Work culture makes a difference in recruitment, retention and team well-being, and all health care organizations strive to offer a more loving work environment where team members can thrive.
Vidant Health Chief Experience Officer Dr. Julie Oehlert joined the SEE YOU NOW podcast, from Johnson & Johnson and American Nurses Association, and discussed leading organizational change on Episode 64: Reporting Powers: Leading With Love.
A new, loving culture
Dr. Oehlert said “power-over” or hierarchical relationships are at the core of many relational issues, and missed opportunities in health care. She encourages all of health care to work together with team members on culture innovations.
“I think most organizations use the definition of culture of ‘How we do things around here,’” Dr. Oehlert said. “That cultural definition is like you’re a fish swimming in a bowl. It is not actionable. We believe that culture is defined by how our relationships are structured with each other – how we treat each other, how we treat patients, how we treat our community, and that definition is very actionable and everyone can impact the culture.”
As team members partner to create a new, loving environment, team and organizational goals become much more achievable. Dr. Oehlert said measures such as whether team members are afraid of reporting safety events, if they feel heard by their manager, and if the community believes the health system is their partner, are key indicators of a positive, changing culture.
Dr. Oehlert noted the importance of looking to an organization’s own team members to change cultures and innovate in their own space. She believes that health care can improve if they listen to their team members who want to have a voice in their own work environment.
“You don’t need other people to help you with your culture. Do you know you have innovators sitting around in your hospital? They’re everywhere,” Dr. Oehlert said. “Your EVS and food services workers will redesign your food delivery in a hot minute. Don’t bother to pay a consultant. Your innovation awaits you if you walk into your departments. Give them an environment and ask them, listen to them and they will design beautiful things.”
It starts at the top
A culture shift in health care must include changes to leadership development. Transformational leadership is full of love, kindness and mentorship.
So, she and the Organizational Development department felt they needed to carve its own path.
“I called our chief operating officer and I had all of these books sitting around me, you know your scholarly books on leadership development,” Dr. Oehlert said. “So I’m looking at all these different models and I’m putting my head in my hands and I’m like, ‘None of these are going to take us where we want to go. We’re going to have to develop our own leadership curriculum and our own leadership framework.’”
A team came together and different and new frameworks were pulled together to create a unique system for Vidant to develop talented team members and grow leaders.
This new system was necessary to transform and later maintain a culture of love, empathy and power-with attitudes from organizational leaders.
“Leadership development is so important because the leaders are at the top of the hierarchy; if they are perpetuating fear or dominance, whether intentional or not, because some leaders were just taught to lead that way, that has to shift,” Dr. Oehlert said. “A new leadership way of being has to emerge.”
Policies reflect culture
Policies are a reflection of the workplace culture and policies can frequently be outdated and not in line with the culture of the organization.
Dr. Oehlert said as the culture shifted, the organization needed to review policies and procedures.
“It’s amazing how many policies, once you read them with a lens of caring and love that you realize – ‘This is terrible. Why would we have this policy?’” Dr. Oehlert said. “Are your policies by their nature punitive? How do you handle mistakes and coaching and errors with your team members? Do you have grace when they are humanly failing? Do you have grace for their mental health issues? You really have to dismantle that.”
Looking for more?
Find and listen to the SEE YOU NOW podcast, Episode 64. Reporting Powers: Leading with Love, wherever you get your podcasts.
Read more on Dr. Oehlert’s previous appearance on the SEE YOU NOW podcast.
Vidant Chief Experience Officer Julie Oehlert talks about nursing innovations on SEE YOU NOW podcast
Vidant Health Chief Experience Officer Dr. Julie Oehlert took time recently to discuss the Vidant system, nursing and innovation on the podcast series SEE YOU NOW.
Johnson & Johnson and the American Nurses Association launched SEE YOU NOW, a storytelling podcast that highlights innovative and human-centered solutions driven by nurses. The podcast addresses today’s most challenging health care problems.
Changing a culture
During her time on the podcast, Dr. Oehlert reflected on the importance of a positive culture in health care and how a strong culture can lead to improved patient and team member experience. When she first arrived at Vidant, she noticed the organization’s culture had room for improvement—including a shift from a “power-over” to a “power-with.” Dr. Oehlert said she focused most of the work in her first two or three years in the system on team members, love, empathy and bringing those elements into relationships so that a new, loving culture could emerge.

