Furthermore, reading plates was subject to human experience and error. The Kiestra, Havasy and Duncan said, takes photos of the plates and uses AI algorithms to see an organism’s growth before the human eye can detect it. “This technology means there’s no variation in how the sample is applied to a plate” Duncan said. That means there’s no delay due to rework, and there’s less room for error.
Acquiring the technology was a four-year process, which included establishing a business case, investing funds, working through construction to get the microbiology lab space ready, installing equipment and training lab technicians. The lab opened officially this past July, and on Oct. 8, the team hosted an open house to celebrate the new technology with a ribbon cutting ceremony and tours for those interested in seeing the new equipment.
It was a great opportunity for Dr. Niti Armistead, the chief quality officer and chief clinical officer at ECU Health, to see the newest technology in action. “The Kiestra is an investment in our people, specifically our laboratory and microbiology team,” she shared. “These are highly trained professionals, and this technology takes away manual, inefficient tasks and allows them to use their skills and education to the fullest extent. This in turn drives improvement in safety with fewer manual errors, efficiency and professional fulfillment. It is another example of how we are advancing our vision to be the national model for rural health as it will be processing specimens from all of our hospitals.”
Jay Briley, the president of ECU Health Medical Center, also attended the event. “It’s exciting to see ECU Health continue to invest in cutting-edge technology like the Kiestra Total Lab Automation system. The system streamlines our processes, reduces manual errors, and allows our highly skilled lab professionals to focus on what matters the most: delivering timely, life-saving results,” he said. “The Kiestra TLA system is a testament to ECU Health’s commitment to innovation and the health and well-being of our patients.”
Andy Zukowski, ECU Health’s chief financial officer, highlighted the value of ECU Health’s investment in this new technology: “The Kiestra Total Lab Automation system represents significant innovation and value for ECU Health. By streamlining our microbiology lab’s processes, it enhances the patient experience and quality of care we provide all while improving throughout and cost savings. The long-term return on investment is clear, as it positions us to continue delivering innovative high-quality care while maintaining fiscal responsibility.”
Amy Campbell, PhD, RN, CPHQ, LSSBB, quality nurse specialist III, represented ECU Health on Sept. 25 at a side event held in parallel to the 79th session of the United Nations (UN) General Assembly in New York City. The meeting, titled “2030 Global Agenda for Sepsis for Attaining Sustainable Development Goals,” was convened as a collaborative effort of the Global Sepsis Alliance (GSA), Medical Women’s International Association, Sepsis Stiftung and UNITE Parliamentarians Network for Global Health.
The meeting was the first-ever global strategy spearheaded by the GSA, with collaboration from 70 partner and member organizations from Regional Sepsis Alliances across Africa, Asia-Pacific, the Caribbean, eastern Mediterranean, Europe, Latin America and North America. The meeting’s objectives were:
- To present the 2030 Global Agenda for Sepsis as the first multi-year global strategy to alleviate the significant human, societal, economic and health care burden of Sepsis.
- To reach consensus on the urgent need for reinvigorating the Sepsis responses at global, regional and national levels for the attainment of 2030 SDGs including the aspirations for Universal Health Care, Maternal, Neonatal and Child Health, AMR, Pandemic PPR, Gender Equality, Peace and Partnerships for Development.
- To discuss the critical role of health care workers, especially the medical women, representing over 70% of the health workforce globally, in the promotion and implementation of the 2030 Global Agenda for Sepsis.
- To call for establishment of a High-Level Political Platform for Sepsis to lead integration of this global health threat into the mainstream of health and development dialogue and architecture, including G7 and G20 Summits, World Health Assemblies, UN General Assemblies, and World Economic Forums.
