While Heather Duncan, the director of ECU Health Medical Center’s laboratory services, knew she wanted to work in health care from an early age, her career plans changed when she learned about the medical technologist program at her school. “I thought I’d be a dermatologist,” she recalled. “But I liked biology and science, and the medical tech program fit my interests. That steered my career, and I’ve never looked back.” The South Carolina native has served in her current role at ECU Health for six years, and she is now wrapping up her four-year term with the Clinical Laboratory Improvement Advisory Committee (CLIAC), which is an appointed position. During her time with CLIAC, Duncan has been instrumental in bringing positive change to her profession.
CLIAC is a federal advisory committee that provides guidance to the Department of Health and Human Services (HHS) and is managed by the Centers for Disease Control and Prevention (CDC). The advice and guidance the committee provides pertains to general issues related to improvement in clinical laboratory quality and laboratory medicine practice.
Duncan said she didn’t even know CLIAC existed until a former co-worker approached her to gauge her interest in being nominated for a position. “They asked me if I would be interested, and it was exciting because CLIAC is so impactful.”
In the past four years, Duncan said she’s been privileged to collaborate with 20 other professionals to develop educational resources for the lab community and update the CLIA regulations. During her tenure, Duncan chaired the CLIAC Certificate of Waiver (CoW) and Provider-performed Microscopy (PPM) Procedures workgroups.

“The work that has come out of those groups has allowed CLIAC to make recommendations to modernize our regulations, which impact the laboratory community at large. We’ll see those impacts here at ECU Health,” Duncan said.
One such regulation restricts who is allowed to train new personnel to perform certain functions in the lab. With Duncan’s work, the regulation has now expanded to allow more people in the lab community to perform that training. “Because there is such a workforce shortage with laboratory technicians, this is impactful by expanding who can provide training, and it improves the overall quality of lab testing,” Duncan said. Caryl Havasy, the system administrator for laboratory services, sees Duncan’s work with CLIAC as instrumental in gaining more lab technicians. “ECU Health, like other health systems, faces an ongoing shortage of laboratory testing personnel. Heather’s experience in laboratory operations and regulatory compliance in our rural-focused health system brings a much-needed perspective to the work of CLIAC, specifically its role in creating the regulatory structure that defines the qualifications for frontline laboratory roles,” Havasy said.
Another exciting recommendation that emerged from the most recent CLIAC meeting would allow for virtual competencies, which would expand training capability and incorporate cutting edge technology into practice. “Because we serve rural communities, having this technology would cover a huge network,” Duncan shared. “We have benefitted from having a direct pipeline to the work CLIAC is doing. For example, our lab was one of the initial beta testers for virtual lab safety training. They sent us four Oculus headsets and they push new training programs to us.”
While this technology isn’t widely used yet, Duncan said being a part of an organization that promotes advancements in technology and makes recommendations on a federal level is gratifying. “This work allows for a forward-thinking process, and it will impact our whole community,” she said. “Our vision is to be the national model for rural health care, so we should use every tool available. Being a part of CLIAC means I’ve been able to make a real difference.”
Havasy highlighted other areas CLIAC and Duncan’s work with the committee makes an impact, including, “a change to rules surrounding histocompatibility testing (performed to match organ donors with recipients, i.e., kidney transplants) that will remove specific requirements for obsolete methods and practices, accept newer testing techniques and eliminate redundant requirements. This will result in a decreased compliance burden on the laboratory and more efficient testing for our eastern NC kidney transplant patients.” Duncan also worked with the CoW workgroup, which addresses regulations as they pertain to labs with a Certificate of Waiver. This waiver is granted to labs that only perform waived tests, which are simple laboratory procedures and examinations with a low risk of an incorrect result (including urine pregnancy tests or blood glucose monitoring). Labs must pay certification fees every two years to acquire and maintain the certificate. Duncan explained that one area her workgroup focused on was an updated fee schedule. “CLIA is a self-funded program, and they haven’t updated their fees in a long time,” Duncan explained. The group also worked on establishing a broader range of sanctions for laboratories that operate under a Certificate of Waiver but are not compliant with the CLIA regulations.
Because of her work with CLIAC, Duncan said ECU Health has a seat at the table and can provide input for advancements in laboratory operations. “Through these efforts,” Havasy added, “Heather embodies the ECU Health vision of bringing our rural health care system needs and potential solutions to a national stage, impacting not only our own operations but those of every health care system across the country.”