“It’s very clear in the science that one type of culture begets certain things and another type of culture doesn’t,” Dr. Oehlert said. “So in a power-with culture, you get a lot of innovation, empathy and compassion. You usually have good mentorship, good talent management, you have shared decision making, great patient experiences, good quality outcomes and people aren’t afraid to report near misses. That culture will deliver results that everyone in health care wants.”
As this desired culture became a reality at Vidant, it built a foundation for resilience in the eight-hospital health system and the more than 13,000 team members. Resilience is necessary at all times in health care to face the various daily challenges, especially in rural health care. But as a pandemic closed in, its importance was magnified.
Delivering health care in rural areas
Dr. Oehlert said delivering health care in rural areas is a challenge Vidant faces every day. The communities Vidant serves face many of the same problems other rural health systems see, along with its own unique challenges.
“People can’t get places, people don’t have access to things that they need or want. Anywhere where there are rural environments, in those kind of forgotten places anywhere in the world, these challenges would be the same,” Dr. Oehlert said. “When you’re in an urban environment, you’re 10 minutes from a resource. Here, you could be an hour and a half from a resource. That brings with it a lot of really interesting possible solutions.”
One of those solutions for Vidant is keeping resources out in the communities that need them. With regional hospital and clinic locations, she said Vidant can keep care and resources as close to home as possible for patients and families throughout a 29-county service area.
Adapting in a crisis
 The COVID-19 pandemic has made the need for care and resources close to home much more important. Dr. Oehlert said a key innovation since the onset of the pandemic has been clinic pop-ups throughout eastern North Carolina.
The COVID-19 pandemic has made the need for care and resources close to home much more important. Dr. Oehlert said a key innovation since the onset of the pandemic has been clinic pop-ups throughout eastern North Carolina.
These community health events bring crucial services, screenings and resources to areas that need them. Talent recruitment is another important service provided during these community events.
“We always bring a recruitment person. So we actually give people jobs, which is what our communities’ want, so we hire right out of these community events,” Dr. Oehlert said. “Then as soon as our entry-level workers get here, we say, ‘What else would you like to be? What else would you dream of doing?’ We do a lot of really relational recruitment right from our low-trust communities.”
Giving team members the room and resources to grow through various programs, like the HomeGrown program, is one way Vidant makes an effort to invest in its team members.
Innovating together
COVID-19 has changed the typical way of doing business across all industries, and health care is no different. Innovation often is born during crisis and desperation and Dr. Oehlert said that while health care is changing and innovating rapidly, advice from a mentor gives her comfort.
“Teddie Potter used to say very kindly to me when things were very chaotic, ‘Julie, sometimes things have to disassemble before they reassemble.’ That gives me some peace because health care is disassembling, but it’s only disassembling so we can reassemble it in a much better, more loving, more caring way that is exactly where we need to head for health care to be what we need it to be for our future,” Dr. Oehlert said.
Dr. Oehlert said while health care moves forward, it will be crucial to keep nurses involved in discussions around innovation because of their unique perspective and connection to the patients they serve.
“They can do it with love and empathy and joy and hope as well as having the technical and scientific expertise,” Dr. Oehlert said. “That’s the beauty of nursing, it’s a heart job but it’s a science job.”
Looking for more?
Find and listen to the SEE YOU NOW podcast, Episode 61. Reporting Powers: Insights in Action wherever you get your podcasts.
Greenville, N.C. – Sept. 28, 2021 – Since 1989, The North Carolina Great 100, Inc. has recognized and honored nurses around the state for their commitment to excellence and to promote a positive image of the nursing profession. Out of thousands of nominations that are submitted annually, 100 recipients are selected based on their outstanding professional abilities and contributions made to improving health care services to their communities.
This year, 14 ECU Health Medical Center (VMC) nurses have been selected to the 2021 NC Great 100.
Vidant Health extends heartfelt gratitude to these nurses for their contributions to patient care and living the Vidant mission of improving the health and well-being of eastern North Carolina.
The Vidant nurses chosen this year are:
Anthony Ayscue, BSN, RN, CRN, is the assistant nurse manager for ARU, VAT and Radiology Nursing at VMC. Anthony has been with Vidant for more than 18 years and has been in his current role for more than five years. Anthony is a certified radiology nurse, and earned an associate’s degree from Edgecombe Community College and a bachelor’s degree from Barton College. He is a member of the Association for Radiologic & Imaging Nursing.