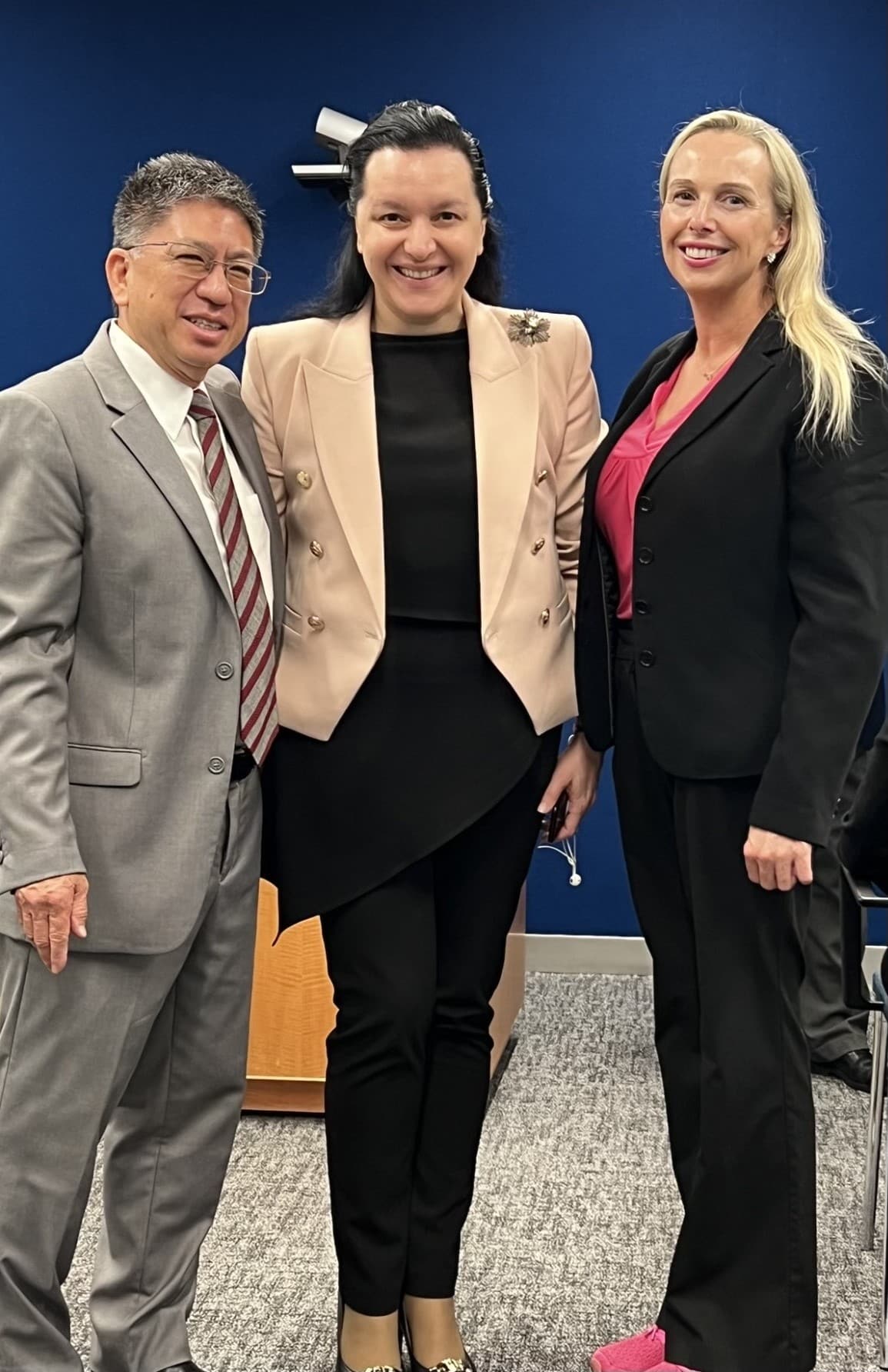
Dr. Campbell was personally invited to attend and speak by Dr. Mariam Jashi, MD, MPH, MPA and the CEO of the Global Sepsis Alliance, and Michael Wong, founder and executive director of the physician-patient alliance for health and safety. This invitation came as a follow-up to the 2024 World Sepsis Congress held this past April, during which Campbell served on the Scientific Committee. “I saw the invite and initially blew it off,” Dr. Campbell laughed. “I wasn’t sure it was real.” But after reassurance the invitation was legitimate, and with the encouragement of her team and Michael Wong, Dr. Campbell decided to go to New York. “I had a training session scheduled at work, but my colleagues covered for me,” she said. “I’m so thankful to my team and leaders who made it so I could attend.”
