On April 3, hospitals across the HonorBridge service area participated in a Pause to Give Life event to recognize the importance of organ donation.
A Donate Life flag was flown outside of ECU Health Medical Center to honor donors, their families, those who are waiting, and recipients who received the gift of life. Typically an outdoor ceremony, this year’s event was hosted in the Interfaith Chapel at ECU Health Medical Center due to inclement weather.
A moment of silence was held at 10:08 a.m. to signify that one donor can save eight lives.
Last year, ECU Health Medical Center had 31 organ donors and 75 organs were transplanted while 17 were sent out for research. The Medical Center had 49 tissue donors with 140 tissues recovered. Additionally, there were 80 eye donors with 98 corneas transplanted, 28 placed for research and 16 whole globes were recovered. This marked a record number of transplants performed at ECU Health Medical Center, including 130 kidney and kidney-pancreas transplants and 5 pediatric transplants.

During the event, Jenny Godwin, a former nurse at ECU Health Medical Center, spoke about the importance of organ donation. In February, Godwin donated a kidney to the 3-year-old daughter of a co-worker and said she felt called to step up for a friend.
“We knew I was going to be a match when I went in for testing. It was this feeling that me and my husband had and we felt very passionate about doing this,” Godwin said. “It’s the first time I’ve been able to experience peace throughout the whole experience so it was amazing.”
In her time at ECU Health, Godwin worked on transplant teams and she said it was a full-circle moment to be on the other side as a patient.
She said the opportunity to be an organ donor has given her a sense of accomplishment and fulfillment.
“People always say it’s better to give than receive and I can tell you it’s been an awesome feeling to know that I have given her life,” Godwin said. “I mean, she’s 3 years old and has her whole life ahead of her. It’s really awesome to know that I was able to be a part of that.”
Godwin said she was tired for the first couple weeks after surgery but a little more than a month removed, she’s feeling great and back to her old self – including running around with children of her own.
Dr. David Leeser, chief of transplantation at ECU Health Medical Center, also spoke during the event and said it’s important to recognize those who have said “Yes” to organ donation, whether it is as a living donor or a donation after a person has passed. He also said with 100,000 patients across the country and 3,000 patients here in North Carolina waiting for a donation, it’s crucial to raise awareness of the need for organ donation.
He said transplantation takes a village and none of what he does as a transplant surgeon is possible without the many teams working to make each surgery possible.

“The transplant team is huge – you have organ procurement organizations like HonorBridge, they spend 24 hours a day, seven days a week ready to come to hospitals, meet with families and get donors,” Dr. Leeser said. “Once they have the donor, they arrange having surgeons available to take out the organs for transplant and figure out who the organ is going to and all the pieces that go into getting the organ to the recipient hospital before the transplant even occurs. Each transplant program has social workers, dietitians, nurses and physicians – everyone is so crucial to make sure a transplant is successful. We stand on the shoulders of so many dedicated professionals that do the hard work of getting our patients ready to go to the operating room.”
At ECU Health, we are grateful for the over five million North Carolinians who have registered as organ, eye and tissue donors. We also appreciate the efforts of our North Carolina Department of Motor Vehicles partners, who ask the questions every day as part of their job. Together, we are united in a mission to save and heal lives and create a culture where donation becomes a fundamental human responsibility.
Those interested in learning about organ donations or interested in becoming an organ donor can visit ECU Health’s donor registration portal or the Donate Life website for more.
Read more
When Lauren Moore, a fourth-year student at the Brody School of Medicine at East Carolina University, begins her residency training at ECU Health Medical Center in July it will mark the beginning of a new chapter in her deeply personal family medicine journey. With a love for health care passed down from her parents, including her late mother, Moore’s next step is another toward her ultimate goal: making a difference in the lives of countless eastern North Carolina community members.
Moore’s experience with health care goes far beyond her medical school training. Her father is a physician’s assistant and she was naturally drawn to the connections he made in the community. Growing up in Farmville and attending school in Greenville, she recalls countless instances where he was stopped in places like the grocery store, catching up with a long-time patient or offering helpful advice.
“Growing up, people would come up to us and be like, ‘Mr. Eddie, how are you doing?’ I’d ask, ‘Dad, who is that?’ He’d say, ‘Oh, a patient that I’ve had for ten years now.’ I would think, ‘That is amazing,’” Moore said. “And even recently, ever since I’ve matched at ECU Health, just within the past few weeks, I’ve had several people from my Bible study at my church that have said, ‘You know, I’ve been needing to get a primary care doctor.’ And I’m like, ‘I’m your person!’ It just feels good that they trust me enough to one day be their doctor and to have those personal connections and be able to serve them to make sure their health is taken care of.”

She also experienced the health care profession from the patient perspective through her mother’s cancer journey. When Moore was seven years old, her mother was diagnosed with breast cancer for the first time and was declared cancer free after about a year of treatment.
Then, six years later, she was re-diagnosed with metastatic breast cancer, which spread to her liver and brain. Moore’s mother passed in June of 2010. She reflected on the care her mom received and how the care teams went above and beyond for patients and families alike. Moore learned what it meant to be a compassionate care giver and she said she’s prepared to bring that same compassion to her future patients.

“Seeing her go through that and seeing the way that her physicians were able to play such a vital role in not only her life, but also my family’s life and making sure that we were OK even after the fact,” Moore said. “If my dad was walking through the hospital, my mom’s physicians would check in on him and ask how he was doing and if he needed anything. So it wasn’t that they were just taking care of my mom as a patient, but they were also taking care of the rest of her life, too. That had such a tremendous impact on me. My goal is not only to care for my patients the same way my dad does, but also to make the families feel the same way that those physicians made me feel.”