Youssef Belahchich, RN, is a staff nurse III working in the Neurosciences Unit at VMC. Youssef has worked at Vidant for seven years and previously served as an orthopedic RN. He graduated from Pitt Community College with an associate degree in nursing and worked in a skilled nursing facility before joining VMC.

Amy Campbell, PhD, RN, CPHQ, LSBB, is a quality nurse specialist III on the Performance Improvement Quality Analytics team at VMC. Amy started her career as a staff nurse on the pediatric floor at the former Pitt Memorial Hospital in 2000. Amy has been in her current role for 12 years. Amy earned an associate degree in nursing from Pitt Community College, bachelor’s degree in science nursing from East Carolina University (ECU), as well as a master’s degree and PhD in nursing from ECU. She is certified in Lean Six Sigma Black Belt from North Carolina State University and is a certified professional in Health Care Quality. Amy was an East Carolina Hall of Fame doctoral scholar and the 2018 Association for Leadership Science in Nursing Doctoral Grant recipient. Amy is a member of National Association of Healthcare Quality, Association of Leadership Science and Sigma Theta Thau.
Michelle Carawon, MSN, RN, CCRN-K, is an infection control preventionist III at VMC. Michelle has been with Vidant for 16 years and has been in her current role for the past year. Michelle is certified in critical care nursing and earned a bachelor’s degree in nursing from East Carolina University and a master’s degree in nursing from Walden University. Michelle is a member of the American Association of Critical Care Nurses, Sigma Theta Tau-International Honor Society of Nursing, the Association for Professionals in Infection Control and the East Carolina University Alumni Association.

Miriam Coggins, BSN, RNC, is a staff nurse at VMC’s Neonatal Intensive Care Unit (NICU). Miriam has worked in the NICU at VMC for 36 years. She earned a bachelor’s degree in science nursing from East Carolina University. Miriam has held multiple roles at VMC including permanent charge nurse, assistant nurse manager and interim manager. As interim manager she assisted with the opening of VMC’s current 50 bed NICU. Miriam has a certification in neonatal intensive care and serves as co-chair of the Central Line Team.

Roland Ennis, RN, is an assistant nurse manager of the Orthopedic Unit at VMC. Roland has been with Vidant for 21 years and has served in his current role as assistant nurse manger for 10 years. He earned an associate’s degree in nursing from Edgecombe Community College.

Amanda Helms, BSN, RN, is a staff nurse III in the Trauma Surgery Intermediate Unit at VMC. She has been at Vidant for 15 years and has served in her current role for nine years. Amanda earned an associate’s degree in nursing at Beaufort County Community College and received a bachelor’s degree in nursing from University of North Carolina at Wilmington. Amanda obtained trauma nursing core course certification and is a member of the American Nurses Association, North Carolina Nurses Association, Society of Trauma Nurses and Sigma Theta Tau International Honor Society of Nursing.

Kristie Hertel, MSN, RN, CCRN, ACNP-BC, FCCM, is an advance practice provider with the Trauma and Surgical Critical Care Department at VMC. Kristie started at VMC in 2006. Kristie earned a bachelor’s degree from Nazareth College, a master’s degree from Rush University and is currently enrolled at UNC Wilmington working toward a doctorate in nursing practice. She has received specialty certification as a certified critical care nurse and acute care nurse practitioner along with induction as a fellow in the Academy of Critical Care Medicine. Kristie is a member a member of the American Association of Critical Care Nurses, Society of Critical Care Medicine and Sigma Theta Tau International.

