The new location will initially be open Monday-Friday and can accommodate up to 350 vaccine appointments per day. Vidant may adjust days and hours of operations for the clinic based on demand. Appointments are required and are already available at VidantHealth.com/Vaccinate or by calling 252-847-8000 — available from 8 a.m. to 5 p.m. seven days a week.
The Convention Center clinic will pause operations from April 7-12 due to an event hosted at the Convention Center. The Convention Center clinic will re-open April 13 to complete already-scheduled second doses only and will permanently close after all scheduled second doses are complete.
Effective April 8 and until further notice, all new doses in Greenville will be given at the Vidant Greenville Vaccine Clinic on Arlington Boulevard.
Although the vaccine offers great hope, Vidant encourages everyone to do their part to keep communities in the region safe from COVID-19: wear a mask, social distance and wash hands. Those who receive the vaccine should still practice these important safety measures.
Visit VidantHealth.com/Vaccinate for more information.
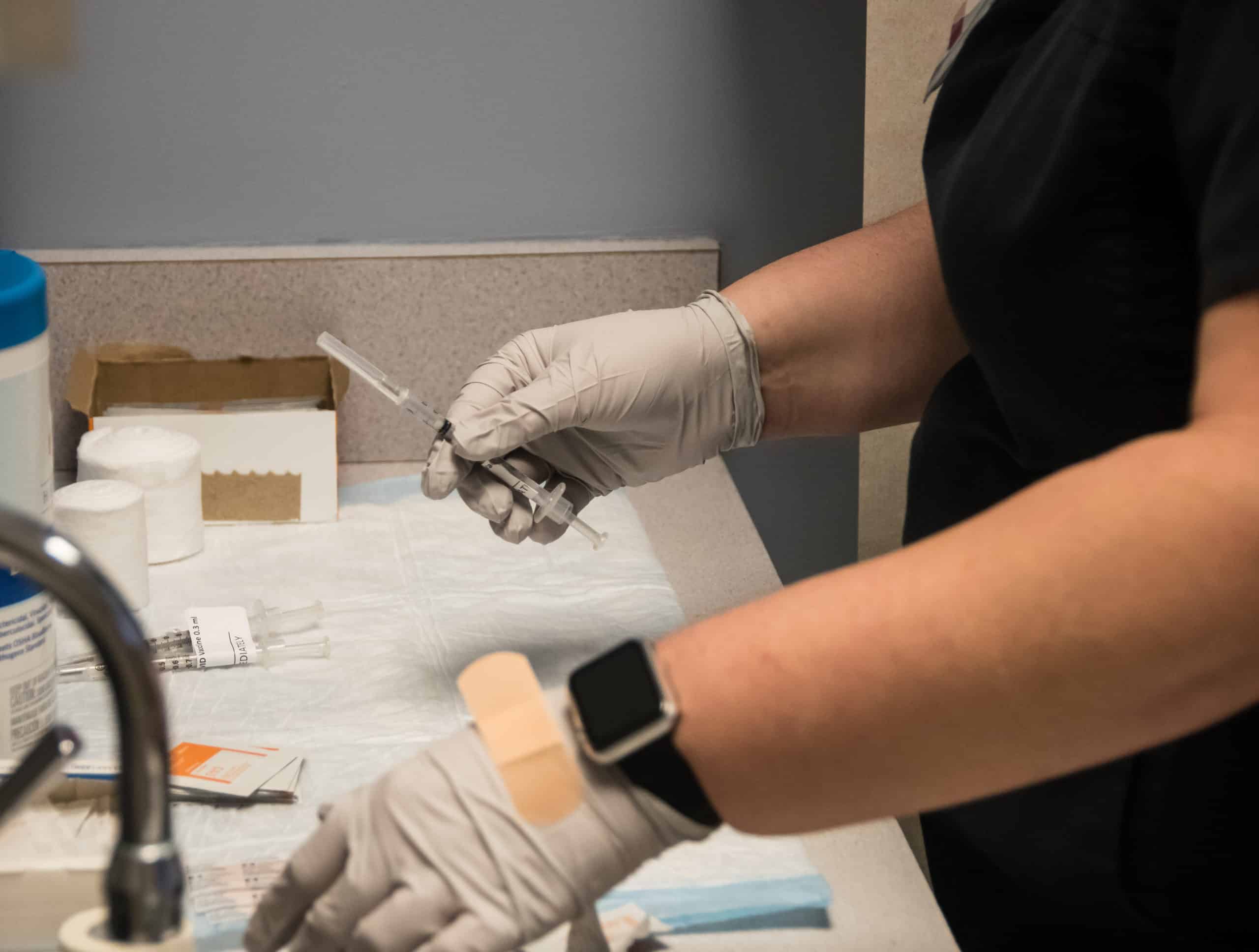
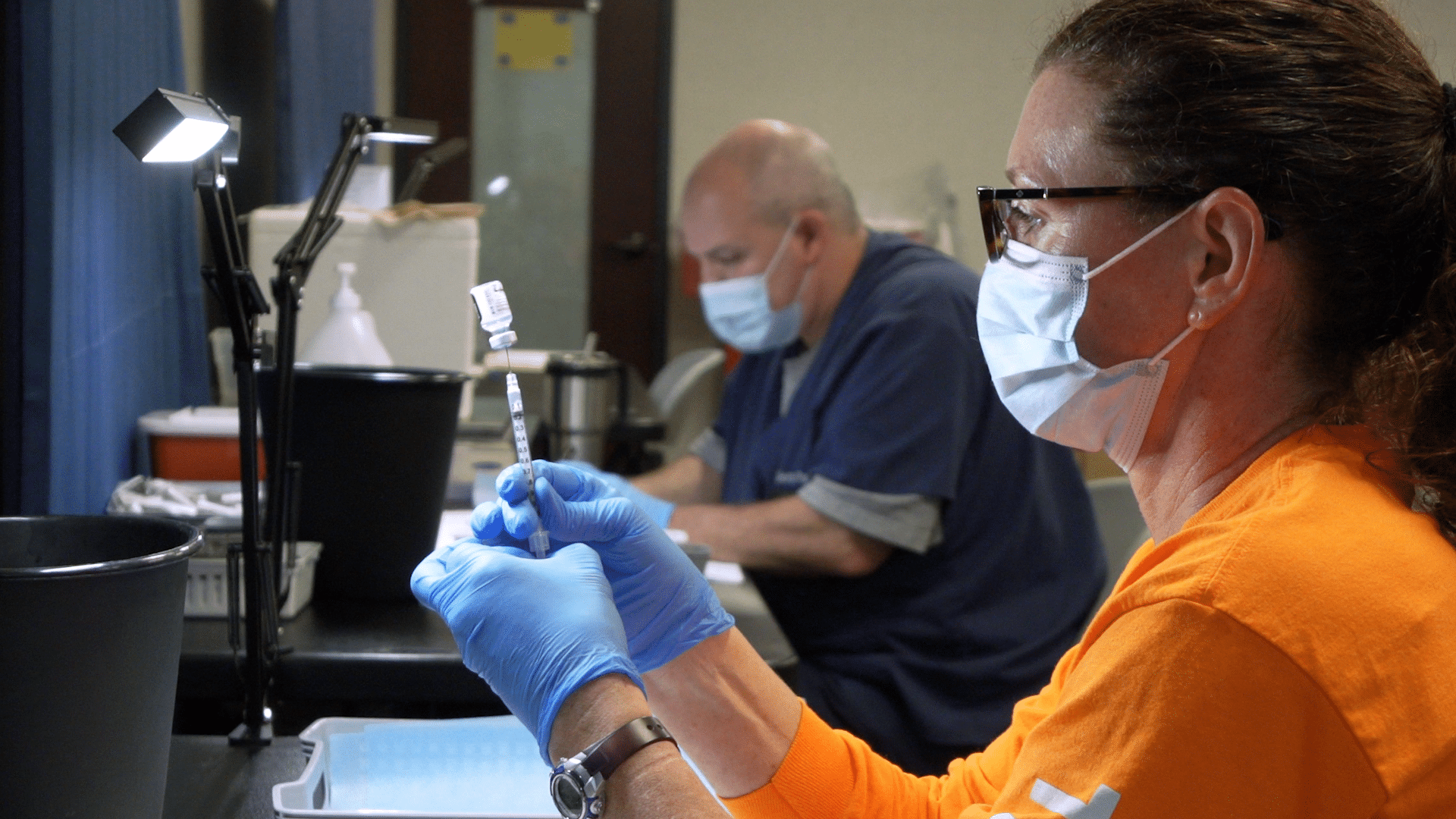
“I’ve never had an opportunity to do anything so important,” said Karen Harris, a pharmacy technician who has been on the job for more than 20 years. But what’s been required for COVID-19 is a first.