Brody Matches
Moore is one of 77 Brody medical students poised to begin their residency at hospitals across the country, following an emotional Match Day ceremony in March and commencement in May. For Moore, who wants to practice family medicine in the region in which she grew up, matching to ECU Health Medical Center was always the goal.
“Being a medical student at Brody and seeing the patient population that we have here, I think that’s really what drew me to ECU Health,” said Moore. “The fact that it serves patients throughout the 29 counties in eastern North Carolina who otherwise wouldn’t have a primary care provider or a Level I trauma center if it wasn’t for us. I was drawn to the educational opportunities given the uniqueness of our patients and everybody in the residency program is just so welcoming and nice. I know it’s family medicine, but it is also like a family there.”

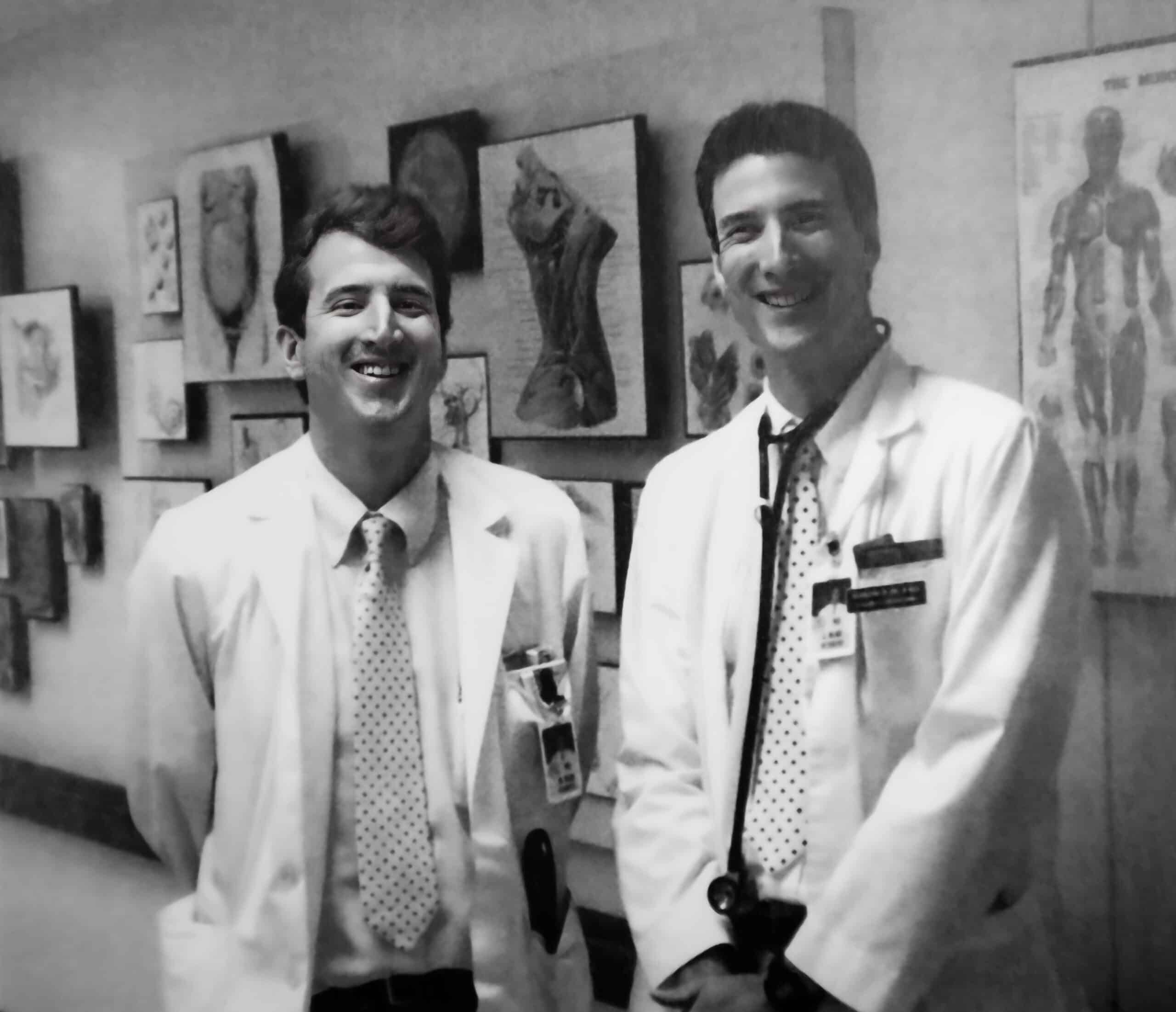
Photo Courtesy of ECU News Services
Match Day at Brody marked a milestone for the Class of 2023, whose medical school journey included the historic events of learning through the COVID-19 pandemic and the integration of Brody and then-Vidant Health, which became ECU Health in 2022.
Match Day is arguably the pinnacle of medical school, when students discover where they will train during their residency, surrounded by friends, family and Brody faculty and staff who have guided them over the years.
The Class of 2023 is a snapshot of Brody’s mission to serve the state. The 77 members of the graduating class represent more than 25 North Carolina counties, from Buncombe in the west to Pasquotank in the northeast.
ECU Health Medical Center had an excellent Match Day, according to Dr. Herb Garrison, associate dean for Graduate Medical Education, with 98 medical students matching into the 12 main residency programs. Twenty-six of the students, or 27%, will graduate from North Carolina medical schools, including 16 students from ECU’s Brody School of Medicine. Brody’s most recent class features the most medical students who will begin their residency at ECU Health Medical Center in July.