Greenville, N.C. – ECU Health and the national nonprofit Undue Medical Debt are pleased to announce an initiative that will help eliminate more than $186 million worth of past-due hospital medical debt for more than 32,000 qualifying patients. Debt relief letters will arrive over the course of December’s holiday season into the New Year on a rolling basis given the size of this relief effort
Eligible community members do not need to apply, and there is no application process. Instead, community members who qualify for this one-time debt relief will receive a branded letter from Undue Medical Debt indicating which past-due hospital debt or debts have been eliminated. Undue Medical Debt works with hospital systems and other providers across the country to purchase past due medical debt belonging to those least able to pay in large portfolios for pennies or less on the dollar and then erases the debt.

ECU Health’s collaboration with Undue Medical Debt pre-dates North Carolina Department of Health and Human Services’ medical debt relief initiative which spans all hospitals in the state and lays out a plan for medical debt relief coupled with changes to Medicaid/Medicare reimbursement policy and financial aid standards in 2025.
Under Undue Medical Debt guidelines, those who qualify for this medical debt relief have hospital medical debts that are 5% or more than their annual income or earn at or below four times poverty-level income. The current federal poverty level is an annual income of under $31,200 for a family of four which means a qualifying family of four would make under $124,800. Community members do not need to take any action, as the eligible hospital medical debt will automatically be eliminated for those who qualify.
“We’re grateful to collaborate with ECU Health to help ease the burden of medical debt in eastern North Carolina,” said Undue Medical Debt CEO and President Allison Sesso. “Helping community members burdened by medical debt takes thoughtful collaboration and I’m proud of the results: over 30,000 people helped this holiday season. We hope this program provides financial and emotional relief to recipients and encourages them to continue engaging with the healthcare system.”
The collaboration with Undue Medical Debt is one of many ways in which ECU Health is living its mission to improve the health and well-being of eastern North Carolina. The initiative aligns with the health system’s commitment to serving underserved communities in the East, many of which have disproportionate numbers of low-income and uninsured or underinsured people. The initiative is also in alignment with ECU Health’s long-standing practice of non-predatory billing practices, which emphasize charity care, zero-interest payment plans, transparent pricing and dedicated resources to help patients navigate financial requirements.
“At ECU Health, our commitment to our mission and patients is at the heart of all we do,” said ECU Health Chief Operating Officer Brian Floyd. “We have always been guided by a deep desire to support our patients in whatever way we can, and this collaboration with Undue Medical Debt will make an enormous impact on so many in our largely underserved region. We could not be more thankful to find an organization like Undue Medical Debt which shares our vision for making high-quality rural health care accessible here in eastern North Carolina.”
Greenville, N.C. – ECU Health, eastern North Carolina’s leading academic health care system, has named Todd Hickey, MHA, FACHE, as president of ECU Health North Hospital, effective Jan. 1, 2025. Hickey will serve as president of ECU Health North in addition to continuing his current role as chief strategy officer for the health system.

“I could not be more pleased to welcome Todd into his new role as president of ECU Health North Hospital,” said D. Van Smith, MBA, MSHA, ECU Health Community Hospitals President. “Todd brings more than 20 years of experience in health care operations, strategic planning and leading transformational change to the role, and I am confident he will continue to guide ECU Health North Hospital in service to communities in the northeastern part of our region. I want to also thank Dennis Campbell for his leadership as the interim president at North over the last six months.”
Hickey joined ECU Health in 2008, serving in service line and hospital operations executive leadership roles at ECU Health Medical Center until becoming the health system’s first Chief Clinical Network Development Officer in 2016. In this role, Hickey successfully led and implemented joint ventures, service line expansions, an integrated population health model and key acquisitions, including the integration of Halifax Memorial (now ECU Health North Hospital) into ECU Health in 2019. He transitioned to Chief Strategy Officer in 2022 which expanded his oversight to include developing and guiding the ECU Health enterprise 3–5-year strategic plan.
“It is an honor to serve as president of ECU Health North Hospital,” Hickey said. “I am fortunate to have had the opportunity to help bring ECU Health North into the ECU Health system and I have a deep appreciation for the important role it plays in Halifax County, Roanoke Rapids and the surrounding communities. I am excited to work with the ECU Health North team to continue advancing the legacy of providing high-quality, compassionate care.”