“This is our contribution to the public,” said Harris, who is part of a system-wide team helping prep vaccines at the Vidant / Pitt County Large-Scale Vaccine Clinic at the Greenville Convention Center.
“It’s kind of overwhelming to even think about being involved. And I’m grateful, so grateful that I can be a part of it – because this is a part of history,” she said.
The vaccines used at the convention center get their start at a pharmacy at ECU Health Medical Center (VMC) each morning. An early start — and a lot of planning and coordination — ensures vaccines arrive when and where they are needed across eastern North Carolina.
“We carry a tray of vaccines out, with 20, 30, 40 doses over to our vaccination area,” said Andy Grimone, assistant director of pharmacy at VMC. “The doses are all prepared and no one really knows how they got to that point.”
What’s not a mystery — the significance of their role and the doses of hope they deliver.
“The experts and the science behind it is saying the vaccine is working,” said Grimone. “So to know that what we’re doing here is making an impact in eastern North Carolina, is pretty awesome. And we couldn’t do it without this team.”
Harris agrees. “Everybody here is dedicated to what we’re doing. We all want to stop COVID-19 and the best way to do that is to vaccinate.”
For additional information on vaccine appointment availability and how to register for your dose of hope, please visit www.VidantHealth.com/Vaccinate.
The Vidant / Pitt County Large-Scale Vaccine Clinic at the Greenville Convention Center has helped thousands of people get their dose of hope in eastern North Carolina and beyond.
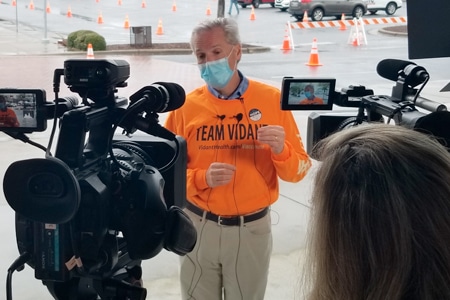
On March 19, the site served as a backdrop for a visit from North Carolina Governor Roy Cooper and other state and local officials.
“We see the data of where these vaccinations are going,” said Cooper. “Therefore, we know what we need to do and we know who is being left out.”
“We’re not done,” said Dr. Michael Waldrum, CEO of Vidant Health. “The game is still being played and we have to play all 60 minutes of this football game, and keep our communities safe.”
The site itself has been a monumental undertaking in support of the communities Vidant serves.
With support from team members and volunteers – to date, more than 70,000 vaccinations have been administered here and at other vaccination sites across the region.
“It’s been a tragic and a trying time,” said Dr. John Silvernail, director of the Pitt County Health Department. “It’s also been a time of great cooperation and a chance to learn from one another.”
While much great work has been done, state and local leaders remain focused on the path ahead.
“As Dr. Waldrum and Dr. Silvernail also said, we cannot spike the football too early,” said Cooper. “We know these variants are out there. We’ve seen them flare up in other countries, in other states. We don’t want that to happen in North Carolina.”
For the latest information on vaccine availability and eligibility, please visit VidantHealth.com/vaccinate.
 Ronald and Vivie Baseford’s hearts of service led them to each other.
Ronald and Vivie Baseford’s hearts of service led them to each other.
Ron began volunteering at Vidant Medical Center (VMC) around January of 2019 and has worked as a patient escort since. Vivie stopped working about two years ago and began volunteering at VMC in October of 2019. It didn’t take long for Vivie to catch Ron’s eye.
“About a week or two after I started, we passed each other in the hall,” Vivie said.
“We were wheeling patients,” Ron said. “Vivie and I passed each other in the corridors a couple of times and smiled and I said ‘Oh boy. I wish everyone had a smile like yours.’ And we just took it from there.”