“We’re thrilled for this class to start their residencies across the country and we’re especially excited about how many will be staying with us at ECU Health Medical Center,” Dr. Garrison said. “This group had their first year of medical school disrupted by the start of COVID and I’m so proud of the way they supported each other through that experience. I’m just excited, as I am every year, to see these skilled and highly trained students start their careers and share everything they’ve learned here with the rest of the world.”
A Rural Legacy
Dr. Mott Blair’s journey to his post as a physician at ECU Health Family Medicine – Wallace is not totally unlike Moore’s. Dr. Blair’s father was a doctor in Duplin County beginning in 1949.
Dr. Blair shared that his father was a primary care physician who also took up obstetrics and did home deliveries for many families. Seeing his father’s connection with patients and families in his home town lead him directly to his own career in medicine.
He attended the Brody School of Medicine – then called ECU School of Medicine – and graduated in 1987, alongside his brother. He matched with ECU Health Medical Center – then called Pitt County Memorial Hospital – and began practicing in Wallace after his three-year residency. He said his decisions to attend Brody, make Greenville his first choice for residency, establish a practice in his rural hometown and eventually partner with the ECU Health system have all been rewarding for himself and beneficial for the patients he serves.
“I feel like the mission of the medical school was a mission that I wanted to take on and I think I’ve been successful in doing that,” Dr. Blair said. “I think the credit in being able to do that goes to the medical school and now the medical center as well. I really think that what we’re doing now, particularly as we support practices across the eastern region of the state, is a crucial thing to put in place, because health care in rural North Carolina is so difficult and we need to have true rural primary care.”
Dr. Blair said that he knows his time at Brody prepared him well for the challenges of residency and he has seen the same for other Brody graduates whom he’s connected with as residents.
For first year residents, he said it’s a new kind of challenge and learning curve, just like those experienced in the first year of medical school and the first year of rotations, but sticking to the same habits that got residents where they are will make all the difference.
“Work hard, study hard. Getting through residency the first year is a lot of hard work,” Dr. Blair said. “So enjoy it and it will go by fast and it will seem like a distant memory pretty quickly. Coming out of Brody, you’ll be well prepared. I found the preparation for me was excellent. You have to be patient with the pace in medicine. It changes rapidly and has really changed a lot since I’ve been in practice and continues to do so.”
In line with the Brody School of Medicine’s mission to increase the number of primary care physicians who serve North Carolina, 52% of the 2023 Brody class matched into primary care residencies — including obstetrics and gynecology — and 44% matched to residency programs in North Carolina.
Moore and Dr. Blair are just two examples of the importance of the Brody School of Medicine and ECU Health connection. Developing high-quality, compassionate physicians for a region in need helps meet the organizations’ combined mission to improve the health and well-being of eastern North Carolina.
“Developing great primary care providers for rural areas is at the core of what we do at Brody and within ECU Health” said Dr. Michael Waldrum, CEO of ECU Health and dean of Brody. “Working as rural health care professionals is hard but we’re working together to train doctors that will care for the whole patient, their physical and emotional health, and I think we’ve been successful in doing that. We have students, professors, residents and doctors that really understand that side of health care and their work in that space leaves a legacy that we can all be proud of.”
Greenville, N.C. – ECU Health is pleased to announce Dr. Richard Medford, MD, FAMIA, FRCP(C), as ECU Health’s first Chief Medical Informatics and Digital Health Officer (CMIDHO) following an extensive national search and interview process with stakeholders from across the organization. Dr. Medford officially joined the health system on May 1, 2023.
 “Over the past several years, we have seen the importance and value of telehealth and other technology in patient care, and we recognize the need to be nimble to work within the digital evolutions and innovations we are seeing in and around the health care industry,” said Dr. Michael Waldrum, ECU Health CEO and dean of the Brody School of Medicine at East Carolina University. “I am pleased to welcome Dr. Medford to ECU Health and feel strongly that his background in health care technology innovation will serve our patients and the region well. As we continue to define the future of ECU Health, Dr. Medford’s collaborative and evidence-based approach will be assets in helping us to realize our vision for those we proudly serve.”
“Over the past several years, we have seen the importance and value of telehealth and other technology in patient care, and we recognize the need to be nimble to work within the digital evolutions and innovations we are seeing in and around the health care industry,” said Dr. Michael Waldrum, ECU Health CEO and dean of the Brody School of Medicine at East Carolina University. “I am pleased to welcome Dr. Medford to ECU Health and feel strongly that his background in health care technology innovation will serve our patients and the region well. As we continue to define the future of ECU Health, Dr. Medford’s collaborative and evidence-based approach will be assets in helping us to realize our vision for those we proudly serve.”
In this newly-expanded role, Dr. Medford will collaborate with executive and clinical leaders to develop and execute strategies to optimize and transform care delivery models and the clinician-patient experience through the strategic use of the electronic health record (EHR), digital tools, advanced technologies, services and processes.
As part of his work at ECU Health, Dr. Medford will continue to practice medicine, allowing him to more fully understand and relate to the challenges and opportunities in the digital environments and frameworks our clinicians provide care within. He has also received a faculty appointment within the Brody School of Medicine with a continued focus on research where he will help serve as a bridge between the academic, medical, information systems and research arenas.
“I am grateful for the opportunity to join ECU Health and to collaborate with the teams here to bring innovations that improve the health status of the patients we proudly serve,” said Dr. Medford. “The unique challenges we face in this vast rural environment require unique, cutting-edge solutions. I look forward to serving on behalf of the people of eastern North Carolina.”
Originally from Toronto, Ontario, Canada, Dr. Medford received his MD from Jefferson Medical College in Philadelphia. He completed an internal medicine residency at Queens University in Kingston, Ontario, and fellowships in infectious diseases from the University of Ottawa and clinical informatics from Stanford University School of Medicine.