In recognition of the one-year anniversary of Medicaid expansion in North Carolina, Gov. Roy Cooper visited ECU Health Medical Center in Greenville to reflect on the impact of expansion and celebrate a year of reaching North Carolinians in need.
Since Medicaid expansion officially launched in North Carolina on Dec. 1, 2023, more than 80,000 eastern North Carolinians and nearly 600,000 people statewide have benefited from access to vital health insurance. Along with Medicaid expansion, the state also passed the Healthcare Access and Stabilization Program (HASP), which provides critical relief to rural hospitals.
Gov. Cooper said Medicaid expansion’s reach in rural communities, like ECU Health’s 29-county service area, has been especially impactful in the last year.
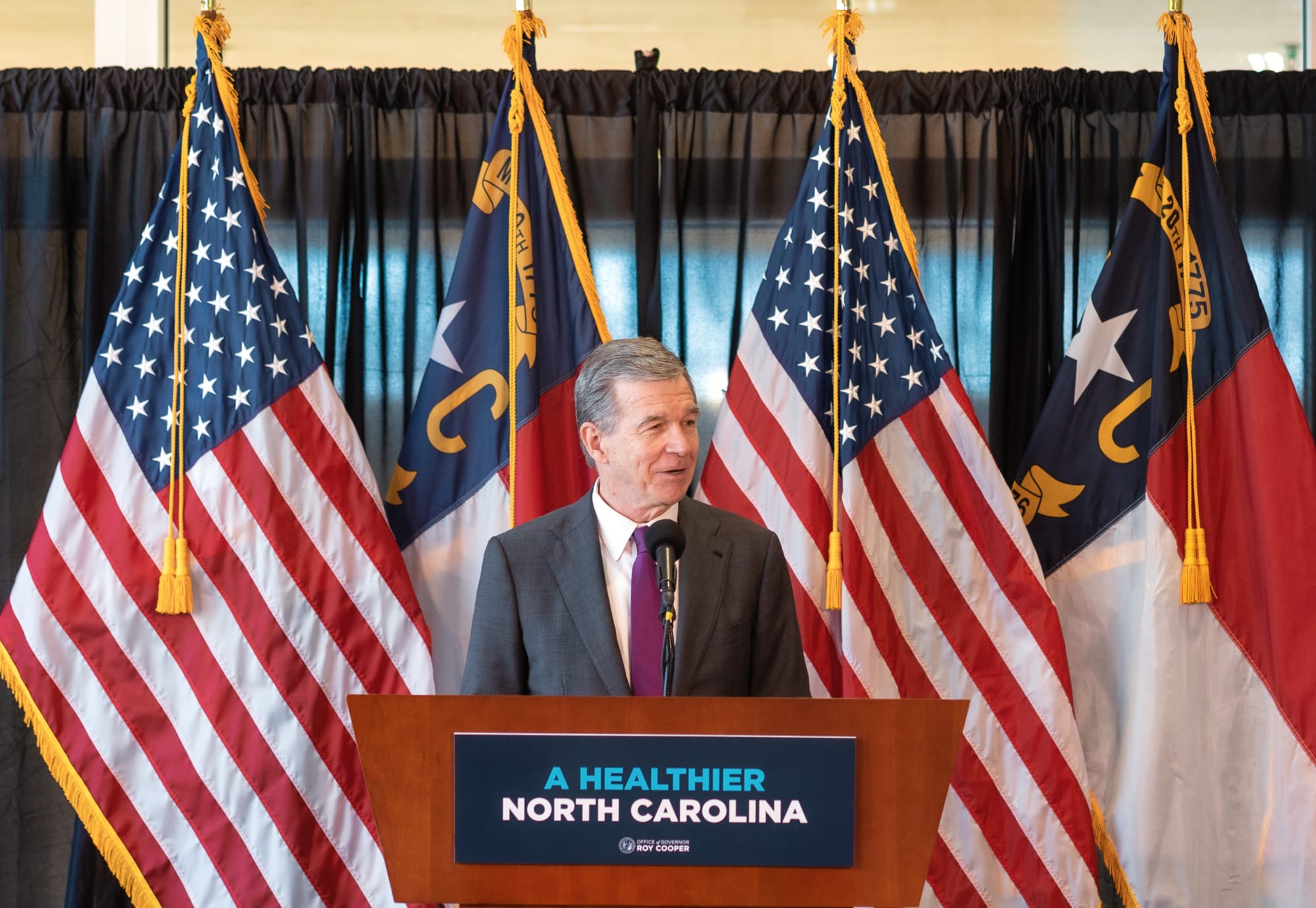
“The last year showed us that this is something that people desperately needed, particularly here in rural North Carolina,” Gov. Cooper said. “I grew up in Nashville and we know that rural North Carolinians have been helped more by Medicaid expansion than anyone else. I hold close to my heart the mission of getting people healthier. I knew getting Medicaid expansion passed and signed into law was the most important thing we could do to accomplish that.”