Once she arrived at the New York University campus, where the parallel session was held, Dr. Campbell said she met many leaders from across the world. “I met Dr. Eleanor Nwadinobi, the president of the Medical Women’s International Association (MWIA), Thomas Heymann, the president and CEO of the Sepsis Alliance and the Honorable Dr. Ricardo Baptista Leite, a member of the Portugese Parliament. People were speaking all these different languages and here I was from eastern North Carolina.”
The meeting focused on early detection of sepsis and how to treat patients with sepsis, no matter where they live. “As one of the speakers, I had the opportunity to emphasize the urgency of early detection, the critical need for continued research and the importance of securing funding so that everyone, regardless of their geographic location, can receive the same standard of care and chance for survival,” Dr. Campbell said. The speakers also discussed what they anticipated to be the next big problem with sepsis: antibiotic resistance.
Dr. Campbell said it was a great opportunity to represent the work she and ECU Health are doing to address the global problem of sepsis. “The attendees were impressed with the work we’re doing. ECU Health is a big deal; we have incredible people and talent, and we deserve a seat at the table,” she said. And next year, she has a seat waiting for her. “I’ve been invited back to speak next year, and I’ll work more with the GSA,” she shared. “We all have a lot to learn and do. Sepsis transcends borders, affecting individuals of all ages, races and socioeconomic backgrounds. However, the most vulnerable populations – children, the elderly and those in low-resource settings – are disproportionately impacted. Sepsis doesn’t wait, and neither can we.”
It was a packed house at ECU Health’s Monroe Conference Center on Oct. 1, as ECU Health and Pitt County Department of Social Services (DSS) welcomed dozens of community-based health partners for a conference designed to help tackle a complex challenge: reducing unnecessary emergency department utilization to ensure enhanced access for those needing emergency care.
It is no secret that overcrowding in emergency departments is a challenge facing hospitals across the country. ECU Health Medical Center, the only Level I Trauma Center in ECU Health’s 29 county service area, is no exception. The medical center serves a largely underserved rural region where access to care is difficult for many. That includes primary care, behavioral health care and other services best rendered in outpatient settings. Combined with a disproportionate number of uninsured community members, this lack of access to care means patients often times end up at hospital emergency departments.
Dr. Leigh Patterson, chief of services for emergency medicine at ECU Health Medical Center and chair of emergency medicine at the Brody School of Medicine at East Carolina University, said ECU Health’s nine hospitals will see nearly 250,000 visits to the emergency department this year, with more than half of those occurring at the medical center. She said conversations with key community health leaders, like the one hosted by ECU Health and Pitt County DSS, can help ensure community members are aware of, and have access to, non-emergent health care resources outside the emergency department setting.

“When I look at what happens inside the emergency department, I see the opportunity for us to help fill the care gaps that exist outside of it,” Dr. Patterson told the group, noting that she sees about 225 adult patients per day in the medical center ED, about 40% of whom could be more appropriately served in an outpatient setting. “When it comes to addressing this problem, it will take all of us as a health care community to make meaningful change. That’s why I’m heartened that so many of you have joined us today to work together toward solutions that make an impact in our community.”
The conference represented true regional community collaboration. Health care partners present at the conference included ECU Health, DSS Directors from across eastern North Carolina, Juvenile Justice, Trillium Health Services, Public School leaders, NC DHHS, payors and other eastern North Carolina hospitals and key stakeholders.

“The ECU Health/Pitt County DSS ED conference was an excellent example of cross system collaboration,” said conference co-sponsor Sharon Rochelle, director, Pitt County DSS. “This was a day to build mutually beneficial partnerships that have common goals to better serve the children and adults of the community.”
The conversation focused on both adult and pediatric/adolescent patient populations and heavily examined the challenges that behavioral health patients face accessing care. Despite the new inpatient behavioral health hospital slated to open in Greenville in 2025, those in attendance agreed that the issue needed immediate attention which involves creating increased interconnectedness among those providing care both in the community and in the hospital setting.
“We are grateful for all agencies involved in this important and challenging work,” said Jacob Parrish, vice president of capacity and throughput at ECU Health. “We know that the complex challenges we face cannot be solved at emergency departments alone. We are fortunate to have so many committed partners who share our vision for continuous improvement through strong relationships and close collaboration. Together, we can ensure the highest quality of care for communities across the East.”
