Renovations to the Pediatric Intensive Care Unit at the James and Connie Maynard Children’s Hospital, known as the PICU, provided a special way to honor some of the bravest patients.
“I’ve had families who their child has spent a significant amount of time in the PICU and asked, ‘How can we leave my child’s legacy on the unit?’” said Child Life Specialist Chelse Cudmore. “And I saw a picture of a wave and I was like, you know, a wave really represents patient and families stays while in the ICU as well as represents grief.”
One ECU Health nurse, Lacey Boldyrev, knows firsthand the journey of a family in the PICU. Her son Thaddeus was transferred to Maynard Children’s Hospital shortly after his birth.
“He was born in Jacksonville at Onslow Memorial Hospital,” said Boldyrev. “We had had just the normal pregnancy, normal ultrasounds, nothing special. I went to go get him and they told me that I couldn’t pick him up and I had to go back to my room and that the doctor would call me there. So I went back to the room and I waited. And the pediatrician that was in the hospital that day, she called and she said, ‘Your son has congenital heart disease and we’re going to send him to Greenville.’ He passed away on Christmas Day, December 2015. And I just felt like after he was gone, that there was that big empty hole.”
In the year that followed. Lacey felt called to serve the medical field and to care for patients just like her son. Her first choice upon graduating from nursing school was the PICU at Maynard Children’s Hospital. The admiration is mutual with the child life team honoring Lacey and choosing Thaddeus’ legacy to represent those who came before.
Cudmore reflected on the wave wall selection process.
“As we were talking about, how could we make this a significant thing? And Lacey, having a child who spent a significant amount of time and would have absolutely qualified for the wall and then him passing as well, and then her that kind of motivating her to want to be a nurse and our PICU. I mean it was really no question about it,” Cudmore said.