This milestone reflects the culmination of more than six years of advocacy by ECU Health, driven by the challenges faced by uninsured and underinsured patients.
Dr. Michael Waldrum, ECU Health chief executive officer and dean of the Brody School of Medicine at East Carolina University, said Medicaid expansion and HASP funding is creating real differences for patients, health care workers and the future of health care in places like eastern North Carolina.
“Medicaid expansion has helped improve access to primary care, empowering people to take control of their health and their lives,” Dr. Waldrum said. “It is also an investment in rural health organizations like ours. At the same time and in partnership with the state, ECU Health and the Brody School of Medicine are also committed to doing their part to support primary care expansion efforts in rural health care.”
He highlighted the expansion of the Rural Family Medicine Residency program, which will train nine rural residents per class across three training sites in the East and the upcoming Center for Medical Education Building on Brody’s campus. This investment has helped and will continue to help ECU Health and Brody serve the combined mission of improving the health and well-being of eastern North Carolina.
Dr. Karen Coward, a family medicine physician with ECU Health, is a Kinston native and practices in Tarboro. She said she knew by age 10 she wanted to be a family physician in her home community. She attended Brody and stayed true to her dream of serving eastern North Carolina.
She said before Medicaid expansion, many of her patients would rely on the emergency department for care. Even if a patient was connected with primary care, it was difficult for them to follow through with appointments or afford medications. Chronic conditions like diabetes, hypertension or even cancer would go unchecked. Now, she said, she’s seen a life-changing shift.
“Patients who once cycled through the emergency department are now establishing relationships with primary care providers like me,” Dr. Coward said. “They are keeping their appointments, following through on recommendations, treatments, and gaining access to medications and specialist referrals that were previously out of reach. For many, this will mean earlier diagnoses and interventions, reducing the burden of advanced diseases.”
Kody Kinsley, secretary of the North Carolina Department of Health and Human Services, joined the event and said that in the past year over $58 million in dental claims alone were filed, millions of prescriptions were filled and hundreds of millions of dollars in claims supporting hospital care were taken care of through Medicaid expansion.
He said this comprehensive health insurance is already making a real difference for individuals and families.
“Medicaid expansion is life changing for families,” Sec. Kinsley said. “It is peace of mind for people as they sit up late at night thinking about how the next day will impact them. Will a sickness impact their family? Will they end up in debt? They don’t have to worry about that anymore.”

The event also included remarks from a Medicaid expansion beneficiary, Darcy Guill from Ayden, who shared her gratefulness for regular care she’s receiving, specialists she’s able to visit and prescriptions she can fill, thanks to Medicaid expansion.
As we look back over the previous year, we’re proud to build the national model for rural health care here in eastern North Carolina at ECU Health and we’re grateful for the support the region and health system through Medicaid expansion and HASP.
Leaders from East Carolina University, Brody School of Medicine, ECU Health and across North Carolina came together for the Center for Medical Education Building groundbreaking on Brody’s campus.
The groundbreaking marked a new era for health care in eastern North Carolina and for rural communities across the state. With the new 195,000-square-foot, seven-story building set to be fully constructed in 2027, the incoming class sizes at Brody are expected to increase significantly – from fewer than 100 this fall to more than 120 by 2027.
“With this building, the state of North Carolina is affirming that rural medical education and health care matters, and that Brody has lived its mission and can solve these complex issues that rural health care faces,” said Dr. Michael Waldrum, chief executive officer of ECU Health and dean of Brody. “Rural health care is in crisis in America, and we are working to create the model for rural health care.

We are leaning into those issues and solving those systematic problems. This facility is emblematic of that work as we train the future physicians for this region and the state.”
The building, Dr. Waldrum said, is designed to fit the unique mission of Brody while providing state-of-the-art technology and amenities to attract and develop the best physicians in the East and North Carolina.