The recent meeting was the first day of the two-day conference, largely centered around examining the issues through open and honest conversations. Those in attendance will reconvene later in the month for the second meeting to develop an action plan with concrete steps and strategies for improving access to care and reducing unnecessary ED utilization in eastern North Carolina.
“This is a complex set of issues, but I am confident we have the right people in our community committed to finding the solutions,” said Brian Floyd, ECU Health chief operating officer. “While these challenges are not exclusive to our health system or region, I know that together we can help support our emergency departments and improve the experience for those needing access to high-quality emergency care which is rendered at our hospitals every single day.”
Resources
Dr. James Speicher, a thoracic surgeon at ECU Health Medical Center and director of the Thoracic Surgery residency program, and his team are working to improve pain management in patients after their surgery.
After meeting with other thoracic surgeons outside of the ECU Health system and hearing a presentation on non-opioid pain management, Dr. Speicher knew it was something he wanted to bring to his thoracic surgery patients in eastern North Carolina.
“I said, ‘That’s a great idea.’ I came back from the meeting and said to the team, ‘Hey, let’s try to do this.’ It took us some time to get access to one of the medications we would use in the pain management protocol, but we started with our protocol multimodal pain management while avoiding narcotics in 2019.”
Dr. Speicher said the new pain management protocol includes a long-acting local anesthetic for nerve blocks, along with a muscle relaxer, nerve pain medication, acetaminophen and anti-inflammatories.

The goal of the program was to send fewer patients home with prescription narcotics while limiting the use of patient-controlled analgesia pumps for patients in the hospital after surgery.
As the team looked at surgical data from 2016-19 and compared it to the study, running from 2019 to today, he said the team found even better results than they were expecting.
“What we found with our study was we had really significant reductions in the uses of opioids. It was around an 85 to 90 percent reduction in our opioid use inpatient and around 60 percent of patients weren’t going home with any sort of narcotic prescriptions,” Dr. Speicher said. “The other thing that was really impressive to me in the study was that our average pain score was actually better for our patients on the non-narcotic protocol. We were reducing the use of narcotics on the floor, sending people home with less prescriptions and introducing fewer opioids into the community, all while actually doing a better job controlling their pain.”
The opioid-free pain management program is part of a larger enhanced recovery after surgery protocol, which Dr. Speicher and his team has been working on over the last few years. He said the team has put in place walking protocols and pre-operative carbohydrate loading along with other changes that have been shown to improve outcomes for patients.
This program is active for thoracic surgeries at ECU Health Medical Center.
“This is exciting work for us because we’re really focusing on helping make patients comfortable, controlling their pain post-surgery and getting them home more quickly,” Dr. Speicher said. “If we can do all of that without a narcotic prescription, that’s a really big win for the patients we serve and the community as a whole.”
When Dr. Tate Holbrook, a pediatric hematologist, founded the Comprehensive Sickle Cell Disease Program at East Carolina University in 1979, he was inspired by the need for basic health care services specifically designed to meet the unique needs of sickle cell patients.
Now, 45 years later, the program stands proudly as a leader in North Carolina at providing state-of-the-art medical care for those living with sickle cell disease, and its founder credits the annual Tate Holbrook Annual Sickle Cell Disease Update conference as a key component of that success.
“ECU has a reputation as being a hands-on, compassionate and people-centered organization,” said Dr. Holbrook, who the conference was named after following his retirement in 2022. “The care at ECU Health Medical Center is exceptional and it’s because of the people who really care. This conference is a big cooperative effort that brings like-minded people together such as researchers, pharmaceutical companies, and others who are helping create advancements in treatment for sickle cell patients.”

The Tate Holbrook Annual Sickle Cell Disease Update is hosted by East Carolina University’s Comprehensive Sickle Cell Program and the Department of Pediatrics Hematology/Oncology, in collaboration with Eastern AHEC. The goal of the conference is to bring together medical professionals and patients to bridge the gap of communication and to improve treatment for patients with sickle cell disease.
