In recognition of the one-year anniversary of Medicaid expansion in North Carolina, Gov. Roy Cooper visited ECU Health Medical Center in Greenville to reflect on the impact of expansion and celebrate a year of reaching North Carolinians in need.
Since Medicaid expansion officially launched in North Carolina on Dec. 1, 2023, more than 80,000 eastern North Carolinians and nearly 600,000 people statewide have benefited from access to vital health insurance. Along with Medicaid expansion, the state also passed the Healthcare Access and Stabilization Program (HASP), which provides critical relief to rural hospitals.
Gov. Cooper said Medicaid expansion’s reach in rural communities, like ECU Health’s 29-county service area, has been especially impactful in the last year.
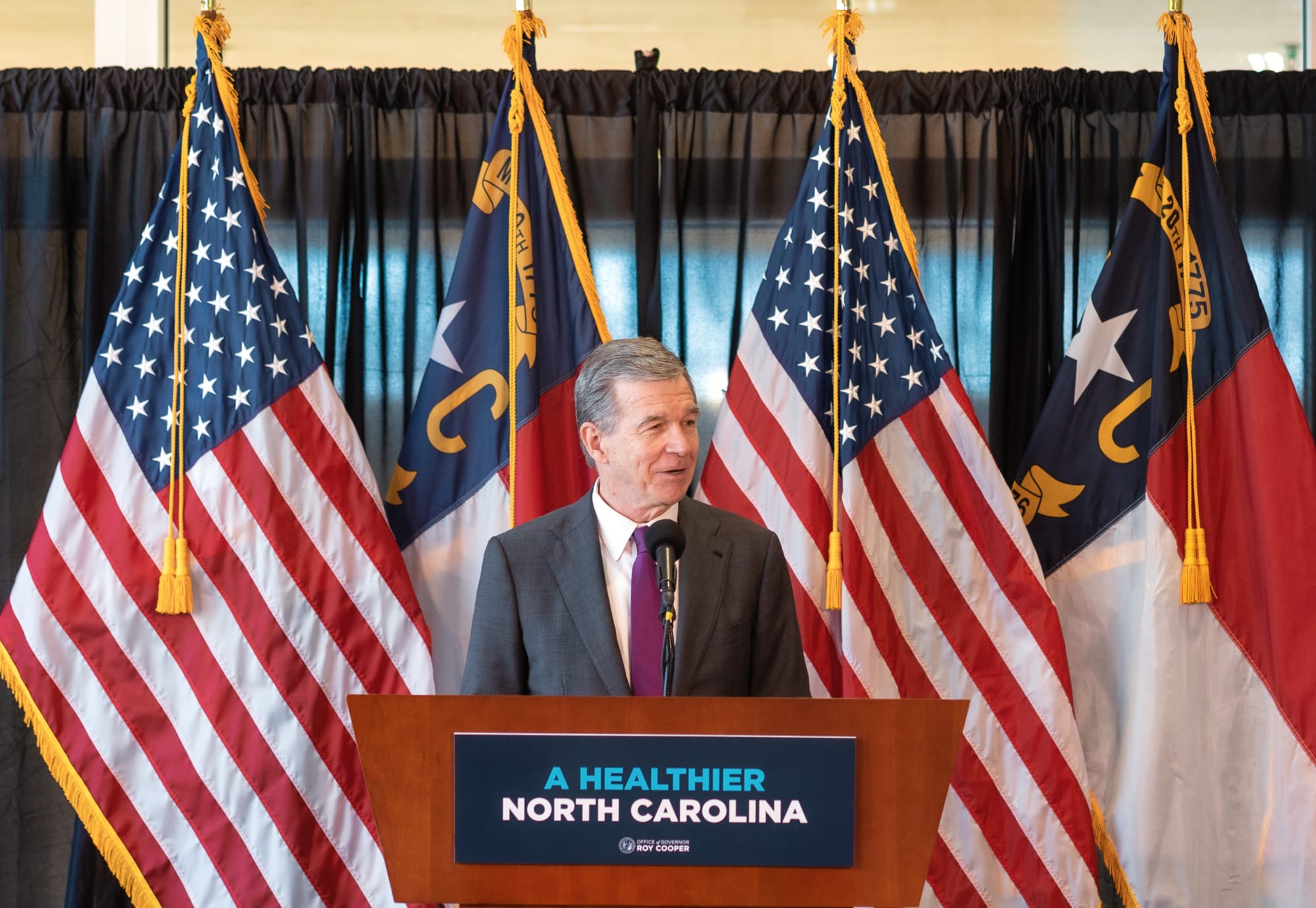
“The last year showed us that this is something that people desperately needed, particularly here in rural North Carolina,” Gov. Cooper said. “I grew up in Nashville and we know that rural North Carolinians have been helped more by Medicaid expansion than anyone else. I hold close to my heart the mission of getting people healthier. I knew getting Medicaid expansion passed and signed into law was the most important thing we could do to accomplish that.”

This milestone reflects the culmination of more than six years of advocacy by ECU Health, driven by the challenges faced by uninsured and underinsured patients.
Dr. Michael Waldrum, ECU Health chief executive officer and dean of the Brody School of Medicine at East Carolina University, said Medicaid expansion and HASP funding is creating real differences for patients, health care workers and the future of health care in places like eastern North Carolina.