“I was asked by the child life team if I would want to put that on the wall,” said Boldyrev. “And I was completely honored to do that. It’s just a little bubble that it means a whole lot to me.”
Resources
Watch more ECU Health News videos
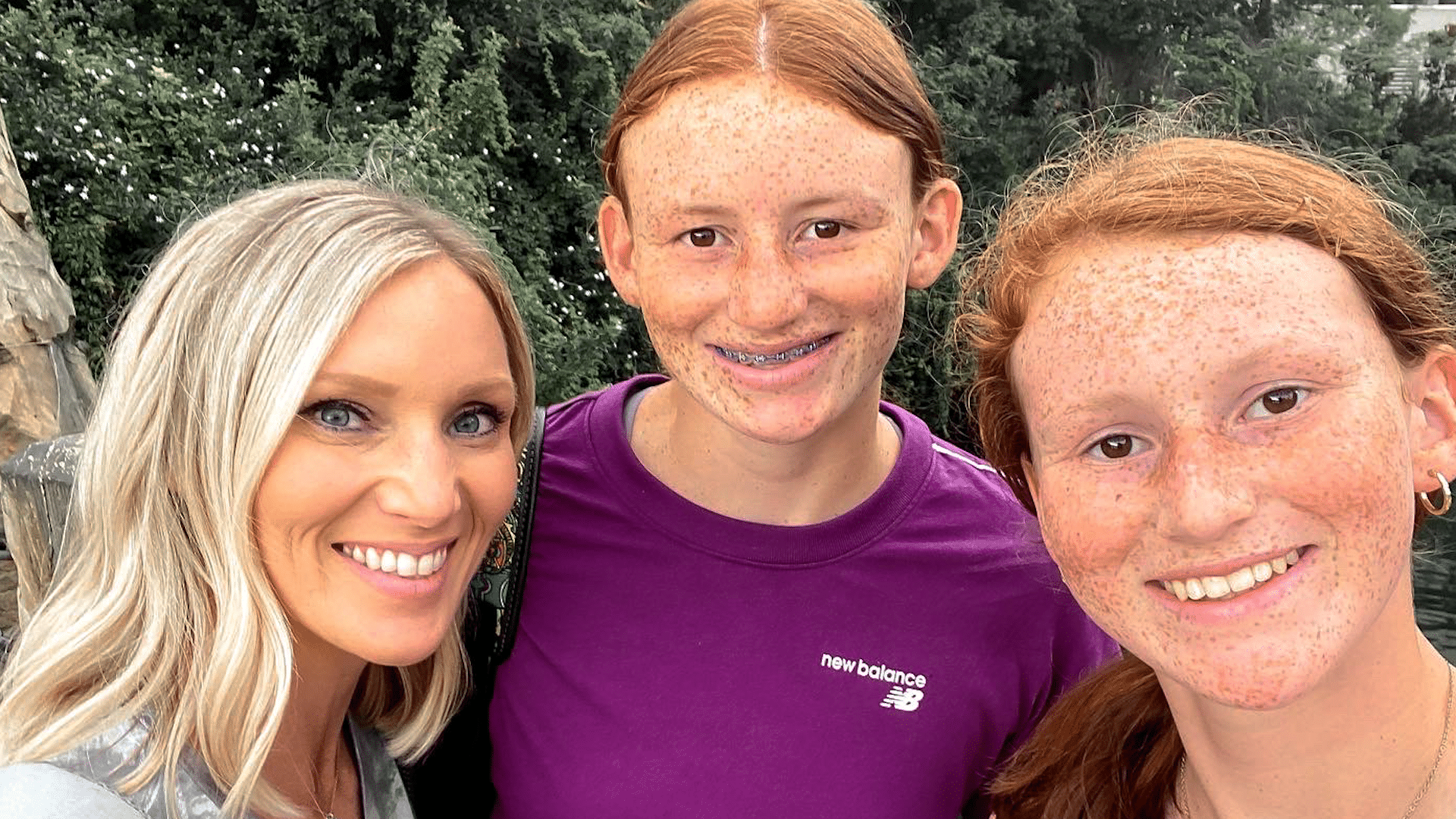
It started out as a typical holiday weekend for Dana Parker and her two daughters.
“We had plans to go hang out with my family the next day, for a cookout,” Dana said, about their plans last summer. “Fourth of July is a big holiday in our family.”
But overnight, those plans for a celebration quickly changed.
“I woke up a few times the next morning and thought, ‘Man, the house is really quiet. I’m surprised the girls aren’t up yet,’” Dana said.
Next came a horrifying discovery, as Dana found her oldest daughter Parker unresponsive on their living room floor.
“She’s just covered in vomit. She had definitely aspirated, I can hear it gurgling in her lungs,” Dana said, as she recounted the experience that day. “Her body is cold, I mean it is cold, stiff, she’s not responsive at all.”
Dana then finds herself reeling as first responders hone in on a possible cause. “They just kept saying, ‘Do you think it could be an overdose?’ They’re hooking her up to all these things and they just keep going back, like ‘Ma’am, she’s young, she’s healthy, all of these symptoms point to an overdose,’” she said.
Evidence found on Parker’s cell phone confirmed those suspicions. “In the course of about 25 minutes, she consumed almost 26 shots of alcohol,” Dana said.
“Depending on how old you are, how much you weigh, how much alcohol you’re ingesting, every child is different in terms of the effect it’s going to have on you,” Nicole Belcher, PA-C, a physician assistant at the James and Connie Maynard Children’s Hospital at ECU Health Medical Center (VMC).
In Parker’s case, she consumed enough alcohol for the care team at the Children’s Emergency Department at VMC to warn of an unknown outcome.
“They said, ‘At this point we don’t know if she’ll wake up. And if she does we have no idea what condition she’ll be in,’” Dana said. “She was already on borrowed time. I mean, it is literally by the grace of God that she was even still breathing at that point.”