To meet this goal, professionals with knowledge and recognition in the sickle cell community discuss the latest advances in treatment of sickle cell disease, cutting edge research, established and new medications and therapies, as well as psychosocial interventions. Conference organizers aim to encourage further discussion between providers and patients to create an environment focused on patient needs.
The most recent conference was hosted at Eastern AHEC on Sept. 6 and brought together medical professionals with 25 patients and six community-based vendors together to learn in a collaborative environment and provide resources to those living with sickle cell disease.
“I’ve come to this conference every year since 2009 when I retired and moved down here,” said Stephanie King, 70, who lives with sickle cell disease. “I think people with the disease should come to these types of events because there’s so much to learn about sickle cell. I go places and I speak about my experience and I have young people that come up to me and say ‘Oh my gosh, you can live this long with sickle cell disease?’ and I always say ‘Yes!’ With medical enhancements and the resources available, we can make it to 70 and beyond.”
Patients like King are at the heart of the conference. The concept of collaborative comprehensive care helps provide state of the art medical care for patients, including education of families and health care providers, psychosocial support to patients, families and community groups, and access to new and innovative therapies. It also emphasizes a close working relationship with other agencies involved in the care of individuals with hemoglobinopathies, including medical centers, community-based sickle cell programs, and the NC Sickle Cell Syndrome Program.
The collaborative approach is what drives progress forward for those living with sickle cell disease, according to Dr. Beng Fuh, current program director of the Comprehensive Sickle Cell Disease Program at ECU.
“One of the most important parts of this conference is that it brings patients with sickle cell together with medical providers,” said Dr. Fuh. “We get to facilitate that exchange between patients and providers to learn how we can improve things and how we can get better. Sickle cell functions best when we take that collaborative approach. When we can hear from each other, we make our providers better and we improve understanding of the disease for patients. When we’re here together we gain a greater appreciation for the fact that we’re all on the same team.”
The Great 100 Nurses in North Carolina honors the nursing profession by recognizing nurses around the state for their commitment to excellence. The recipients are distinguished for their outstanding professional ability as well as their contributions to improving health care services in their communities. This year, 19 ECU Health nurses were recognized as honorees, including Dennis Campbell, II, Myra Thomson, Alex Gilbert, Gina Coldwell and Lou Ann Proctor.
Dennis Campbell, II
Although he is now the president of ECU Health Beaufort Hospital and the interim president at ECU Health North Hospital, Dennis Campbell, II began his career in 2004 as a nurse in the medical/surgical intensive care unit. Over time, he spent his early career in the emergency department, the burn center and the telemetry floor, and he was a staff nurse educator and a clinical educator for local nursing schools in his home state of Indiana.

However, a job opportunity brought him to eastern North Carolina, and he’s since navigated his way into quality leadership, corporate compliance, behavioral health and nursing leadership.
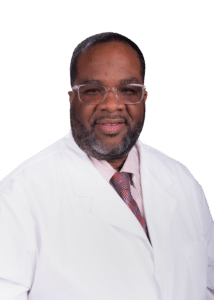 Dennis said finding his path to nursing was a winding road. “I was looking for something I could do that would provide a secure job,” he shared. “I shadowed a nurse in the local community as well as a respiratory therapist. What attracted me to nursing was how polished that nurse was. She was neatly dressed in white scrubs and a hat. The way she presented herself to her patients made me say, ‘I can do that.’” What kept Dennis coming back day after day was the difference he was making every day. “It’s the connection with people at the most vulnerable times of their lives,” he said. “I get to make the ordinary extraordinary, and if there’s something I can do to put a smile on your face, that also fills my cup.” That hasn’t changed since Dennis found his way into leadership roles. “It’s a platform that impacts healthcare and people in a larger way.”
Dennis said finding his path to nursing was a winding road. “I was looking for something I could do that would provide a secure job,” he shared. “I shadowed a nurse in the local community as well as a respiratory therapist. What attracted me to nursing was how polished that nurse was. She was neatly dressed in white scrubs and a hat. The way she presented herself to her patients made me say, ‘I can do that.’” What kept Dennis coming back day after day was the difference he was making every day. “It’s the connection with people at the most vulnerable times of their lives,” he said. “I get to make the ordinary extraordinary, and if there’s something I can do to put a smile on your face, that also fills my cup.” That hasn’t changed since Dennis found his way into leadership roles. “It’s a platform that impacts healthcare and people in a larger way.”