Dr. Medford is triple board certified and the recipient of numerous honors, awards and grants. He has proven to be a transformational and strategic leader who understands the importance of leveraging digital technologies and the EHR to drive health system success, enhance patient safety and quality, improve provider efficiency, decrease provider burnout and augment research endeavors.
Students at A.G. Cox Middle School in Winterville learned about the dangers of vaping tobacco or other substances and drug use during an event hosted at the school on Feb. 28.
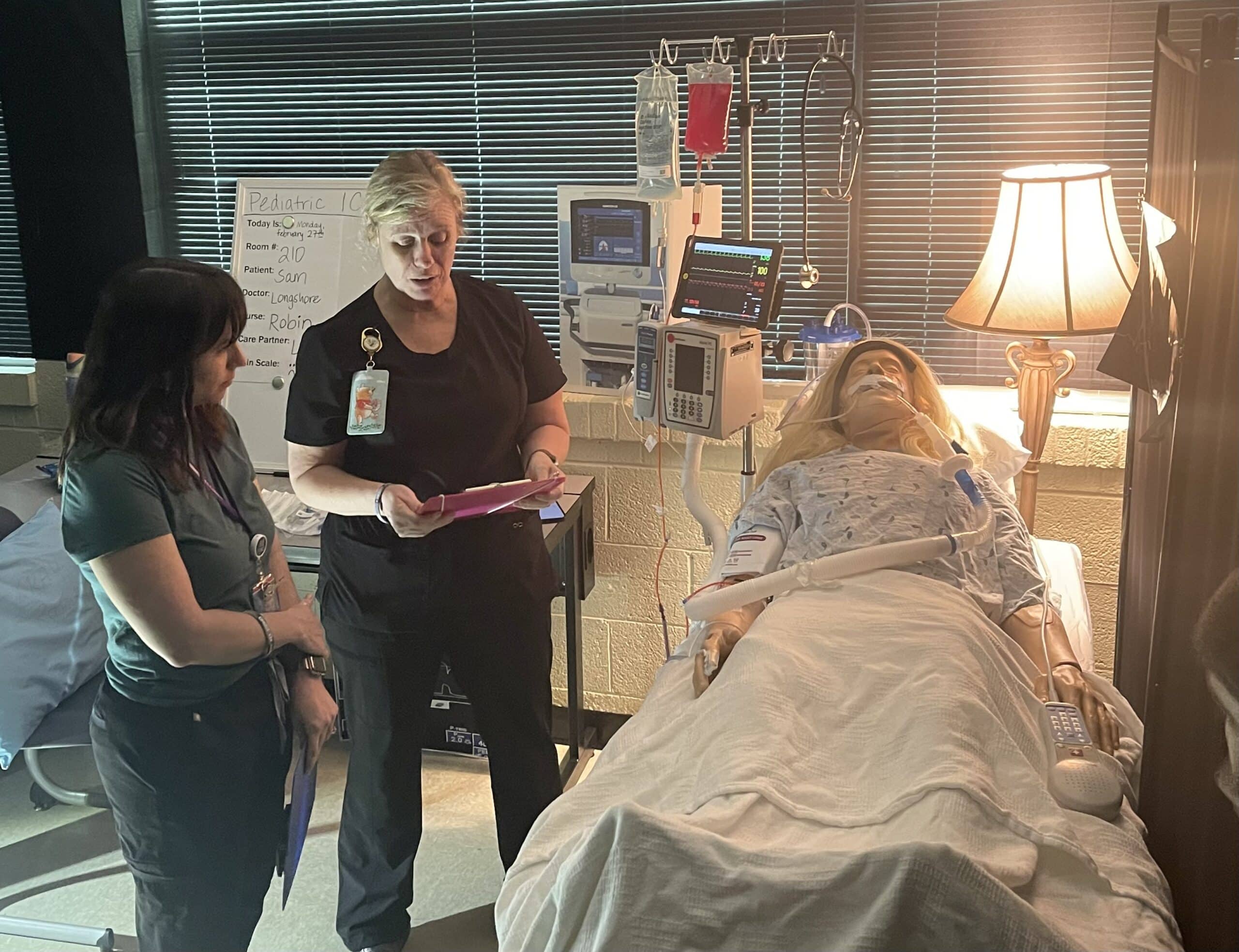
Pitt County School nurses, ECU Health team members and volunteers, and local high school students acted out two different scenarios for the A.G. Cox students, who are in grades 6-8, to show how quickly things can go wrong.
In one scenario, a student at a party takes a gummy from a friend, which turns out to be laced with drugs. The student then falls critically ill from the effects of the drugs.
In another, a student is taken to the hospital after using a vape they were told did not have tobacco in it, but instead was filled with an unknown drug.
Emerson Fipps, a senior at South Central High School in Winterville, helped act out the first scenario with another student and an ECU Health volunteer. She said she’s proud to support events where she can help other young people set themselves up to make positive decisions.
“Middle school is really where everything starts to come up,” Fipps said. “Teenagers are just trying to find themselves so they’re getting into things that they shouldn’t. They’re not really fully educated about everything these destructive decisions could affect. It’s really good for them to start hearing about it young because when they’re in these situations, they’ll already have the information.”
Tiffany Thigpen, the Region 10 tobacco prevention and control coordinator for the Pitt County Health Department, said schools across the country are seeing an increase of students vaping and using gummies and other drug-infused edibles.
The National Poison Data System reported 3,054 cases of pediatric edible cannabis consumption in 2021, a large increase from 207 cases in 2017.
Thigpen said one of the most important things parents can do to keep their children safe from tobacco and drugs is talk to them.