Stephanie Head, MSN, RN, PMGT-BC, NE-BC, is the nurse manager of the Vidant Pain Management Center, a hospital outpatient department of VMC. A Vidant nurse for 30 years, Stephanie has been the manager at the Vidant Pain Center for the past nine years. Prior to her current role, Stephanie served as a nursing assistant for two years. Stephanie earned a bachelor’s degree and master’s degree in nursing leadership from East Carolina University. She holds a specialty certification in pain management nursing and is a nurse executive-BC. Stephanie is an active member with American Society of Pain Management Nurses and North Carolina Organization of Nurse Leaders.
Patty Jordan, MSN, RN, NE-BC, CCCC, is a senior nurse administrator in Patient Care Services at VMC. Patty has been with Vidant for five years. She earned a bachelor’s of science degree in nursing and a master’s of science degree in nursing and health care administration from Southern Illinois University – Edwardsville. Patty has obtained specialty certifications as a nurse executive, and as a cardiovascular care coordinator. Patty is a member of American Association of Critical Care Nurses, East Carolina Chapter of American Association of Critical Care Nurses, American Organization of Nurse Leaders, Sigma Theta Tau, and the North Carolina Nurses Association.

April Meeks, BSN, RN, PCCN, is the assistant nurse manager on the Palliative Care Unit at VMC. April has been with Vidant for 15 years and in her current role for more than a year. She earned an associate degree in nursing from Edgecombe Community College and a bachelor’s degree in nursing from the University of North Carolina at Wilmington. April is specialty certified as a progressive care certified nurse. April is a Daisy Award Honoree and a Vidant Brody Award Finalist. April is a member of the American Association of Critical Care Nurses, North Carolina Organization of Nurse Leaders, North Carolina Association of Healthcare Quality and Sigma Theta Tau.