Still, Dennis was surprised that “little old me” was nominated for and selected as a Great 100 Nurse. “It says a lot about what my colleagues think about me, and I’m grateful,” he said. “And it’s good for all Great 100 nurses, because it’s often the case that we are the unsung heroes. It means people are taking notice and want to recognize those who give their heart and soul.” Dennis said the honor is also a legacy for his family. “They don’t get to go to work with me every day and see what I do, and my work is hard to quantify. To have that recognition is impactful to my family.”
Myra Thomson
 Myra Thomson, a nurse manager in the Medical Intensive Care Unit (MICU) and the Continuous Renal Replacement Therapy program at ECU Health Medical Center, decided to be a nurse because her mother was a nurse. “It was all I knew; I was raised in a medical profession home. It fit me and my personality,” Myra said.
Myra Thomson, a nurse manager in the Medical Intensive Care Unit (MICU) and the Continuous Renal Replacement Therapy program at ECU Health Medical Center, decided to be a nurse because her mother was a nurse. “It was all I knew; I was raised in a medical profession home. It fit me and my personality,” Myra said.
The East Carolina University graduate began her career with ECU Health right after graduation. During her clinical rotation on the medical intermediate unit, she had the opportunity to shadow in the MICU. This confirmed Myra’s conviction to work with the critically ill patient population. “I love that there’s a complexity, with more than one thing to treat,” Myra said. She also enjoys the MICU team. “It’s the place to be,” she said. “I love my team at work and outside of work. They call me if they need something, and I check in on them. They’re my people.”
Myra said it was amazing to find out she was named a Great 100 Nurse. “It’s an honor for me that the people I work with think enough of me to say what they did about me. It shows they’re exactly why I do what I do.” It’s also special that so many ECU Health nurses are recognized this year. “The nurses here work very hard across the system, and they deserve to be recognized. It makes you proud to work at ECU Health,” Myra said.
Alex Gilbert
 Alex Gilbert, a staff nurse III in the surgical intensive care unit (SICU), calls himself a “second generation nurse,” because both of his parents were also nurses. “Mom works in the ECU Health Cancer Center,” Alex said. “Dad was a flight nurse with EastCare. That’s how my parents met.”
Alex Gilbert, a staff nurse III in the surgical intensive care unit (SICU), calls himself a “second generation nurse,” because both of his parents were also nurses. “Mom works in the ECU Health Cancer Center,” Alex said. “Dad was a flight nurse with EastCare. That’s how my parents met.”
Alex used to watch his father on the helipad and wait for him to get off work, which sparked his own interest in a health care profession. That spark was reignited when his grandmother got sick during his senior year of high school. “That renewed my interest and showed me I could care for people. I knew I had a calling.”
After graduating from East Carolina University with his BSN, Alex split his time between the SICU and the ECU Health EastCare Transport Team as a flight RN. He also serves as an EMT-B in the community. Alex said he was surprised when he discovered he was a Great 100 Nurse honoree. “I can think of so many others who deserve this award,” he said. “We don’t do the job for recognition; we do what we do to care for people.” Alex did cite his passion for his work as a key factor in his success, as well as the support from his family and his co-workers. “It’s not just a nine to five job; it’s someone’s life. It’s an honor and a pleasure to care for someone. But I can’t take all the credit. My faith, my family and my co-workers all play a part. I’d put my team up against any in the country, and I wouldn’t be getting this award if not for them. I’m just a piece of the puzzle.”
ECU Health’s representation in the Great 100 Nurses is a testament to the care our nurses provide, and the education and support ECU Health provides its nurses, Alex said. “We’re the biggest level one trauma center East of I-95,” he said. “Our patients are the sickest of the sick, and our nurses are on the top of their game.”
Gina Coldwell
 A Newport News, Virginia, native, Gina Coldwell knew she had an interest in nursing early-on, but she couldn’t go to school while caring for her four small children. “I was a stay-at-home mom for 15 years,” she said. “But then I got divorced and was working two minimum-wage jobs and I wanted to do something I enjoyed.” That’s when Gina went back to school and received her associate degree in nursing from Edgecombe Community College in 2019. “I started working at ECU Health that following summer,” Gina said. She began on the Neuroscience Intermediate Unit, but she also continued her education to complete her BSN from East Carolina University in 2021, followed by enrolling in a master’s program at Carson Newman University, with plans to graduate in 2025.