Dr. Jason Higginson, chief health officer at ECU Health and executive dean of Brody, said during the event that the nearly 200 attendees showed how grateful the community is to see support for Brody and the region.
“This is one of the biggest investments in eastern North Carolina,” Dr. Higginson said. “The Brody School of Medicine is here for the community and to see that support in return has been amazing. The school has a nearly 50-year history of developing physicians for eastern North Carolina, and we plan on continuing that. This facility is a great step in how we’re working to meet the needs of this region and state.”

Speakers also included ECU Chancellor Philip Rogers, University of North Carolina System President Peter Hans and fourth-year Brody student Shantell McLaggan.
The future-Dr. McLaggan spoke to the family atmosphere cultivated at Brody and how excited she is for future students to experience it inside a new facility, offering the very best tools for students to succeed.
Dr. Michael Lang, chair of the Department of Psychiatry & Behavioral Health at the Brody School of Medicine and ECU Health, is a Brody graduate himself and was born and raised in eastern North Carolina. He said he’s proud to be a part of Brody and the health system and believes the investment will benefit eastern North Carolina and rural areas and expand upon the decades of success the school has experienced.
“What I’m hoping is that we’ll be able to provide an even better pipeline to get physicians into these rural communities,” Dr. Lang said. “The small towns of eastern North Carolina, just like small towns everywhere, are desperately missing doctors. What I’m hoping is, as we expand the class, we will be putting more doctors of all sorts of specialties into those rural areas.”
The new Center for Medical Education Building also serves as a promise to the East and a commitment to the shared mission of Brody and ECU Health to improve the health and well-being of eastern North Carolina.
“These beautiful rural communities that we talk about are so important to the fabric of North Carolina,” Dr. Waldrum said. “They are dependent on us to come up with the model for rural health care, to deliver care and educate the future doctors. I’m so excited to celebrate that with you today as we put a shovel in the ground and mark this historic step forward.”
Resources
Rural Health Day at ECU Health
More information on the Center for Medical Education Building
Robert J. Greczyn, Jr., chair, ECU Health Board of Directors, recently received the 2024 Trustees Award for Distinction from the East Carolina University Board of Trustees in honor of his extraordinary leadership and service. This prestigious award recognizes individuals who embody excellence, innovation, and an unwavering commitment to advancing ECU’s mission of student success, public service, and regional transformation.
“I am deeply honored to receive the 2024 Trustees Award for Distinction,” said Greczyn. “East Carolina University and ECU Health have been central to my journey of service, and I am grateful to have played a part in advancing the collective mission to improve lives across our region.”
The Trustees Award for Distinction is reserved for leaders who inspire, influence and motivate others toward achieving shared goals. Honorees demonstrate a profound dedication to ECU’s strategic vision through championing partnerships, fostering philanthropy, and promoting public service—all while exemplifying strong character and professionalism.

Greczyn’s devotion to ECU runs deep. As a former member and chair of the ECU Board of Trustees from 2003 to 2011, Greczyn has continuously worked to elevate the university. Currently, he serves as chair of the ECU Health Board of Directors, where his extensive health care experience has been pivotal in integrating the health system with the Brody School of Medicine.
“Bob’s passion for serving the underserved and addressing complex health care challenges has been a guiding light for ECU Health,” said Dr. Michael Waldrum, chief executive officer of ECU Health and dean of the Brody School of Medicine at East Carolina University. “Through his leadership, the organization has stayed true to its mission-driven focus on improving the health and well-being across eastern North Carolina.”
Greczyn has been a prominent leader in North Carolina’s health care landscape for over three decades. Professionally, he served as the president and CEO of Blue Cross and Blue Shield of North Carolina from 2000 to 2010.
He also served as president and CEO of Healthsource Health Plans Inc. Greczyn also established a Rural Health Center in Anson County. His expertise running both not-for-profit and for-profit entities is supported by a leadership style that emphasizes enterprise risk, compliance, ethics and governance standards.
“As a member of our board, Bob has always advocated for patients, their families, team members, students, educators and especially those in underserved communities who struggle to gain access high-quality care,” said Dr. Waldrum. “His focus has always been on how we can make the greatest impact for our region. I am grateful to have the privilege to serve alongside so many mission-driven individuals like Bob who dedicate themselves to advancing this beautiful part of our state.”
Greczyn’s influence extends far beyond professional achievements; his commitment to serving underserved communities, championing collaboration, and driving positive change underscores his dedication to the mission of ECU. Greczyn’s recognition through the Trustees Award for Distinction is a testament to his enduring impact on ECU, ECU Health and the communities we serve.