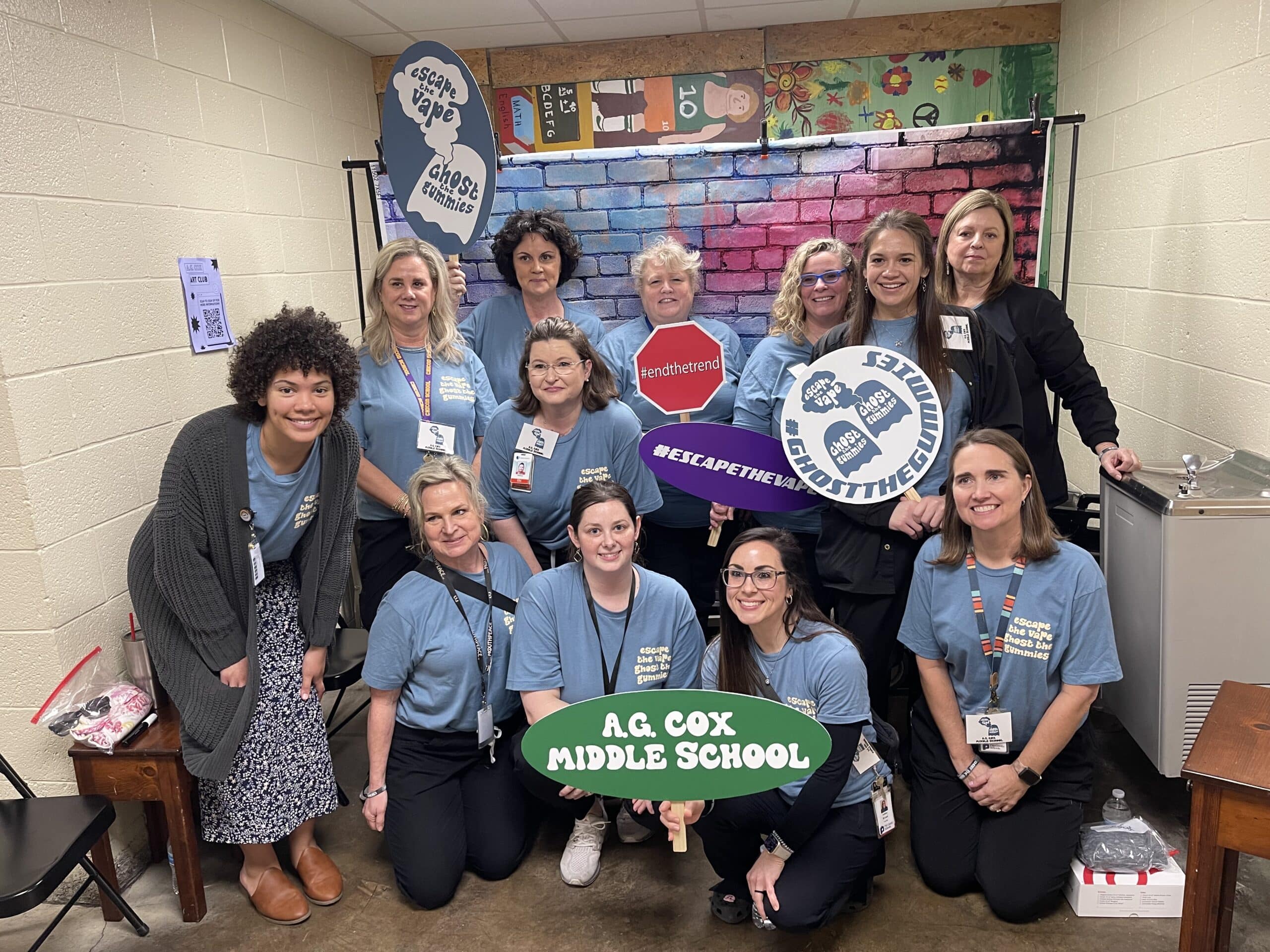
“Talk to your children, let them know that these things are not safe,” Thigpen said. “Let them know that it is OK to say no. Talk to them about refusal skills and ways to say no to their peers. Let them know they can talk to you about what they’re experiencing. If they do use these products, share the dangers with them and ways to stop.”
Thigpen said the county is working to get as much information as they can into the hands of students about the dangers of drugs and vaping to help stop addictions before they begin.
Laurie Reed, manager of school health services at ECU Health, said partnerships make all the difference for events like the one hosted at A.G. Cox Middle School.
“Our school board and our school health advisory committee are very supportive of programs like this in our school system,” Reed said. “We just hope we’ll be able to offer more of them. It’s a great collaborative effort and it takes a lot of effort on the part of our school nurses, Injury Prevention, our health department, but it’s a great collaborative opportunity for our community.”
Greenville, N.C. – With a significant decrease in demand for COVID-19 testing, combined with the extensive availability of other convenient options such as at-home tests, community health departments and physician practices, ECU Health is closing its COVID-19 testing sites effective Friday, July 29. This includes testing sites at 13 ECU Health medical group clinics (formerly Vidant Medical Group) and the drive-thru testing site in Greenville. This decision comes as North Carolina nears the end of the COVID-19 state of emergency, which will be lifted mid-August.
From the onset of the pandemic, ECU Health has placed the health, well-being and safety of eastern North Carolina at the forefront of our COVID-19 response. Once COVID-19 testing capabilities were established, ECU Health heavily invested in building a robust, state-of-the-art testing program. Since launching the testing sites across the region, we have been able to monitor the spread of COVID-19 and its impact on our region as well as share this valuable data with community members.

ECU Health established the Greenville drive-thru COVID-19 testing site and regional testing sites when other convenient testing options were not available. These testing sites, which have helped mitigate the spread of COVID-19, served our communities for almost two years. Throughout this time, ECU Health resulted more than 800,000 total tests.