“Medicaid expansion has helped improve access to primary care, empowering people to take control of their health and their lives,” Dr. Waldrum said. “It is also an investment in rural health organizations like ours. At the same time and in partnership with the state, ECU Health and the Brody School of Medicine are also committed to doing their part to support primary care expansion efforts in rural health care.”
He highlighted the expansion of the Rural Family Medicine Residency program, which will train nine rural residents per class across three training sites in the East and the upcoming Center for Medical Education Building on Brody’s campus. This investment has helped and will continue to help ECU Health and Brody serve the combined mission of improving the health and well-being of eastern North Carolina.
Dr. Karen Coward, a family medicine physician with ECU Health, is a Kinston native and practices in Tarboro. She said she knew by age 10 she wanted to be a family physician in her home community. She attended Brody and stayed true to her dream of serving eastern North Carolina.
She said before Medicaid expansion, many of her patients would rely on the emergency department for care. Even if a patient was connected with primary care, it was difficult for them to follow through with appointments or afford medications. Chronic conditions like diabetes, hypertension or even cancer would go unchecked. Now, she said, she’s seen a life-changing shift.
“Patients who once cycled through the emergency department are now establishing relationships with primary care providers like me,” Dr. Coward said. “They are keeping their appointments, following through on recommendations, treatments, and gaining access to medications and specialist referrals that were previously out of reach. For many, this will mean earlier diagnoses and interventions, reducing the burden of advanced diseases.”
Kody Kinsley, secretary of the North Carolina Department of Health and Human Services, joined the event and said that in the past year over $58 million in dental claims alone were filed, millions of prescriptions were filled and hundreds of millions of dollars in claims supporting hospital care were taken care of through Medicaid expansion.
He said this comprehensive health insurance is already making a real difference for individuals and families.
“Medicaid expansion is life changing for families,” Sec. Kinsley said. “It is peace of mind for people as they sit up late at night thinking about how the next day will impact them. Will a sickness impact their family? Will they end up in debt? They don’t have to worry about that anymore.”

The event also included remarks from a Medicaid expansion beneficiary, Darcy Guill from Ayden, who shared her gratefulness for regular care she’s receiving, specialists she’s able to visit and prescriptions she can fill, thanks to Medicaid expansion.
As we look back over the previous year, we’re proud to build the national model for rural health care here in eastern North Carolina at ECU Health and we’re grateful for the support the region and health system through Medicaid expansion and HASP.
Greenville, N.C. – Trish Baise, ECU Health chief nursing executive, was recently honored as one of Becker’s Hospital Review’s 2024 Chief Nursing Officers (CNOs) to know. Since stepping into the role in 2022, Baise has cultivated a dynamic nursing environment that drives innovations to enhance patient care quality and elevate patient experiences across eastern North Carolina.
“This recognition by Becker’s reflects the collective efforts of the incredible nurses across ECU Health, all of whom are dedicated to creating an environment where nurses and patients alike can thrive,” said Baise. “Together, we are driving innovative approaches in rural health care, committed to excellence in all we do and enhancing patient care across eastern North Carolina. I am honored that ECU Health has been recognized for this commitment.”
Tasked with addressing nurse staffing shortages, managing budgets and fostering growth opportunities for emerging nurses, the nursing leaders recognized by Becker’s play a crucial role in shaping the future of nursing.

Beyond leading nursing departments, CNOs drive innovative initiatives that uphold high patient care standards. Their roles demand a unique blend of clinical expertise and executive leadership. This list honors CNOs for their commitment to optimizing health care.
Baise has led efforts to establish a supportive environment where both nurses and patients can thrive. Under her leadership, ECU Health has achieved its third Magnet recognition, underscoring a commitment to nursing excellence. The Advancing Nursing Practice and Excellence (APEX) initiative has been foundational to this strategy, focusing on innovation, research and collaborative efforts to advance nursing in rural health care. Through partnerships with East Carolina University and local colleges, ECU Health also invests in the future of nursing, offering residency programs to equip new nurses with essential skills. This vision represents ECU Health’s dedication to defining a new standard for patient care and nursing excellence in eastern North Carolina.
“As the region’s largest health care provider and educator, ECU Health has a unique role in shaping community health, and Trish understands that our mission’s success depends on attracting the best providers, nurses and care teams to our health system,” said Dr. Michael Waldrum, CEO of ECU Health and Dean of the Brody School of Medicine at East Carolina University. “Trish’s dedication to service and our mission aligns with ECU Health’s work to build the model for rural academic health care. ECU Health is proud to lead the way in defining the future of nursing in our region.”
Resources
Amy Campbell, PhD, RN, CPHQ, LSSBB, quality nurse specialist III, represented ECU Health on Sept. 25 at a side event held in parallel to the 79th session of the United Nations (UN) General Assembly in New York City. The meeting, titled “2030 Global Agenda for Sepsis for Attaining Sustainable Development Goals,” was convened as a collaborative effort of the Global Sepsis Alliance (GSA), Medical Women’s International Association, Sepsis Stiftung and UNITE Parliamentarians Network for Global Health.