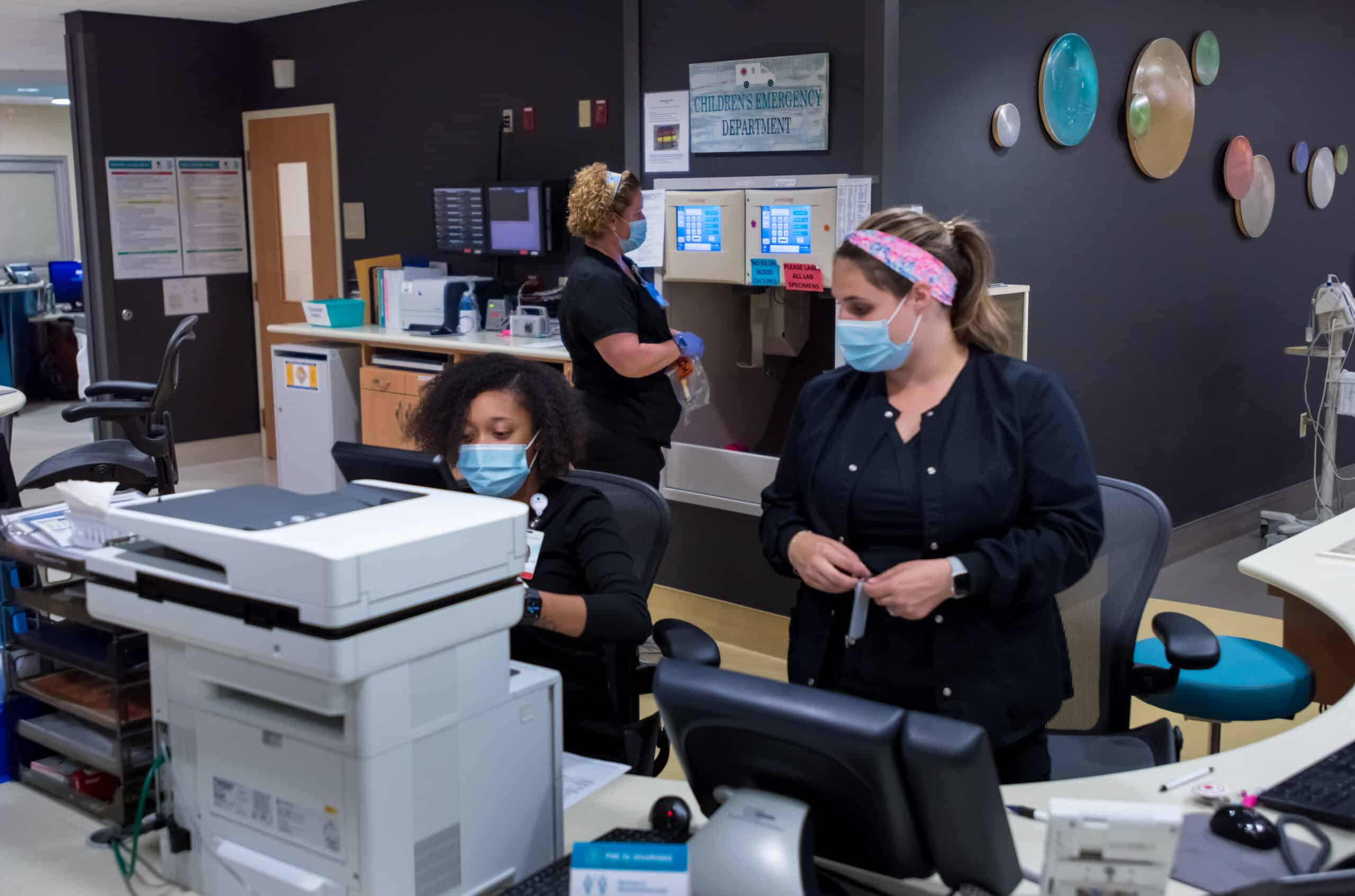
Shannon Mazza Roberson, BSN, RN, CPEN, SANE-P, is a staff nurse IV in the Special Care Nursery at Maynard Children’s Hospital. Shannon has been with VMC for the past eight years and she earned a bachelor’s degree from Barton College. She began her career with Vidant in the Children’s Emergency Department as a staff nurse. Shannon has been a part of the leadership team within Emergency Services as both assistant nurse manager of the Children’s ED and nurse manager of the Adult ED. Shannon has more than 23 years of nursing experience and has cared for pediatric patients throughout her career. She is a certified pediatric emergency nurse as well a sexual assault nurse examiner for pediatrics. She is a 2020 finalist for the Vidant Brody Award as well as a Daisy and Team Daisy Award recipient. Shannon holds multiple certifications in the field of Emergency Services. Shannon is a member of the International Association of Forensic Nurses, the Emergency Nurses Association and a member of Sigma Theta Tau.

Sherry Stone, DNP, RN, NPD-BC, is an education specialist in nursing at VMC. Sherry has been at Vidant for six years. She earned an associate degree from Patrick Henry Community College, a bachelor’s degree from Old Dominion University, a master’s degree from Western Governor’s University and a doctorate in educational leadership from American Sentinel University. Sherry has obtained certification in nursing professional development. She is a member of the American Nurses Association, the North Carolina Nurses Association, the National League for Nursing and The Association for Nursing Professional Development for which she serves as the chair for the Recognition Committee.

Ashley Venters, MSN, RNC-LRN, is a staff nurse III in Special Care Nursery at VMC. Ashley has been in her role for more than 14 years and earned a bachelor’s degree and master’s degree in nursing education at East Carolina University. Ashley is currently working towards post-master’s work in the field of family nurse practitioner. Ashley obtained her specialty certification in low-risk neonatal nursing and is a member of Beta Nu and Sigma Theta Tau.
Since 1989, The Great 100 Gala has recognized and honored nurses in North Carolina for their commitment to excellence and to promote a positive image of the nursing profession. Out of the thousands of nominations, the selection committee chooses 100 nurses to honor as the best of the best in the state. Read more »