Regrettably, closing the testing sites impacts the employment of 141 team members across the region who were specifically hired to support the health system’s COVID-19 response. ECU Health is providing human resources and talent acquisition support to all team members who are interested in applying for open positions for which they are qualified for within the health system. This includes those who are working in part-time, full-time and supplemental roles related to the system’s initial COVID-19 response efforts.
ECU Health will continue to provide COVID-19 testing, if needed and by appointment, for patients during their scheduled visits at ECU Health primary care offices. Testing will also be available as needed in the inpatient setting.
The community should continue to follow the usual protocols when sick, and seek appointments with their primary care providers. Those strictly seeking a COVID-19 test should not visit the Emergency Department and should instead contact their primary care office or seek alternative testing options.
To find a COVID-19 testing location closest to you, please visit NCDHHS’ Community Access Points website at www.covid19.ncdhhs.gov/FindTests.
Greenville, NC – March 14, 2022 – As Vidant continues to respond to the evolving COVID-19 pandemic across North Carolina, we are taking steps to ensure the safety of all. Vidant remains vigilant with its screening process for all visitors, entry requirements and visitor restrictions by department.
In response to decreased community spread, Vidant is carefully expanding visitation across the system, including for COVID-positive patients. Effective 8 a.m. Wednesday, March 16, Vidant will adopt the below visitor guidelines. Visitors must wear surgical masks provided at screening stations or personal N95/KN95 masks as long as they are clean, intact, without a valve and have no visible gaps.

Despite the encouraging trend of cases, it remains vitally important for community members to continue to practicing safety measures such as washing hands, wearing a mask and avoiding large gatherings.
For the latest information on Vidant’s visitor restrictions, please visit VidantHealth.com/VisitingVidant.
This is an evolving situation, and Vidant continues to monitor the spread and examine local data, including COVID-19 cases in our region and in hospitals, and will adjust visitation restrictions accordingly.
Vidant strongly encourages visitors to consider virtual visitation options such as FaceTime and phone calls. Assistance with virtual visits, including iPads for patients without the necessary technology, is available on request. Virtual visitation is the safest way to stay connected with a loved one.
Patients should limit their belongings to a few key items and refer to the below tips:
- Bring your phone, tablet or other electronic device to connect with family members
- Limit clothing to clean undergarments and one outfit for discharge
- Wear or pack non-slip shoes
For the latest information on Vidant’s visitor restrictions, please visit VidantHealth.com/VisitingVidant.
Greenville, NC – March 1, 2022 – As Vidant Health continues to respond to the evolving COVID-19 pandemic across North Carolina, we are taking steps to ensure the safety of all. Vidant remains vigilant with its screening process for all visitors, entry requirements and visitor restrictions by department.
In response to decreased community spread, Vidant is carefully expanding visitation in most clinical areas across the system, including for COVID-positive patients. Effective 8 a.m. Wednesday, March 2, Vidant will adopt the below screening process, entry requirements and visitor guidelines. Visitors must wear surgical masks provided at screening stations or personal N95/KN95 masks as long as they are clean, intact, without a valve and have no visible gaps.

Despite the encouraging trend of cases, it remains vitally important for community members to continue to practicing safety measures such as washing hands, wearing a mask and avoiding large gatherings.
For the latest information on Vidant’s visitor restrictions, please visit VidantHealth.com/VisitingVidant.
This is an evolving situation, and Vidant continues to monitor the spread and examine local data, including COVID-19 cases in our region and in hospitals, and will adjust visitation restrictions accordingly.
Vidant strongly encourages visitors to consider virtual visitation options such as FaceTime and phone calls. Assistance with virtual visits, including iPads for patients without the necessary technology, is available on request. Virtual visitation is the safest way to stay connected with a loved one.
Patients should limit their belongings to a few key items and refer to the below tips:
- Bring your phone, tablet or other electronic device to connect with family members
- Limit clothing to clean undergarments and one outfit for discharge
- Wear or pack non-slip shoes
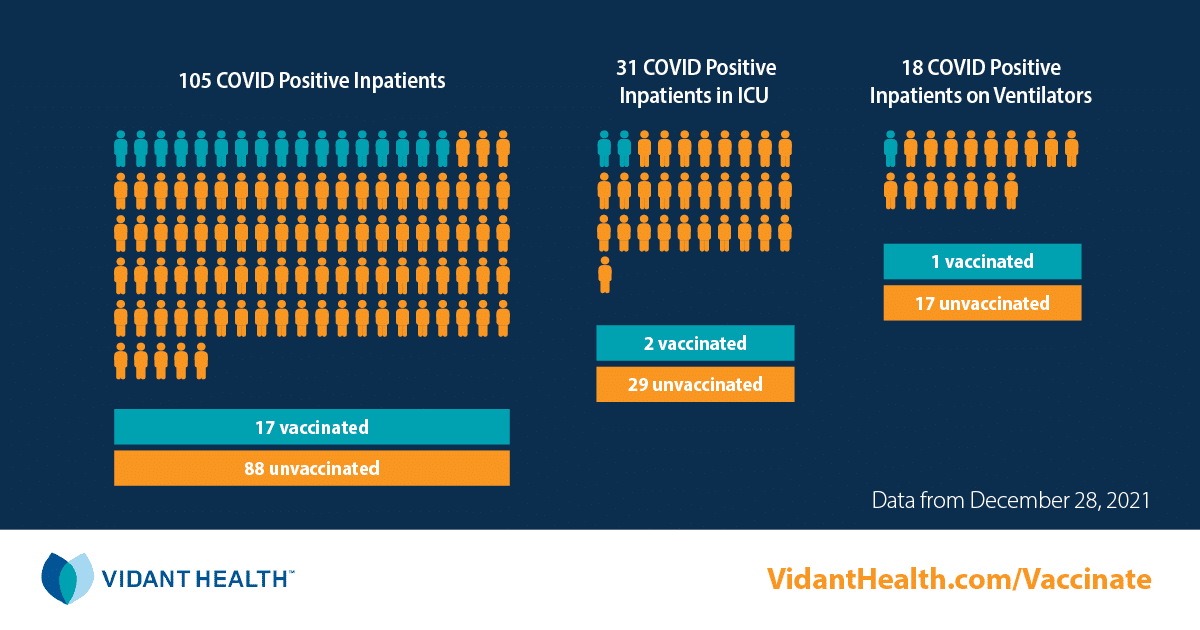
Greenville, NC – Dec. 29, 2021 – As Vidant Health continues to respond to the evolving COVID-19 pandemic and the increasing spread of the Omicron variant, we are taking steps to ensure the safety of all. In consultation with infectious disease experts and based on current trends, Vidant is proactively updating visitor guidelines for the health system and adjusting the reopening of the Wellness Center – Greenville.