There were lunches in the cafeteria at VMC before things became a little more formal. Dinners at Vivie’s house and date nights around town became the norm for them. They travel together, love watching movies and both find a piece of joy in spending time serving others.
When the pandemic began to intensify, the volunteering at VMC was halted but Ron and Vivie grew closer together. They decided to move in together and were married on July 7, 2020.
“We’ve been happy ever since,” Ron said. “We have the same interests. We love to travel, we love to go places in the car and visit places around here. We like to go up in the mountains and hike and see some of the waterfalls in that area.”
The time away from volunteering left some quality honeymoon time for the two, and they kept busy while away from helping patients, families and team members at VMC. They returned to volunteering about eight weeks ago, both on Monday mornings but in different areas of the hospital.
Vivie volunteers in the Eddie & Allison Jo Smith Tower and is happy to be back helping serve her community. Her love for the medical field goes back to her schooling days. While her first husband attended medical school, she sat in on classes with him and later worked with the Red Cross for a number of years.
“I always had an interest in that type of thing,” Vivie said. “When my first husband was stationed in Germany, I worked for the Red Cross and I volunteered. When he went into Rocky Mount to start his practice, I worked at the Red Cross also. I’ve been doing stuff like this practically all my life.”
She said she has enjoys interacting with patients and Vidant team members and the opportunity to be involved in health care again.
“When I was working, I worked as a teller at a bank, so I love people,” she said. “Just to be with people and help them, it makes me feel so good. Anything I can do for them, anywhere I can take them is just great. It’s very fulfilling to me.”
Ron, known as Mr. Ron around VMC, said he loves to meet new people and his role as a patient escort gives him the chance to talk to many different people each Monday.
“I like to talk to people,” he said. “While we’re walking, most of them are tense because they don’t know what they’re going to do and I certainly can’t help them with that but I talk to them about the weather and where they’re from and so forth and so on. We both very much look forward to going in on Mondays.”
Another benefit, Ron said, is the exercise he gets while escorting patients during his four-hour volunteering shifts. He said the exercise app he uses says he averages between five and six miles most Mondays while walking with patients and families through the hospital.
“It always pleases me because, all the people there, not only the patients but relatives that go with them sometimes, are all so very appreciative,” he said. “That’s always what makes it worth walking that six miles.”
“The people that work at the hospital are so appreciative of us, too, which really makes a difference,” Vivie added. “They make us feel like part of the team and they’re such nice people.”
If you would like to join Ron, Vivie and the other amazing volunteers at Vidant Health, visit VidantHealth.com/Volunteers/.
On Feb. 24, the Medical Intensive Care Unit (MICU), who have seen COVID-19 patients since the pandemic began, shared their journey on Hometown Healing. Myra Thompson, the nurse manager of the MICU at VMC, said it is a part of daily life for those on her unit.
“We can’t get away from it,” she said. “It doesn’t go away. It is in my head all the time, whether I’m here or not.”
Thompson said it has been difficult to be away from family, friends and loved ones during the pandemic, but it is necessary to keep them safe. She said she does not want to be the one who could possibly spread the virus to a loved one because she works with so many infected patients.
She said some days don’t even feel real when working on the unit with all she sees. But she knows there is work that needs to be done and people who need help.
“We have families too and we have things we are worried about at home and all kinds of other things and we come here,” Thompson said, “we are expected to put that aside and do what we do. It’s more than being a hero for working in this unit.”
For Thompson, having a team to go through the daily challenges with makes things better. The team has also benefited from a tranquility room on the unit, where they can take a break away from the unit and have a moment to breathe.
Another source of inspiration and hope for brighter days ahead, comes from the community.
“Just love us. Motivate us. It’s the hardest work that we’ve ever done, and we do it well,” she said. “Just don’t give up on us. Please wear your mask, please wash your hands. Please stay home unless you have to be out. Just keep loving and supporting us.”
Behind the teams directly working with patients to keep everyone safe during the pandemic is the Environmental Services Team (EVS). This group of team members was recognized on Feb. 23 for their efforts throughout the pandemic.