The meeting was the first-ever global strategy spearheaded by the GSA, with collaboration from 70 partner and member organizations from Regional Sepsis Alliances across Africa, Asia-Pacific, the Caribbean, eastern Mediterranean, Europe, Latin America and North America. The meeting’s objectives were:
- To present the 2030 Global Agenda for Sepsis as the first multi-year global strategy to alleviate the significant human, societal, economic and health care burden of Sepsis.
- To reach consensus on the urgent need for reinvigorating the Sepsis responses at global, regional and national levels for the attainment of 2030 SDGs including the aspirations for Universal Health Care, Maternal, Neonatal and Child Health, AMR, Pandemic PPR, Gender Equality, Peace and Partnerships for Development.
- To discuss the critical role of health care workers, especially the medical women, representing over 70% of the health workforce globally, in the promotion and implementation of the 2030 Global Agenda for Sepsis.
- To call for establishment of a High-Level Political Platform for Sepsis to lead integration of this global health threat into the mainstream of health and development dialogue and architecture, including G7 and G20 Summits, World Health Assemblies, UN General Assemblies, and World Economic Forums.
Dr. Campbell was personally invited to attend and speak by Dr. Mariam Jashi, MD, MPH, MPA and the CEO of the Global Sepsis Alliance, and Michael Wong, founder and executive director of the physician-patient alliance for health and safety. This invitation came as a follow-up to the 2024 World Sepsis Congress held this past April, during which Campbell served on the Scientific Committee. “I saw the invite and initially blew it off,” Dr. Campbell laughed. “I wasn’t sure it was real.” But after reassurance the invitation was legitimate, and with the encouragement of her team and Michael Wong, Dr. Campbell decided to go to New York. “I had a training session scheduled at work, but my colleagues covered for me,” she said. “I’m so thankful to my team and leaders who made it so I could attend.”
Once she arrived at the New York University campus, where the parallel session was held, Dr. Campbell said she met many leaders from across the world. “I met Dr. Eleanor Nwadinobi, the president of the Medical Women’s International Association (MWIA), Thomas Heymann, the president and CEO of the Sepsis Alliance and the Honorable Dr. Ricardo Baptista Leite, a member of the Portugese Parliament. People were speaking all these different languages and here I was from eastern North Carolina.”
The meeting focused on early detection of sepsis and how to treat patients with sepsis, no matter where they live. “As one of the speakers, I had the opportunity to emphasize the urgency of early detection, the critical need for continued research and the importance of securing funding so that everyone, regardless of their geographic location, can receive the same standard of care and chance for survival,” Dr. Campbell said. The speakers also discussed what they anticipated to be the next big problem with sepsis: antibiotic resistance.
Dr. Campbell said it was a great opportunity to represent the work she and ECU Health are doing to address the global problem of sepsis. “The attendees were impressed with the work we’re doing. ECU Health is a big deal; we have incredible people and talent, and we deserve a seat at the table,” she said. And next year, she has a seat waiting for her. “I’ve been invited back to speak next year, and I’ll work more with the GSA,” she shared. “We all have a lot to learn and do. Sepsis transcends borders, affecting individuals of all ages, races and socioeconomic backgrounds. However, the most vulnerable populations – children, the elderly and those in low-resource settings – are disproportionately impacted. Sepsis doesn’t wait, and neither can we.”
Greenville, N.C. – ECU Health Medical Center has been nationally recognized as a national leader in patient experience for the second consecutive year, according PEP Health’s 2025 rankings. PEP Health evaluated more than 35 million online reviews from patients and their families in 2024, offering a real-time look at patient experiences across health care providers nationwide.
ECU Health Medical Center’s recognition was highlighted by top-5 national rankings in several categories including overall patient experience, communication & involvement and emotional support.
“At ECU Health, creating caring experiences for our patients and team members is at the core of our mission,” said Dr. Julie Kennedy Oehlert, chief experience officer at ECU Health. “Our definition of excellence is shaped by feedback from our patients and fostered by the compassion and dedication of our team. Being recognized nationally for our excellence in communication and emotional support is a rewarding acknowledgment of the safe, healing environments we strive to create. We are committed to continually listening and evolving to meet the needs of those we are honored to serve.”

PEP Health’s 2025 Rankings focus on hospitals with at least 750 staffed beds and at least 250 patient experience comments left online between Sept. 1, 2023, and Sept. 1, 2024. These comments, sourced from patients and their families on social media and review platforms, were analyzed against seven internationally recognized domains of patient-centered care: fast access, effective treatment, emotional support, communication & involvement, attention to physical and environmental needs, continuity of care, and billing and administration.
According to PEP Health, research has shown that enhancing patient experience is not only associated with improved care outcomes, but also strengthens financial performance, safety and health equity. Positive patient experiences directly impact CMS Star Ratings, which are closely tied to reimbursement rates and play a critical role in driving new patients and increasing patient retention. ECU Health’s commitment to delivering exceptional care in eastern North Carolina ensures that the most vulnerable populations in receive the support and attention they need.
“This recognition is a testament to the unwavering dedication of our team members who bring compassion and empathy to every patient interaction,” said Brian Floyd, chief operating officer, ECU Health. “Caring for patients during some of life’s most challenging moments is more than a job – it’s a calling. I am incredibly proud of the heart and commitment our team demonstrates every day. Earning this national recognition for patient experience reflects their hard work and the trust our patients place in us, and we will continue to prioritize compassionate, patient-centered care in all we do.”