Breathing then – and thriving now. While minor nerve issues persist, the multi-sport student athlete has made nearly a full recovery. And Dana is grateful for the care her daughter received.
“The little things that they do mean more than what they realize. Just the little kind words and taking the time to ask the questions and to say, ‘Hey, are you ok? Is there anything I can get you?’ I would just love to say ‘thank you,’” Dana said.
Now Dana wants other parents to learn from her family’s experience, and to consider how they talk to their children about the dangers of drinking.
“In her eyes, maybe she was drinking responsibly. She wasn’t out on the street, she wasn’t at a party, she wasn’t driving, you know – she’s in the comfort of her own home. She gets curious, she wants to experiment,” Dana said.
Experts agree.
“Bottom line, is to have the conversation. I think the earlier we walk about it, the better,” said Belcher. “The reality is, they are going to learn it from you, or they’re going to see it on social media, they’re going to see it on television, they are going to see it on the movies. Being able to have that open communication and being able to model safe behaviors with alcohol is the most important thing.”
Resources
April is Alcohol Awareness Month. If you or a loved one needs support, resources or treatment, the Substance Abuse and Mental Health Services Administration (SAMHSA) can help.
SAMHSA’s National Helpline is free, confidential and accessible 24 hours a day, seven days a week: 1-800-662-HELP.
They also offer an online treatment locator: https://findtreatment.samhsa.gov/
Watch more ECU Health News videos
Vidant Health team members and other community organizations came together to give patients at the James & Connie Maynard Children’s Hospital a Halloween experience to remember.
More than 20 cars drove by the Maynard Children’s Hospital with decorations on their cars and decked out in Halloween costumes. From the Mystery Machine to Star Wars and unicorns to super-dogs, everyone came out to put a smile on the face of Vidant’s smallest patients.
Alix Larrazabal is a Child Life student at the children’s hospital and helped organize the parade. She said the event was a success and seeing the reactions from the children was a highlight.

“It was honestly the most fun thing to see this come to life from the very beginning, months ago when we first started talking about it to seeing it now, how it turned out and how excited the kids were, it was amazing,” Larrazabal said. “I’m really happy with how it turned out.”
The ground outside the front entrance to the children’s hospital was decorated with Halloween-themed chalk as some East Carolina University students and children’s hospital patients brought out the spirit of the season. Many children showed off their Halloween costumes during the parade as well.
In years past, team members would dress up in their costumes and visit patients but COVID-19 brought about changes to the event. Last year was the first year of the parade-style Halloween celebration and it was a hit. Larrazabal said it’s important for the patients to have a safe and memorable holiday.
“This allows all the kids to safely come outside despite why they’re here at the hospital,” Larrazabal said. “It gives them a normal Halloween when they might not have gotten that inside the hospital.”
Larrazabal said the patients in the Maynard Children’s Hospital received a goodie bag with toys and art supplies as part of the event, whether or not they could make it outside to the parade.
On July 23, 2021, Cleere Reaves, 26 and a half weeks pregnant with her and her husband Will’s first child, headed to a regularly scheduled OB-GYN appointment with Dr. Kori Whitley for a glucose screening.
Cleere also had an ultrasound added to her visit, though it wasn’t totally necessary based on her scheduling.
“Praise God that was added,” Cleere said.
The ultrasound showed that something was wrong in the womb and it was time to move Cleere immediately over to Maynard Children’s Hospital at Vidant Medical Center. Dr. Whitley told Cleere and Will that they might be 90 hours from delivery, but their son would likely need to be delivered even earlier than that.
Will, a lawyer, began his nearly hour and a half drive from court in Onslow County while Cleere was admitted to the hospital for more ultrasounds and tests.

“Basically they figured out that they didn’t think it was safe for the baby to be in the womb anymore,” Will said. “And then the question was, well how long can he be in there?”