Natashia Scott, the EVS manager at VMC, along with about 265 other team members, work behind the scenes every day to ensure doctors, nurses, patients, visitors and everyone who enters the hospital doors are as protected as possible from the virus.
It is not a job without risks.
“We disinfect and clean patient areas in the hospital to make sure it is clean and conducive for our patients,” Scott said. “We have to touch every surface, like walls, and we have to take the curtains down. We’re touching every high-touch surface like light handles and door handles.”
COVID-19 fundamentally changed how the team had to do their jobs. She said what used to be a 30-minute job can now take an hour.
The pandemic also brought more technology to the team.
“We introduced solaris, which is a UV disinfect tool. It ensures all of the surfaces that we might not get are penetrated, sanitized and disinfected,” Scott said.
She said she knows it is a scary thing, to go into a room and clean room that a COVID-19-positive patient has been in. But with a community and hospital relying on them, they step up to get the job done.
Scott said as a manager, it is important that she stands with her team and makes them feel comfortable during challenging times. Her team is working together to help a community.
“Our housekeepers are the real heroes. None of this would be possible without them,” Scott said.
Watch and read more on the MICU team’s story and EVS team’s story.
There are key factors that impact heart health that everyone needs to be aware of to maintain a healthy cardiovascular system. These include monitoring blood pressure, knowing your cholesterol and getting enough exercise.
High blood pressure, also referred to as hypertension, occurs when the pressure of blood flowing through your blood vessels is consistently too high. According to the American Heart Association, nearly half of American adults have high blood pressure and many do not even know it.
Dr. Blase A. Carabello, chief of cardiology, Brody School of Medicine at ECU and ECU Health Medical Center, said, “High blood pressure is often a symptomless ‘silent killer’ because there are often no noticeable symptoms that accompany this condition. The best way to know if your blood pressure is in a healthy range is to get your blood pressure checked and monitor your blood pressure numbers regularly.”
Cholesterol levels can play a key role in heart health. It comes from two sources: the liver, which makes all the cholesterol you need, and the rest comes from foods from animals. Cholesterol circulates in the blood and as the amount of it increases in your blood, so too does the risk of cardiovascular diseases such as heart disease and stroke. When it comes to cholesterol, remember to check, change and control.
Another key factor influencing heart health is atrial fibrillation or “afib,” a quivering or irregular heartbeat that can lead to blood clots, stroke and heart failure and a shortened life span. Typically, people who have one or more conditions including high blood pressure, sleep apnea, underlying heart disease, and other chronic conditions including thyroid problems, diabetes and asthma may be at risk for atrial fibrillation. However, the single most important modifiable risk factor for afib is obesity.
The treatment goals of atrial fibrillation begin with diagnosis through in-depth examination from a physician. Based upon the diagnosis, providers may offer a variety of options including medication that usually entails the use of blood thinners, nonsurgical procedures, including electrical cardioversion to reset the heart to a normal rhythm and procedures that can block the area of the heart where blood clots form if patients are unable to take blood thinners.
“Being proactive about your heart health is the best way to be aware of potential problems,” said Dr. Carabello. “Eating a healthy diet, maintaining a healthy weight and being physically active can make a positive impact on blood pressure, cholesterol and atrial fibrillation, which will help maintain good heart health. Also, seeing your provider for screenings and check-ups is key to preventing problems before they arise.”
Even though the pandemic continues to make an impact on daily life in eastern North Carolina, Dr. Carabello encourages community members to continue to seek medical attention and to be knowledgeable about the procedures in place to make patients as safe as possible.
He said, “Heart disease did not take a break during the pandemic and any negative heart condition needs to be addressed in its earliest stages when the widest variety of treatments are available.”
For those who have experienced a major cardiac event, Vidant offers a Cardiovascular and Pulmonary Rehabilitation Program to help create a path forward. A team of respiratory therapists, registered nurses, exercise professionals, dietitians and a medical director guide patients through a program focused on exercise, nutrition and behavior modification to prepare and equip those in the program to continue physical activity and healthy lifestyle changes.
For more information about cardiovascular resources at Vidant Health, including treatments, screenings and technologies, visit VidantHealth.com/Heart-Vascular.