ECU Health serves a vast rural region and understands the critical need for accessible health care in these communities. The demand for health services is exceptionally high, and many residents face significant barriers to receiving the care they need. ECU Health launched the Health Hub initiative in May 2023 as a strategic effort to bridge these gaps and help meet patients where they are. These Health Hubs are designed to improve access to vital health care and community resources, specifically targeting underserved areas.
“These hubs are strategically placed based on data indicating regions of high social vulnerability,” said Kasey Perkins, community health engagement coordinator, ECU Health. “Oftentimes, these areas have limited access to primary care services and individuals have difficulty seeing a doctor for those unexpected acute illnesses we all get.”
Health Hubs are currently located in four counties: Pitt, Martin, Edgecombe and Beaufort.
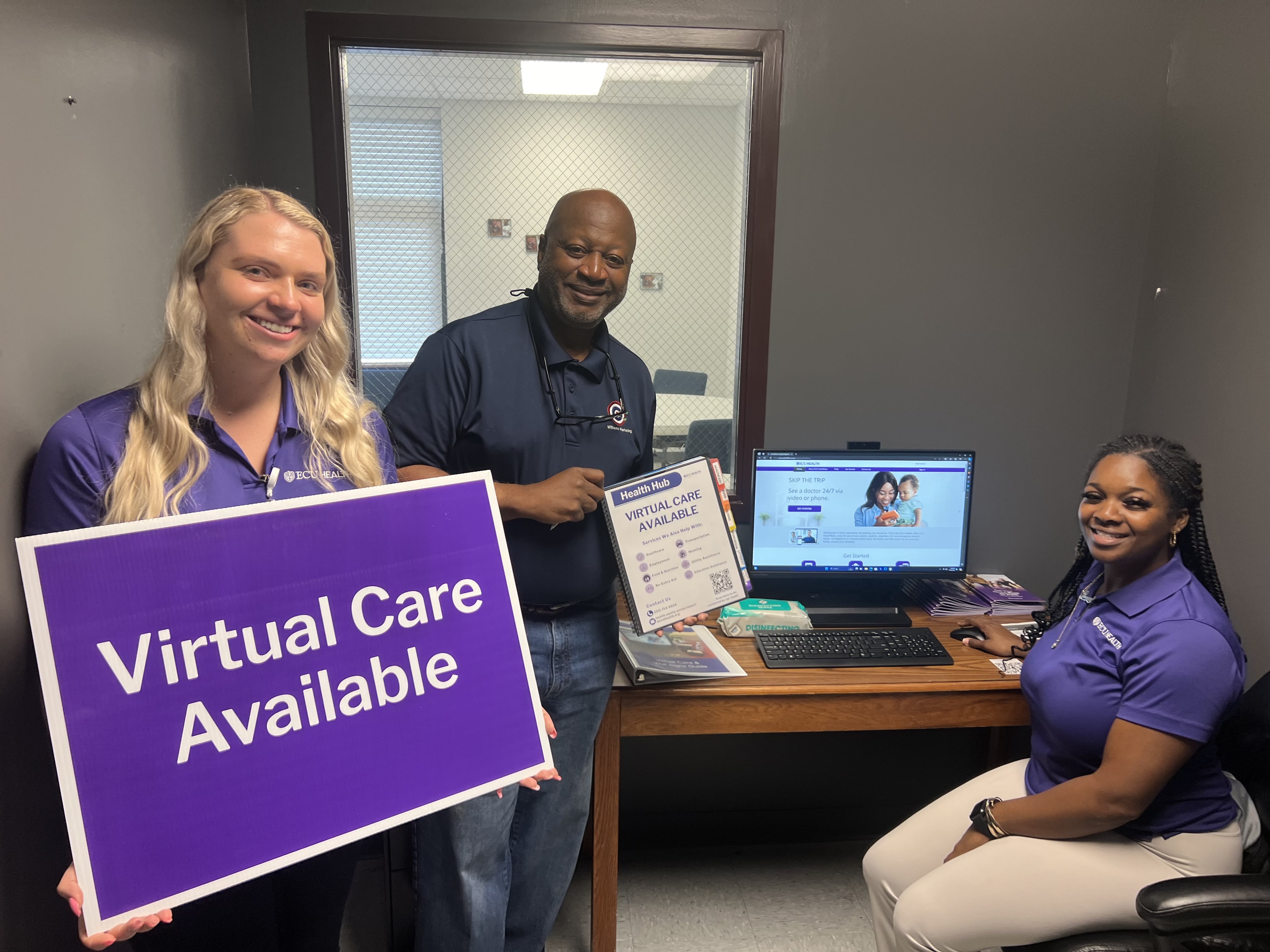
The hubs serve dual purposes. First, they provide access to virtual care, which is particularly vital in areas where individuals might otherwise visit emergency departments for non-urgent issues. By educating the community about virtual care options, Health Hubs help people get appropriate care quickly and more efficiently. Second, Health Hubs offer a gateway to community resources, addressing social determinants of health such as food insecurity, housing and employment.