Sledge Strong

Photo courtesy of Reaves family
The time frame changed quickly as the team at Maynard Children’s Hospital reviewed the situation. Among several other factors, the ultrasound revealed that there was fluid around Sledge’s liver and near his brain, prompting doctors to be extremely concerned about a serious condition called hydrops, which can be life-threatening for premature babies.
Cleere was taken back about 2 p.m. that same day, July 23, to deliver her baby boy. As William Sledge Reaves was born, doctors could tell right away there was no sign of hydrops – the first big win in the life of a young fighter.
“It was really incredible because I can definitely tell you, there were angels in that room that helped him,” Cleere said. “I have no doubt that the Lord was very much present in that room and fighting for him.”
Sledge, with an appropriately tough name, weighed just 1 pound, 12 ounces at birth and was intubated right away to help him breathe. Intubating a child so small was another early win.
Sledge has been in the Neonatal Intensive Care Unit (NICU) at the Maynard Children’s Hospital since his birth and continues to get stronger and face the ups and downs of his young life.
Life in the NICU

Cleere and Will said they often hear the term “NICU rollercoaster ride” as they navigate this time with their newborn son. There are plenty of wins and challenging times, but Will and Cleere both said the support of team members in the NICU keep them on track.
“The providers are really helpful with that,” Will said. “If Sledge does have a tough day with one thing, they’ll say look at all these other great things that happened today. It’s hard but it’s a great reminder.”
“You’re kind of trying to coach your mind to say ‘Hey, this is part of the ride and sometimes what feels like a back step is not. His body is learning, all his systems are growing, he’s maturing and this is part of it,'” Cleere said. “It’s really just having such a sense of trust that they’re good at what they do, this is not their first rodeo, so Will can be the dad and I can be the mom – because that’s what Sledge needs and he can feel that from us I think.”
Trusting the care team is an invaluable part of life in the NICU, Will and Cleere agreed. They said it’s not natural to have a baby and leave the hospital to go home with their child staying behind.
The camaraderie with the care team and welcoming team members at every turn who care for physical and emotional needs make it easier to sleep at night and come back into the Maynard Children’s Hospital each day to spend time with their baby boy and focus on being parents.
“I think it starts when you walk into the Children’s Hospital,” Will said. “Whether it’s Jackie, Barbra, Lee or anyone out there at the front desk who are just inviting and welcoming and asking how Sledge is doing. It starts there and then continues to when you get back and see Mr. Lawrence, Natasha or MJ and they’re asking how he’s doing, how you’re doing and making sure you have everything you need.
“Then, his primary care nurses, nurse practitioners, doctors – there are too many to name, there’s so many of them – they just make you feel like ‘Hey, we’re all here, we’re all in this together.’ That’s amazing when you consider the fact that every single one of them has been working 12-hour shifts. Whether you walk in at 7 a.m. or 7 p.m., you’re getting the same positive attitude.”
Moving Forward
 Cleere and Will said Sledge still has a long road ahead of him and they are proud of their son for all he has overcome to this point. Cleere has a mantra that she heard early on in their experience and keeps close to her heart through their time in the NICU.
Cleere and Will said Sledge still has a long road ahead of him and they are proud of their son for all he has overcome to this point. Cleere has a mantra that she heard early on in their experience and keeps close to her heart through their time in the NICU.
“As a mom, you just pray that he rests and grows and I think about that all the time,” Cleere said. “He’s going to have his bumps, we’ve had them and we’ll still have some. Then we’ll have it where we coast a little bit. But as he rests and as he grows, he’ll be able to handle and fight whatever comes his way and he’ll move right along.”
Sledge has come off of his ventilator but still receives some respiratory support. His feedings are growing and so is he as he was up to 4 pounds, 6 ounces at nine weeks.
The Reaves family looks forward to everyone being home together, but until then Sledge will continue to live up to his tough name and fight with parents and a care team by his side.
As temperatures climb in late summer, it is critical to take precautions to keep everyone safe. Read more »