Vidant continues to strongly encourage masking, vaccinations and boosters, as we all work together to combat COVID-19.
Visitor Guidelines
Effective 8 a.m., Thursday, Dec. 30, Vidant will update its visitor guidelines across the system, including restricted visitation and a new requirement that all visitors wear a hospital-issued mask. Cloth masks will no longer be permitted. Visitors should also be mindful of Vidant’s new screening process and are encouraged to visit VidantHealth.com/checkin to register prior to their visit.

This is an evolving situation and Vidant continues to monitor the spread and examine local data, including COVID-19 cases in our region and in hospitals, and will adjust visitation restrictions accordingly.
For the latest information on Vidant’s visitor restrictions, please visit VidantHealth.com/VisitingVidant.
Wellness Center – Greenville
Originally scheduled to fully reopen on Jan. 1, the Greenville Wellness Center will open with limited services only starting on Jan. 1, such as personal training, private lessons, fitness orientations and tours. The fitness center, indoor track and pool will remain closed for general membership for the time being. Community members signed up to become members of the Greenville Wellness Center will receive additional details directly from the Wellness Center.
Vidant leadership, with guidance from our infectious disease experts, will continue to review the COVID data and spread throughout the coming weeks to determine a date for a full reopening.
The Wellness Centers in Ahoskie and Washington will continue their current operations.
All Vidant Wellness facilities will follow stringent COVID protocols for the safety of all including required masking for all members, visitors and staff, effective Dec. 29.
For more information, please visit https://www.ecuhealth.org/services/wellness-prevention/vidant-wellness-centers/#covid-19-update
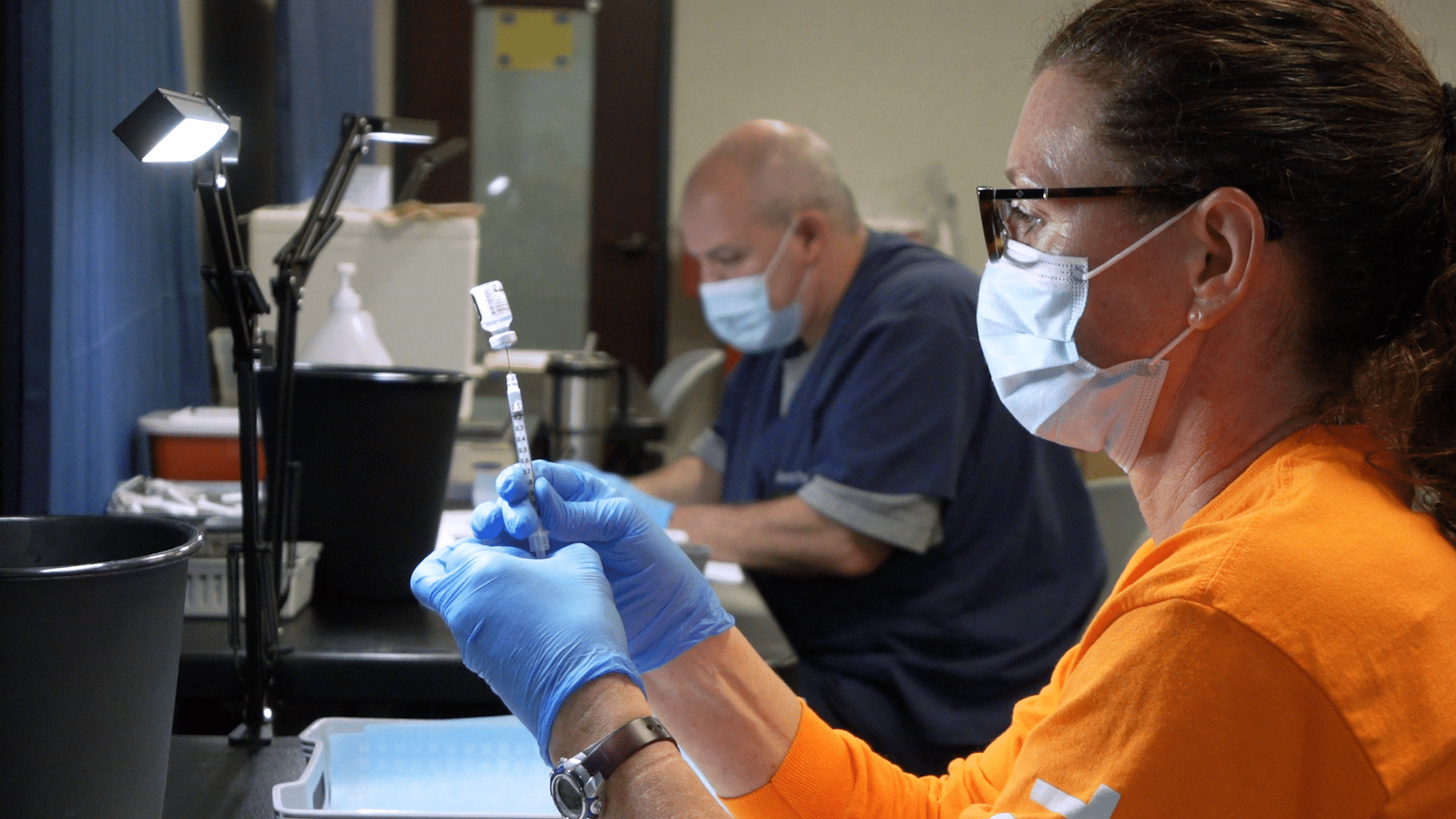
Greenville, N.C. – Nov. 02, 2021 – Eligible community members who received their first two Pfizer-BioNTech (also known as Comirnaty) or Moderna COVID-19 vaccine doses at least 6 months ago, or the single dose of the Johnson & Johnson COVID-19 vaccine at least 2 months ago can now schedule a COVID-19 booster shot appointment through Vidant Health by visiting VidantHealth.com/Vaccinate or calling 252-847-8000.