“Each hub features a community resource guidebook, organized into tabs for different social needs, filled with contact information and details on various agencies and services available in the area,” said Perkins.
Health Hubs are located at local churches, businesses and organizations, and a designated Health Hub ambassador serves as the community’s point of contact. These ambassadors help residents connect with virtual care services and navigate the resources available to them. The hubs are equipped with necessary devices, including a computer with a webcam and microphone, and vital sign monitors like blood pressure cuffs, pulse oximeters and thermometers. This equipment allows individuals to have virtual visits on-site if they don’t have access to the technology at home.
Three new locations were added in July 2024, bringing the total amount of Health Hubs to 21. Health Hubs are open to everyone in the community. Residents can walk in during designated hours to learn more about virtual care or access community resources. The virtual care service, ECU Health Now, is available for anyone throughout eastern North Carolina and can be accessed on a computer or mobile phone. It is free to register and make an account, and it only costs $55 per visit when you speak with a provider, which is often less than a typical insurance co-pay or Emergency Department visit.
“The Health Hub initiative represents a significant step toward making health care more accessible and addressing broader social needs,” said Perkins. “By partnering with local organizations and connecting individuals with vital resources, Health Hubs are making a real difference in the communities they serve.”
As ECU Health continues in its journey toward leading positive changes in support of the health and well-being in the communities it proudly serves, its impact can be seen – and tasted – in the health system’s nine hospital cafeterias where Food and Nutrition team members create delicious and healthy food options for patients and visitors.
With a focus on plant-forward meals that support health, well-being and a healing experience, the Food and Nutrition team has been instrumental in ECU Health’s team member and community-focused Blue Zones initiatives, which recently won the North Carolina Hospital Association’s 2024 Highsmith Award for Innovation.
The four Blue Zones initiatives implemented by ECU Health include the Team Member Blue Zones Challenge, Plant-Forward Meals for patients and team members, Wellness Center Blue Zones, and targeted initiatives in Bertie, Chowan and Dare County. ECU Health is prioritizing the community and engaging in partnerships with local foodbanks and churches to spread the word of the initiative – and make sure the community knows that healthy, plant-forward food is not only nutrient-dense, but also delicious.

None of it would be possible without the expertise of the Food and Nutrition team. With nearly 300 Food and Nutrition team members helping prepare nearly three and a half million healthy and delicious meals at ECU Health locations across the region, this team is making healthy food accessible to patients, families and team members. On any given day, the ECU Health Food and Nutrition team prepares a menu inspired by international cuisines which heavily feature plant-based ingredients: Tandoori chicken, chipotle chicken tacos, sushi, to name just a few.
“It’s hard to describe how fortunate we are at ECU Health to have such an incredible Food and Nutrition team, which is truly at the heart of our work to encourage healthier lifestyles through the Blue Zones initiatives,” said ECU Health Chief Well-being Officer Dr. Christina Bowen. “Our team members and communities benefit from the amazing work they do. Their passion for creating meals that not only taste good, but are also good for you, is a critically important part of the positive change we are leading in eastern North Carolina.”
The summer break was no break for more than two dozen East Carolina University College of Nursing students who got to see what their post-graduation life could be like with a new student nurse extern program sponsored by ECU Health Medical Center in Greenville.
In the summer of 2023, shortly after an expansive academic-practice partnership agreement was signed between ECU Health and the College of Nursing, leaders from both organizations explored options to help expand the number of new graduates who could fill vacant nursing ranks across eastern North Carolina.
One of the initiatives the group quickly agreed on was an extern program: nursing students would be certified as nursing assistants and then work in a variety of care settings across the health system to gain practical experience before starting their final semesters of nursing school.

To be eligible for the extern program, student nurses would be required to complete Nurse Aide II certification, which all nursing students are eligible for, but not all take advantage of. Nurse Assistants are allowed to perform limited patient care activities as well as assist licensed health care workers with taking notes and uncomplicated wound care.
Dr. Jeanne Martin, chair of the baccalaureate nursing program, said the certification gave ECU Health leaders the confidence that the nursing students could “function within the scope of an NA II all the while learning the RN role with their preceptor.”
“During clinical experiences, students function under the licensure of their faculty and may administer meds or other skills not part of NA II certification,” Martin said.
While their practical role was limited, Martin stressed that the intangible skills the students learned – like how to comfort a patient and translate complex medical terminology and procedures to a patient’s families, was invaluable.
On July 9, the graduates of the first extern program gathered at the Monroe Center on the ECU Health campus to celebrate their accomplishments with their preceptors and the leaders who originated the program.
“I’m so grateful that you took this journey with us and congratulations. We appreciate the opportunity to partner with you on your professional journey,” Dr. Trish Baise, ECU Health’s chief nursing executive, said to the graduates during the ceremony. “Our goal is for you to be as prepared as you possibly can be as you transition into practice.”
Baise said she plans to expand and evolve the program so that more nursing students have an opportunity to gain valuable experience while still in school because nursing care is increasingly complicated and challenging.
Dr. Bim Akintade, dean of the College of Nursing, was an early proponent of the academic-practice partnership and said he is thrilled at the results the inaugural cohort of externs achieved during their eight-week experience.