A Newport News, Virginia, native, Gina Coldwell knew she had an interest in nursing early-on, but she couldn’t go to school while caring for her four small children. “I was a stay-at-home mom for 15 years,” she said. “But then I got divorced and was working two minimum-wage jobs and I wanted to do something I enjoyed.” That’s when Gina went back to school and received her associate degree in nursing from Edgecombe Community College in 2019. “I started working at ECU Health that following summer,” Gina said. She began on the Neuroscience Intermediate Unit, but she also continued her education to complete her BSN from East Carolina University in 2021, followed by enrolling in a master’s program at Carson Newman University, with plans to graduate in 2025.
Gina said she didn’t know what specialty she wanted after initially graduating from nursing school. For her, the team on 3 North drew her to the neuroscience unit. It was a challenging first year, but Gina said she has grown to love the challenge. “It’s hard to not take the work home with me,” she said. “But it’s so fascinating. You get such a diverse group of people, from someone who fell and broke their back to someone who had a stroke. It’s not an easy fix, but you have the benefit of seeing the fruits of your labor and how your patients improve. It’s so rewarding and fulfilling.”
That passion is one reason Gina was nominated for and recognized as a Great 100 Nurse. “I was shocked when I found out,” Gina said. “I was proud because I still consider myself a baby nurse. And we have amazing nurses at ECU Health. We’re a Level I Trauma hospital, and everything we deal with is big. You must have your heart in it, and you must have good leadership that recognizes that heart.” Gina also works with new graduates and new hires. “I love to teach and train,” she said. “And if I don’t know something, I ask someone who does. We’ll find out the answer together.”
Lou Ann Proctor
 Lou Ann Proctor, a staff nurse IV in the pediatric intensive care unit (PICU), calls herself a legacy Great 100 Nurse. “My mother, Janice Proctor, was in the first group selected to be a Great 100 Nurse in 1989, the year I graduated from nursing school at ECU,” Lou Ann said. “My Aunt Lucy Weaver and Aunt Becky Lewis were also chosen in 1994 and 1993. Sadly, I just lost my mother last year, and she would have loved this.”
Lou Ann Proctor, a staff nurse IV in the pediatric intensive care unit (PICU), calls herself a legacy Great 100 Nurse. “My mother, Janice Proctor, was in the first group selected to be a Great 100 Nurse in 1989, the year I graduated from nursing school at ECU,” Lou Ann said. “My Aunt Lucy Weaver and Aunt Becky Lewis were also chosen in 1994 and 1993. Sadly, I just lost my mother last year, and she would have loved this.”
It was her mother’s work that inspired Lou Ann to become a nurse in the first place. “My father was a farmer, so when I turned 15, I wanted to get out of the tobacco fields and I went to work with my mother at Edgecombe General Hospital in Tarboro. I got to work beside her and see how amazing she was at her job,” she said.
Lou Ann has continued that legacy by being nominated as a Great 100 Nurse several times before being an honoree this year, although she remains humble about the work she does every day. “I’ve been a bedside nurse for 35 years and have been involved in Nurse Congress, Quality/EBP Council and my unit council, but there are so many nurses I would nominate for this award. That recognition is overdue and well deserved for them.” When she found out she has won the award this year, the moment was bittersweet. “My co-workers nominated me this time and I was both thrilled and heartbroken to be selected,” she said. “It would have meant so much if my mother was still here. But my Aunt Lucy and family plan to attend the Gala with me and that will make it special.”
The recipients will be honored at a statewide gala in September, to be held in Concord.
Greenville, N.C. – The Eastern Carolina Injury Prevention Program (ECIPP) at ECU Health Medical Center was awarded the Safe States Injury and Violence Prevention Achievement Award at the Safe States 2024 Injury and Violence Prevention (IVP) Professionals Annual Conference in Portland, Oregon on Aug. 20-22. Safe States recognizes the outstanding achievements of members and partners annually through peer-nominated awards.