Seven key priorities served as the central discussion point as community-based health partners joined ECU Health and Pitt County Department of Social Services (DSS) in October for the second session of a conference series designed to support the emergency department and improve access to non-emergent care across eastern North Carolina.
The seven key priorities, identified during the first conference session in early October, represent the unique viewpoints from stakeholders across the community and all of whom share a common goal: reduce unnecessary utilization of the emergency department in Greenville.
The seven priorities include:
- Placement/disposition – getting patients placed in the appropriate care settings outside the emergency department such as skilled nursing facilities, in-home care, adult care homes, foster homes, etc.

- Navigating the system – defining roles and responsibilities of each agency
- Collaboration – improve collaboration among systems and across agencies
- Crisis system – more clearly defining how the system operates and clarifying any confusion that may exist
- Community options and wraparound support – ensure a robust support system in the health care setting and in the community to ensure people get the help they need
- Access to services – provide clarity on where patients need to go to access care
- Regulatory – reduce barriers and create efficiencies in key operational areas like timely discharge and clinical assessments
“This was a moment for us as a health care community to not only clearly define the challenges facing the patients we serve, but to also explore how we can implement solutions that improve the emergency care realities here in eastern North Carolina,” said Jacob Parrish, vice president of capacity and throughput at ECU Health, who served as one of the conference organizers. “The challenges facing emergency departments both locally and nationally cannot be solved solely by the hospitals themselves. These conversations help us take our words and put them into collaborative action.”
Health care and community partners in attendance at the conference included ECU Health, DSS Directors from across eastern North Carolina, Juvenile Justice, Trillium Health Services, Public School leaders, NC DHHS, payors, faith leaders, and other eastern North Carolina hospitals and key stakeholders. The conversation focused on both adult and pediatric/adolescent patient populations who present at the emergency department but could be better served in a different setting.
The importance of education and outreach served as a common theme throughout the discussion. Organizations talked not only about the importance of providing critical information directly to patients, but also emphasized the importance of educating themselves on the role that other organizations and agencies play in the care continuum.

ECU Health highlighted the growing demand for emergency department services and the urgent need to streamline care in the community for non-emergent cases. The discussions underscored how patients with non-critical issues are often funneled to emergency departments due to limited access to routine and primary care resources and crisis services, creating unnecessary strain on EDs. ECU Health Medical Center, for example, remaining full nearly half the year due to high patient volumes, which often exceed its 974-bed capacity. This backlog directly impacts how long some patients may wait in the ED.
“Our commitment to improving emergency care access and efficiency for our patients is unwavering,” said Dr. Leigh Patterson, chief of services for emergency medicine at ECU Health Medical Center. “The collaboration we’re seeing across health care and alongside our community partners demonstrates a shared dedication to creating lasting solutions that serve the unique needs of eastern North Carolina.
By addressing the root causes that lead to emergency department overutilization, we’re working to not only improve the experience for our patients but also strengthening health care in our region.”
ECU Health and Pitt County DSS will host a third session of the conference to further discuss action items and strategies to support more collaboration in the community.
Greenville, N.C. – ECU Health has earned 2024 College of Healthcare Information Management Executives (CHIME) Digital Health Most Wired recognition as a certified acute and ambulatory Level 8. The Digital Health Most Wired program conducts an annual survey designed to identify and recognize health care organizations that exemplify best practices through their adoption, implementation and use of information technology and included more than 48,000 represented facilities in 2024.
“I am incredibly proud of our team’s dedication and innovation, which have been instrumental in achieving the 2024 Most Wired Award,” said Donette Herring, chief information officer, ECU Health. “Our efforts to improve the well-being and efficiency of our clinical team members and adoption of artificial intelligence were top priorities this past year. These achievements underscore the team’s commitment to innovation, education and the seamless integration of technologies across the organization. We look forward to building on these successes and exploring new opportunities to advance ECU Health’s strategies and improve operational performance.”

ECU Health ranked above peers in categories across eight key areas including: infrastructure, security, administrative/supply chain, analytics/data management, interoperability/population health, patient engagement, innovation and clinical quality/safety. Participants receive a comprehensive benchmarking report enabling them to evaluate their current information systems’ health. This report assists in devising strategies to elevate the quality of health care organizations to enhance industry-wide care standards. The assessment covers digital health performance. The survey assesses the adoption, integration and impact of technologies at all stages of development, from early development to industry leading.