“We are very thankful for ECU Health’s efforts to give our students a chance to learn some of the inner workings of their profession now, before they graduate. Once they are licensed and at the bedside, their nurse managers, and more importantly their patients, will rely on them to be ready on day one, and this experience puts them in an excellent position to be ready,” Akintade said.
Tracy Langston, ECU Health’s director of nursing professional development and innovation, was the medical center’s lead for the extern program and responsible for placing the students in their roles. She is most proud of the growth the student nurses achieved with developing their time management and communication skills.

“It’s been a phenomenal experience for our externs. They really increased their confidence as nurses, they are excited about the skills they were able to achieve and experience, and they’ll use that as they finish nursing school,” Langston said. “They spoke about how this program helped them work on their time management skills and prioritization as they prepare to hopefully join us as new graduate nurses after graduation.”
During the ceremony, students recounted their experiences during the extern program.
Blair Beaulieu, a nursing student from Greenville, said working alongside the family medicine team gave her insights into the working life of a nurse that she just couldn’t get from textbooks and classroom lectures.
“This program allowed me to explore the various opportunities and interdisciplinary communication, walking information down to the laboratory, transferring patients who needed higher acuity needs of various floors — just seeing those inner workings of a hospital,” Beaulieu said.
Kiley Fisher almost missed the graduation ceremony and was dressed in grey scrubs, rather than Pirate nurse purple, having raced over from the hospital after helping with a birth.
Fisher credits her experience with reinforcing foundational skills — like drawing blood and placing Foley catheters — which gave her space to work on critical thinking and communication with all members of the care team.
“I can now not freak out when a patient asks a question that I don’t know the answer to and how to continue to look professional while saying I don’t know, let me find out for you,” Fisher said. “It’s reaffirmed that nursing is where I’m meant to be.”
Emma Campbell, a nursing student who worked in the ambulatory clinics, found her footing, and her voice, while working directly with patients.
“I was challenged to develop my interprofessional communication, my confidence in my interactions with patients,” Campbell said. “Working with family medicine clinics, I was able to improve in these areas substantially.”

Kinsey Cook, one of the student nurses, said the extern program forced her to gain new levels of self-confidence, largely because she wasn’t given a choice.
“I was shy and nervous around other team members, but I gained confidence throughout this program by answering the phone and assessing the plan of care with doctors. I was able to talk to pathology, labs, pharmacy, nutrition services, and I got to see more than just the nursing aspect of patient care,” Cook said.
Cook spoke with pride at learning to believe in herself in the clinical role, as well as advocating for the patients she interacted with, a skill fostered by spending time with a charge nurse in the unit to which she was assigned.
Ankita Das said her experience working with palliative care teams helped her to develop a set of skills that can’t be learned in the classroom — one-on-one interactions with patients and the loved ones in the room with them.
“During this externship I realized I needed to further develop, and learn more about, comforting patients, family members and what to say when their loved ones passed,” Das said. “I observed the chaplains’ interactions with the families — they were empathetic and always offered to talk about memories with family. They lent a shoulder to cry on and a listening ear, this helped me learn what to do and what to say when a patient passes.”
The program’s success has given its leaders hope for future iterations, and opportunities to expand student participation in the future across the health system’s locations in eastern North Carolina.
“One of the reasons for implementing a student nurse extern program is that it’s an excellent recruitment and retention tool,” Langston said. “This is just the start. We are looking forward to continuing our student nurse extern program in 2025, so students — get ready to apply in December.”
As part of its commitment to providing high-quality care to the people of eastern North Carolina, ECU Health now offers innovative advanced 3-D shoulder replacement surgery, providing a new solution for patients with complex shoulder joint damage. This cutting-edge procedure is designed to relieve pain and restore mobility for individuals suffering from conditions such as osteoarthritis, rotator cuff injuries and fractures.
According to Dr. Shawn Yeazell, ECU Health orthopedic surgeon, patients can sometimes have one or more shoulder replacements that failed or wore out, which leaves only a little bit of bone to work with, so traditional implants don’t work.
“We have an aging population, which is increasing the demand for orthopedic procedures like joint replacements,” said Dr. Yeazell. “We want our patients to live comfortably and to be able to do the things they love, so having the ability to provide complex procedures to relieve pain and joint immobility is crucial.”
Traditional shoulder replacement surgeries involve removing damaged bone and replacing it with standard metal and plastic parts. According to Dr. Yeazell, standard shoulder replacement parts work for most people who need a procedure. However, in cases where bone is missing or existing bone is poor quality, standard parts may not be sufficient.
“There’s a certain amount of bone that’s required for a traditional replacement,” said Dr. Yeazell. “The 3-D printed shoulder replacement surgery is a solution for those patients who would have no other option.”
The 3-D shoulder replacement process begins with doctors performing CT scans of the patient’s shoulder. These scans are then sent to an outside vendor, which creates 3D-printed joint replacements custom-fitted to the patient’s anatomy. This personalized approach allows orthopedists to perform surgeries with greater precision and effectiveness.

“Being able to perform cutting-edge procedures like 3-D joint replacement surgeries close to home is critical in caring for our region,” said Dr. Yeazell.