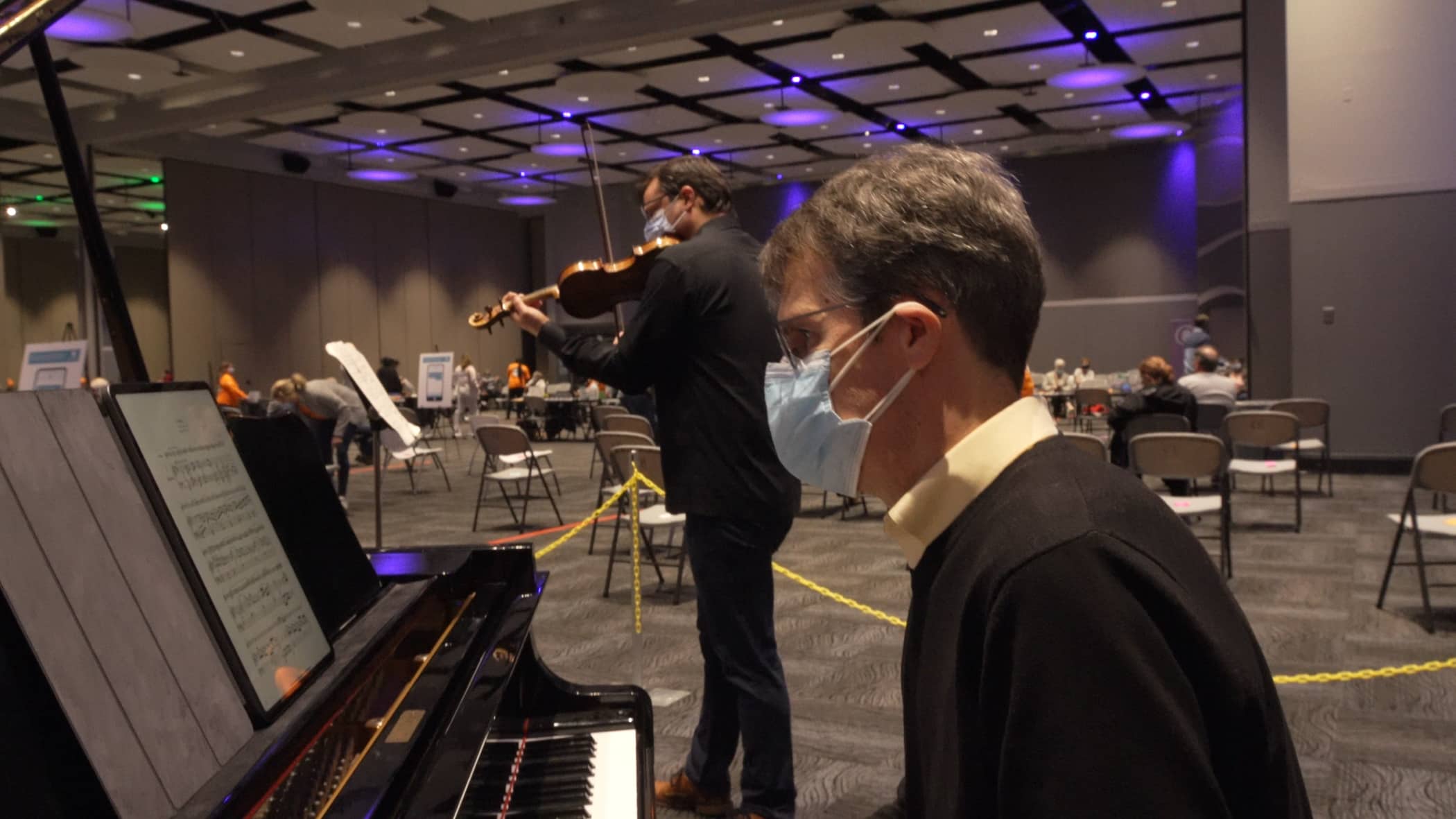
“Music therapy is not a new science,” said Vidant Chief Experience Officer Dr. Julie Kennedy Oehlert. “We know that music can calm anxieties and ease pain. Music from internationally renowned musicians provides a soothing experience for community members in the observation area after they receive their dose of hope.”