“We are incredibly proud of the recognition ECIPP’s initiatives have received,” said Sue Anne Pilgreen, manager, ECIPP, ECU Health. “This award highlights our team’s leadership and expertise in injury prevention and advancing safety practices locally and nationally. While this recognition is encouraging, what truly motivates the ECIPP team is getting to see the impact that this work has on the members of our community as we remain dedicated to promoting safety, encouraging healthy behaviors and reducing injuries.”
Established in 1995, ECIPP is a collaborative prevention focused health program at ECU Health Medical Center. Partnering with the ECU Health Trauma Center, the James and Connie Maynard Children’s Hospital and the Brody School of Medicine‘s Department of Emergency Medicine, ECIPP is dedicated to improving the health of eastern North Carolina by reducing the incidence and impact of injuries. The American College of Surgeons noted the value of ECIPP’s work in the verification of Maynard Children’s Hospital as a Level I Pediatric Trauma Center.
ECIPP has been instrumental in the development, implementation and interdisciplinary adoption of injury prevention practices for children and adults across eastern North Carolina. ECIPP offers a wide range of prevention programs aimed at addressing the most pressing injury concerns in the region. These programs include education on child safety, teen safe driving, hot car safety, firearm safety, suicide prevention, traffic safety and poison prevention. ECIPP also partners with Greenville Police Department on the Greenville Traffic Safety Task Force, which earned a national achievement award in 2023.
By building innovative partnerships, ECIPP has successfully promoted the adoption of injury prevention practices across various industries. For instance, the firearm safety program collaborates with wildlife organizations and pawn shops to provide education and gunlocks, while partnerships with Community Health Workers help deliver bike safety education and helmets. ECIPP also created an LGBTQ+ youth suicide prevention documentary that has been integrated into college curricula and hospital onboarding processes. From 2020 to 2023, ECIPP reached 86,333 individuals, distributing 2,405 gun locks, 256 medication lock boxes, 3,204 bike helmets and 259 child car seats.
“ECIPP’s strategies and partnerships have been crucial in expanding education and resource access in rural eastern North Carolina communities,” said Catherine Nelson, senior administrator of Community Health Programs, ECU Health. “This award is a testament to our commitment to injury prevention and the positive impact we’ve made for children and families across the region. By collaborating with local organizations and leveraging innovative approaches, we’ve been able to address critical issues, ultimately advancing the health and safety of our communities.”
To learn more about ECIPP, visit the webpage.
ECU Health Medical Center is excited to welcome the newest class of Project SEARCH students. The one-year internship program is designed for high school students with developmental and intellectual disabilities in their final year of their high school education. Through Project SEARCH, these students gain valuable real-world skills, enhancing their employability, confidence and independence.
The Project SEARCH Class of 2024 includes: Cameron McKenna, Daniel Sparrow, Keon Cox, Mariah Locklear, Kalasiah Forbes-Paige, Kenny Lucas, John Walker-Aytch and Nasir Gardner.
“We’re honored that ECU Health Medical Center continues to host Project SEARCH expanding educational opportunities for our students,” said Doris Hill, workforce development coordinator at ECU Health. “This program empowers students with essential job skills they can carry into their careers, while also enhancing diversity within our organization and the local workforce. We’re eager to witness the growth and new experiences our incoming students will gain throughout their journey with us.”

During the program, students participate in internships across various departments at ECU Health Medical Center, including in hospitality, cafeterias, housekeeping and some clinical spaces. These hands-on experiences help students transition from classroom learning to professional environments, bridging the gap between education and the workplace.
The employment rate for youth with disabilities is about 60 to 70 percent less than youth without disabilities, according to the Office of Disability Employment Policy. Project SEARCH has proven results with a 65 percent employment and 90 percent retention rate nationally. Students who participate in the program are enrolled at various Pitt County high schools.
The Project SEARCH program at ECU Health Medical Center began in 2015 through partnerships with Pitt County Schools, RHA Health Services and the North Carolina Division of Employment and Independence for People with Disabilities. The program has become a beacon of hope and opportunity for the students while also making significant contributions to the local community. Project SEARCH is instrumental in cultivating our ECU Health community into one that embraces diversity, inclusivity and shared success.