By offering 3-D shoulder replacement surgery, ECU Health is enhancing the quality of life for patients with complex shoulder conditions, ensuring they can continue to enjoy their daily activities pain-free. Dr. Yeazell is the first surgeon to bring the Zimmer Biomet 3-D custom Vault Reconstruction System (VRS) implant and associated technology to the ECU Health System.
To learn more about ECU Health’s orthopedic services, visit www.ecuhealth.org/ortho.
Dr. John Catanzaro, professor and chief of the Division of Cardiology at the Brody School of Medicine at East Carolina University and director of the East Carolina Heart Institute at ECU Health Medical Center, was recently honored with the prestigious Dr. John “Jack” Rose Distinguished Professorship, recognizing his significant contributions to improving health care delivery, excellence in clinical medicine, administration and academic advancement, including formation of the first Clinical Cardiac Electrophysiology Fellowship at ECU Health.
The Rose Professorship, established by ECU Health and East Carolina University through the ECU Health Foundation and state funds, honors Dr. Rose, a renowned cardiologist and professor. This endowed title supports the director of the East Carolina Heart Institute recognizes Dr. Rose’s exceptional contributions to cardiology and medical humanitarian work. Dr. Rose, who joined ECU Health in 1982 and the Brody School of Medicine in 1990, is celebrated for his dedication to patient care, teaching, and community service. Recipients of this professorship are expected to embody his ideals and passion for teaching, inspiring future generations of medical professionals.

“It’s an honor to be named to the Rose Professorship,” said Dr. Catanzaro. “This title not only recognizes Dr. Jack Rose’s work and legacy, which is focused on humanitarianism and the humanistic qualities of medicine, but it also allows me to highlight and continue his remarkable contributions. As program director, I perform hands-on teaching with trainees during cardiac procedures as well as teach didactic sessions. My primary role is to train the next generation of electrophysiologists to increase access to the patients of eastern North Carolina while maintaining a high standard of excellence in administration and leadership. This professorship is an opportunity to advance Dr. Rose’s legacy of teaching, administration and leadership, ensuring that his impact endures in these areas.”
Dr. Catanzaro completed his Doctor of Medicine with distinction in research at SUNY Downstate Medical Center, followed by an internal medicine residency and cardiovascular disease fellowship at North Shore University Hospital and a clinical cardiac electrophysiology fellowship at The Johns Hopkins Hospital. He also holds an MBA from the University of Florida. He is a Fellow of the American College of Cardiology, Heart Rhythm Society European Heart Rhythm Society and European Society of Cardiology. Dr. Catanzaro is actively involved with the Heart Rhythm Society’s Atrial Fibrillation Stroke Prevention Task Force and serves as vice chair of their Quality Improvement Committee. Nationally recognized for his work, Dr. Catanzaro has delivered invited presentations and chaired panels in the U.S., France, Italy, Germany, England, Romania and more. He also performed recorded procedures for the Heart Rhythm Society Scientific Sessions.
Dr. Catanzaro wanted to transition to an administrative role to broaden his impact beyond individual patients to the entire region and the cardiology division.
“We thought he was the best person for the future of cardiology,” said Dr. Mark Iannettoni, W. Randolph Chitwood, Jr, MD, Distinguished Chair in Cardiovascular Sciences, Brody School of Medicine at ECU and chief, Cardiovascular Service Line at the East Carolina Heart Institute at ECU Health Medical Center. “Dr. Catanzaro possesses a highly entrepreneurial spirit, bringing significant innovation to ECU Health. He has developed new techniques and devices in electrophysiology, advancing our capabilities in device management and patient care.”
The Rose Professorship comes with an endowment, managed by the university, to support ongoing and future initiatives in medical education and innovation. The endowment provides approximately $64,000 annually to advance the cardiology division’s educational and innovative efforts, supporting activities such as purchasing educational equipment, facilitating attendance at conferences, and other educational pursuits.
“The professorship facilitates innovation within the field by providing the necessary funding for new initiatives, such as introducing new devices,” said Dr. Catanzaro. “The goal is to use a certain amount of the endowment each year to support these innovations and to produce more trained physicians for the region. This helps establish our institution as a center of excellence and makes our advancements known.”
Dr. Catanzaro utilized part of the endowment to establish a two-year Electrophysiology Fellowship, admitting one fellow per year, starting this year. Electrophysiologists treat heart rhythm disorders and heart failure with electric devices inserted into the heart. As part of the fellowship, doctors will learn about pacemakers, defibrillators, implantation, ablations, leadless pacemakers, and left atrial appendage closure devices.
“This was one of the fastest fellowships from concept to establishment that we’ve ever done, which just goes to show you how much drive Dr. Catanzaro has,” said Dr. Herb Garrison, former associate dean for ECU’s Brody School of Medicine Graduate Medical Education. “It typically takes two to three years to establish a new residency or fellowship, and we did this in less than a year. That was a record time. And part of that had to do with Dr. Catanzaro and Alyson Riddick, who did an excellent job putting the application together.”
Dr. Jan Lopes is the first fellow in the Electrophysiology Fellowship at ECU Health. He learned about the new program through his cardiology fellowship leader in El Paso, Texas, and decided to join the fellowship because of Dr. Catanzaro’s strong vision for the program.