Four Seasons Artistic Director Ara Gregorian values the partnership they have built with Vidant. “Four Seasons is committed to bringing great music and musicians to as many people as possible, and I can think of no better way to do this during the pandemic than bringing musicians from around the world to regularly perform at the Large-Scale Vaccine Clinic,” Gregorian said.
“The beautiful, healing music gratefully provided by Four Seasons will forever be a part of the memories of those that receive their vaccine,” Dr. Oehlert said. Vidant and Four Seasons have partnered for years to bring musical experiences to patients at ECU Health Medical Center via live performances and video recordings featuring acclaimed Four Seasons musicians.
Dr. Oehlert said, “This collaboration is yet another demonstration of how our community comes together to support each other during this pandemic and other times of need.”
Vidant has vaccinated over 10,000 people thus far. For more information about vaccination appointments, visit www.Vidanthealth.com/vaccinate or sign up for email updates on Vidant’s vaccine efforts as new information becomes available.
The 72-year-old lifelong eastern North Carolina resident was among the first in line at the large-scale vaccination clinic, organized by Vidant Health and the Pitt County Department of Health.
“I hope and pray that some other people will come to realize that this is what we need to do,” Joyner said. “We need to get this vaccine.”
Vidant teams have been working around the clock to prepare to vaccinate more than 4,000 people in the first week.
“We knew this was going to be a big deal, we knew we were going to need a lot of help and expertise to do it,” said Dan Drake, PhD, RN, president of ECU Health Physicians & Ambulatory Services.
“There is a lot of pride with being able to offer this to people who are vulnerable, and frail and at risk,” said Vidant Health Chief Experience Officer Julie Kennedy Oehlert, DNP, RN. “And none of us take it lightly.”
“Many of the patients that we have immunized have been so gracious; in fact, many of them have talked about it like it’s a life-saving intervention and for many of them it may be,” said Drake.
As the COVID-19 pandemic continues to be unprecedented, so is the defense against it.
“This is the largest mass vaccination effort in the history of humankind; it’s the largest public health intervention we have ever faced,” said Drake.
“We all stood and watched these people that we’ve been preparing for, for a couple of weeks – and we were just like, ‘Yay! You’re here. We’re here for you! You’re here, we’re here. Let’s do this!’” said Oehlert.
It’s a rallying cry for a region – and a dose of hope for the communities Vidant serves.
Joyner, for one, agrees: “It’s a blessing, it’s a blessing that we’ve got this.”
Appointment information for eligible community members:
Beginning 8 a.m. Friday, Jan. 22, community members can view appointment availability by conveniently visiting VidantHealth.com/Vaccinate. The online appointment scheduler is the fastest and most convenient way to view and schedule an appointment. If internet access is not available or special assistance is required, community members may call 252-847-8000 — available from 8 a.m. to 5 p.m. seven days a week.. Due to large call volumes, community members are encouraged to only use this number if necessary.
Appointment information for those on the Pitt County Health Department Wait List:
A majority of the appointment slots in the initial phase will be allocated for the more than 8,000 people on the Pitt County Health Department wait list. Those already on the health department’s wait list will be directly contacted in the coming days and weeks by either email or phone. Individuals who are on the wait list are encouraged to check their email regularly and answer calls from a phone number beginning with 252-902. The Pitt County Health Department will stop accepting new wait list submissions effective today, Thursday, Jan. 21.
Vidant serves a region of 1.4 million people and appointments are expected to fill up quickly. The public is encouraged to be patient as it is expected to take months to vaccinate eligible community members. The initial goal is to administer more than 4,000 vaccines per week depending on the state’s vaccine allocations. Vidant and Pitt County will adjust appointment slots as needed, depending on vaccine allocations and other resources.
Vidant is also collaborating with other health departments and ECU to rapidly open more vaccine clinics across the region.
Although the vaccine offers great hope, Vidant encourages everyone to do their part to keep communities in the region safe from COVID-19: wear a mask, social distance and wash hands. Those who receive the vaccine should still practice these important safety measures. Importantly, a high number of COVID-19 patients are relying on Vidant for care and our team members are not immune from community spread. Please do your part to protect yourself and those around you.
Community members can visit VidantHealth.com/Vaccinate to view appointment availability, stay up to date on Vidant’s vaccine efforts and sign up for email updates.