ECU Health has piloted several initiatives to enhance patient care and streamline operations. The clinical communication program has enhanced the timeliness of communication and care coordination among team members, as well as increased workforce mobility, evidenced by high utilization in medication administration, documentation, and secure messaging. The MyChart Bedside program allows patients to access real-time education, lab results and pertinent care information directly from iPads, enhancing patient understanding and engagement. In the Emergency Department, the ‘Hello World’ initiative improves patient engagement through enhanced texting capabilities, keeping patients informed on next steps.
Additionally, regional facilities have expanded the tele-sitter program, optimizing resource allocation for patients who need monitoring but not constant one-on-one attention. The implementation of flowsheet macros has been a major efficiency booster, saving nurses millions of clicks and positioning ECU Health as a leader in this innovative adoption. ECU Health is also advancing artificial intelligence (AI) integration across its operations. The launch of the AI Center of Practice (AICoP) has gathered over 200 members across departments to foster collaboration and AI best practices.
“We are proud to recognize your ECU Health’s exceptional dedication to digital health excellence,” said CHIME President and CEO, Russ Branzell. “ECU Health’s pioneering performance in the industry not only inspires other organizations by example, but also provides patients around the world with better care.”
For patients in eastern North Carolina facing spine-related issues, ECU Health’s new minimally invasive spine surgery program at the ECU Health Neurosurgery & Spine Center in Greenville is designed to provide faster recovery times, fewer complications and improved outcomes. By focusing on complex spine procedures with less invasive techniques, ECU Health is enhancing access to high-quality care that allows patients to return to their lives quicker and with greater confidence.
“We are excited to offer minimally invasive spine surgery, which allows patients to experience a quicker recovery, less blood loss and reduced risk of complications, ultimately lowering the likelihood of needing additional surgery,” said Dr. Aaron Bond, neurosurgeon at ECU Health. “We’re committed to making these advanced procedures more accessible for our patients and to expanding this service in eastern North Carolina.”

The ECU Health Neurosurgery & Spine Center’s multidisciplinary team includes physician assistants and nurse practitioners, who support patients at every stage of care. In-house physical therapy services and a close partnership with ECU Health Neurology provide comprehensive support under one roof, improving the continuity and quality of care for patients with complex spine conditions.
“While not every patient is a candidate for minimally invasive surgery, those who are find it helps them avoid hospital stays and return to their daily lives more quickly,” said Dr. Bond.
These procedures are performed at ECU Health SurgiCenter, where many patients can undergo outpatient spine surgeries without the need for hospitalization. This approach is particularly effective for individuals suffering from acute herniated discs – often leading to sciatica, spinal stenosis – which frequently affects older patients, and traumatic burst fractures. Due to limited access to minimally invasive options in some areas, the center has seen a significant number of patients traveling long distances for treatment.
Patients who have undergone these minimally invasive procedures report notable success in reducing or eliminating back and leg pain, with recovery times significantly shorter than those associated with traditional open surgeries.
“Having these services available locally is crucial for improving patient outcomes,” said Dr. Bond. “It reduces the need for follow-up visits, cuts down on travel time and costs and ensures patients have consistent, accessible support right in their community.”
With growing demand for minimally invasive spine care, ECU Health’s Neurosurgery & Spine Center is combining state-of-the-art technology with a highly skilled support team. As demand continues to rise, ECU Health is committed to expanding its capacity and providing high-quality, accessible spine care to make a lasting difference for patients throughout the region.
D’Nise Williams is the program coordinator for the Eastern Carolina Injury Prevention Program’s (ECIPP) Teen Safe Driving Program. This year marks the 12th year in a row her team has received grant funding from the Governor’s Highway Safety Program (GHSP). The ECIPP is a community collaboration between ECU Health, Maynard Children’s Hospital, the ECU Health Trauma Center and the Brody School of Medicine at East Carolina University. Its goal is to improve the health of eastern North Carolina residents by reducing the incidence and impact of injuries, and it accomplishes this goal through programs like the Teen Safe Driving Program.
The Governor’s Highway Safety Program is the State Highway Safety Office for North Carolina, and it is dedicated to reducing the number of traffic injuries and fatalities in the state. It promotes highway safety through a number of grants and safe driving initiatives like Click It or Ticket and Speed a Little, Lose a Lot. Many of the grants address behavioral approaches to traffic safety, and the grant the ECIPP received focuses on vulnerable road users—in this case, teenage drivers.