“Dr. Catanzaro’s enthusiasm for the program and education, along with the opportunity to shape the program for future fellows, attracted me to the fellowship,” said Dr. Lopes. “Despite being a new program, it feels well-established and highly developed. I feel incredibly supported in my role and am receiving top-tier training that rivals what is offered at major medical centers nationwide. We are utilizing cutting-edge technology and performing the latest procedures here at the medical center.”
Training doctors like Dr. Lopes with the latest technology and procedures is important for the future of health care. The need for well-trained electrophysiologists is increasing across the nation and here in eastern North Carolina, according to Dr. Garrison.

“The incidence of arrhythmias, along with the need for pacemakers and defibrillators, is rising as the population ages, making it a critical area of focus,” said Dr. Garrison. “Establishing residencies and fellowships serves two main purposes: recruiting top-tier faculty and creating a pipeline of skilled electrophysiologists. Faculty are attracted to institutions with trainees, and enhancing our program with excellent faculty was a strategic move by Dr. Catanzaro. This initiative ensures we have the necessary capability and qualified physicians to meet the growing demand for electrophysiology services.”
With the increasing demand for physicians and electrophysiologists trained to treat rural patients, Dr. Catanzaro’s efforts at ECU Health is paying off in the form of improved recruitment efforts.
“Dr. Catanzaro has successfully attracted numerous cardiologists,” said Dr. Iannettoni. “He has excelled at developing divisions within the cardiology department and navigating the integration of academia and medicine. His efforts have resulted in many of our graduates choosing to stay with us, which is a significant benefit of our program. We’re proud to retain our own trainees, ensuring continuity and excellence in our team.”
Each summer, teenagers from across eastern North Carolina dedicate a portion of their summer to serve their community at ECU Health hospitals across the region.
The VolunTeen Program is designed to teach students ages 15-17 the value of community service and to provide experiences that foster growth and maturity. The program runs from June to August and volunteers serve at least one shift per week at the hospital.
At ECU Health Medical Center, 122 teens completed 4,717 hours of service across 39 departments this summer. Sara Tingen, volunteer services coordinator at ECU Health Medical Center, said this year was very successful and they hosted their largest group of VolunTeens since the onset of the COVID-19 pandemic.
While the volunteers serve in many roles across the hospital, Tingen said patient transporting from one area of the hospital to another is one of the most important tasks.

“The (ECU Health) Cancer Center alone can see 400 people in one day,” Tingen said. “That’s a lot of time it would take for a nurse or other team members to transport a patient, they rely heavily on our transport volunteers. They can just pick up the phone, say, ‘Hey, I need this person to go here to there.’ And it’s done, they can move on to caring for their next patient. We’re proud to be a smiling face and someone patients can connect with while we help them get around.”
Emily Anthony recently finished her third summer in the VolunTeen Program, where she spent her time escorting patients, assisting the Volunteer Services team on projects and serving as a leader for other VolunTeens.
She said her favorite part of the VolunTeen Program is talking to patients and team members while also making connections with her fellow VolunTeens. Emily is entering her senior year of high school and wants to pursue health care.
“It’s really great to get experience in health care, because I want to do something in health care, maybe a nurse,” she said. “The first summer, I just thought it would be a good experience to do the VolunTeen Program but I just loved working in the hospital. I worked in a unit the first summer with all the nurses and I just loved it.”
Christopher Latimer is entering his sophomore year of high school and said he had a great experience in his first year as a VolunTeen. He’s already decided he’ll join again next summer.
He said he’s had an interest in nursing and getting first-hand experience working alongside nurses has helped him understand the day-to-day work of a nurse in a hospital setting.
“I was on 2 South most of the time and I worked in the Cancer Center as well,” Christopher said. “They were both good experiences. I was going around, asking patients questions and seeing if I could help them in any way. I helped the care partners, seeing if I could help out the nurses with anything, really. I’m thinking about nursing and I’m going to also try and do different areas the next time I VolunTeen to see more and just kind of see my options in health care.”

Chad Tucker, director of Volunteer Services at ECU Health Medical Center, said Christopher’s experience is exactly what the program hopes to give back to the local students who are spending their time serving their community.
“This program is an investment in our future,” Tucker said. “A lot of these students are going into college and they get a chance to see the hospital first hand. It’s so rewarding when you see former VolunTeens who are in medical school, or they’re nurses here, they’re respiratory therapists, they are in various capacities and they attribute part of their foundation to the VolunTeen Program. These young people are able to help team members and the patients we serve, but it also gives them help in their careers.”
The program also offers Leadership Sessions for VolunTeens, which gives them a chance to see unique areas of the health system and opportunities for skill development. In one session, the group visited the EastCare helipad, learned about the team, got to look around the inside of a helicopter and even saw a landing.
In another session, the Human Resources and Workforce Development team worked on resume building and shared interview tips with the VolunTeens.
“We have quite a few seniors who are coming up on college applications so if they’re interviewing for jobs or interviewing for scholarships, it just gives them a good perspective on how to navigate possibly their first interview as a young adult,” Tingen said.
We’re proud to support the VolunTeen Program at ECU Health Medical Center and select ECU Health Community Hospitals and we’re grateful for the teen who step up each summer to help us serve eastern North Carolina.
To learn more about the VolunTeen Program and other volunteer opportunities at ECU Health, visit ECUHealth.org/Volunteers.