The program’s grant runs for a one-year cycle, and each year, educational efforts focus on two counties, which are selected through examination of county crash rate data. “We look at which counties would benefit from interventions to reduce crash rates, even by a small percentage,” Williams said. With the help of the GHSP grant funding, the Teen Safe Driving Program has been able to expand its services from Pitt County to Beaufort, Lenoir, Martin, Craven, Wayne, Nash, Greene, Duplin and Halifax counties, with hopes to further expand into Onslow County this year. “GHSP has been funding this project for more than a decade,” said Jennifer Delcourt, the vulnerable road users coordinator with the Governor’s Highway Safety Program. “This speaks to the impact of the project and the success of staff in reaching teens and parents with important traffic safety information in eastern North Carolina.”
According to data collected between 2016 and 2021, speeding, lane departure and distracted driving were the top factors in car crashes. To combat this, the program focuses on “5 to Drive rules for new drivers,” as developed by the National Highway Traffic Safety Administration (NHTSA), which include no drinking and driving, buckling up, no use of phones while driving, no speeding and no more than one passenger at a time.
The Teen Safe Driving Program partners with high schools, as well as driver’s education programs, within the identified counties, to promote these safe driving practices for teenagers. “We do lunchtime education tables, partner with health science or P.E. classes, provide parent education curriculum and partner to bring the Cinema Drive interactive 3D movie experience to schools, which is an interactive driving experience that follows someone who has been drinking and driving. We have goggles and an interactive steering wheel, and you can pick out distractions as you drive with and without the goggles,” Williams explained. “The goal is to raise awareness that as a driver, you’re wielding tons of metal on the road, and you need to be your best self mentally.”
The program also provides targeted campaigns for teen drivers, including social media ads, billboards movie theater ads, mall campaigns and gas station TV ads. None of this would be possible without the funding from GHSP.
In 2023, the program achieved just over two million views in their mall campaign, 617 students in driver’s education classes, 7,168 students in lunchtime table education and 6,822 impressions via social media messages. These efforts have yielded positive results for the program. Teens are given pre- and post-intervention surveys to gauge their responses to the education, and there are also pre- and post-driver observations at the conclusion of driver’s education classes. “We usually see a change in behaviors, although it varies by county,” Williams said. “Last year we marked a 6% decrease in distracted driving in Pitt and Duplin counties, but the year before we recorded a 15-20% decrease in our counties of focus.”
Williams said that while it can be challenging to initially establish relationships with schools, once the partnership is established, the Teen Safe Driving Program is invited back year after year. Her goal is to continue to offer school interventions that result in safer driving behaviors, but she also has new ideas. “I want to work on targeted interventions for neurodivergent teens, like teenagers with ADHD or autism. We have so many teens who have trouble focusing already, and a teenager’s frontal lobe, which is responsible for making good decisions, isn’t fully developed,” Williams said. She also wants to establish a partnership with teenagers to create an advisory board for the program. “I’d like to think I’m ‘hip,’” Williams laughed. “But I would love to consult with other teenagers to get their input on what messaging reaches their age group.” Sue Anne Pilgreen, the executive director for the Safe Communities Coalition, the manager of the Pediatric Asthma Program and the manager of the ECIPP, echoed this sentiment. “Teens today aren’t the same as they were 12 years ago, and as they have changed, so has our program. We continue to focus on the historical distractions such as underage drinking and texting while driving, but we now know that mental well-being and substances such as marijuana can also impact teen driving.” Williams said consulting teens about what resonates most with them will help her find innovative and creative ways to reach and engage a teen audience.
Pilgreen championed Williams’s efforts to reach teen audiences across eastern North Carolina. “We are so fortunate to have D’Nise’s mental health background and expertise to better inform the education that we are offering, and to ensure that we are connecting with teens on a ‘real life’ level. My perception of a teens experience isn’t necessarily reality, and D’Nise knows that hers isn’t either. D’Nise is very intentional in bringing youth voices to her work, and structuring her programming and activities in a way that best impacts them.”
Williams emphasized that while the program’s focus on safe teen driving centers on a few counties each year, she is always available to speak to groups and do targeted programming and interventions. “I never turn down the opportunity to encourage kids to be safer,” she said.