Vidant is offering booster shots to eligible community members in accordance with the North Carolina Department of Health and Human Services (NCDHHS) guidelines. Appointments can be scheduled at Vidant clinics throughout the region.
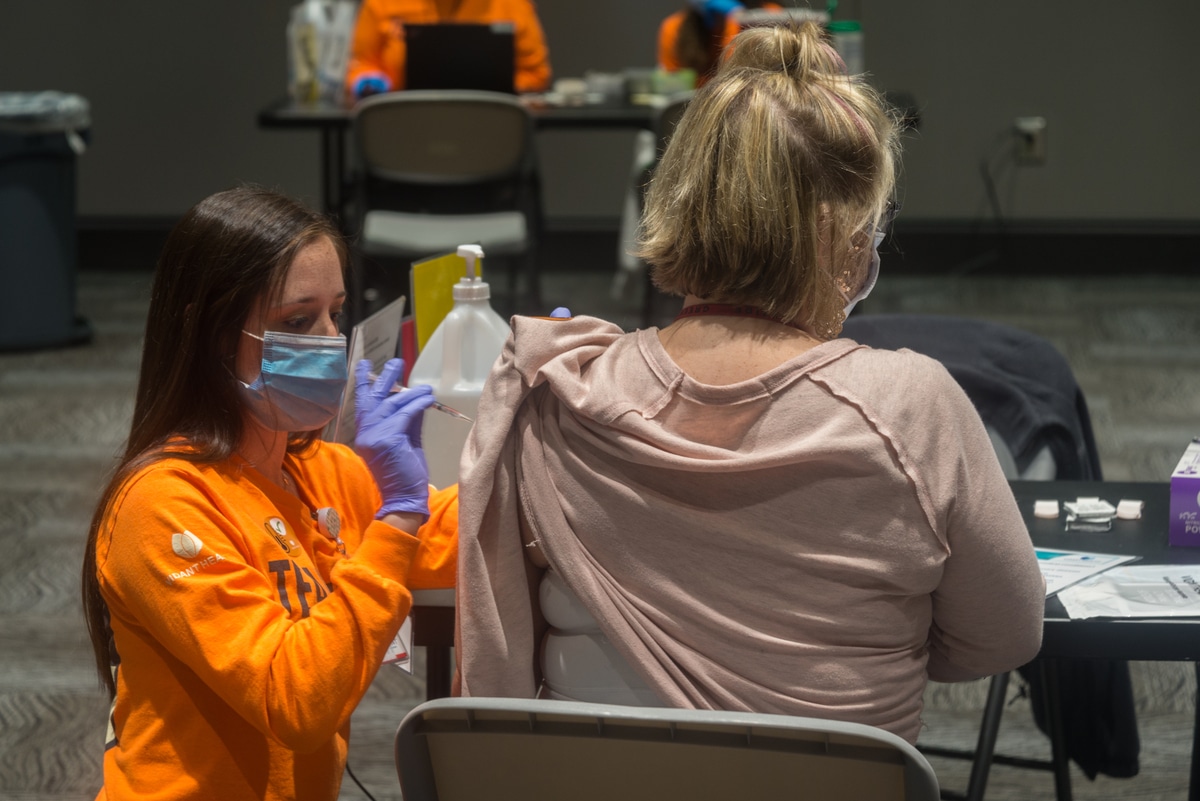
BOOSTER SHOTS FOR PFIZER & MODERNA VACCINE RECIPIENTS
Community members who initially received a Pfizer or Moderna vaccine must wait at least 6 months since their second dose and meet at least one of the below criteria:
- 65 or older
- 18 or older and live in a long-term care facility
- 18 or older, have a medical condition that puts you at high risk for severe COVID-19, and believe the benefit of receiving a booster outweighs the risk of receiving the booster.
- 18 or older, have higher risk of exposure due to work or living situations, and believe the benefit of receiving a booster outweighs the risk of receiving the booster.
BOOSTER SHOTS FOR JOHNSON & JOHNSON VACCINE RECIPIENTS
Community members who initially received a Johnson & Johnson vaccine must be 18 or older and wait at least 2 months from their initial dose.
Studies show that after being vaccinated against COVID-19, protection against the virus may decrease over time and provide less protection against the Delta variant. A booster shot may help increase immune response and improve protection against COVID-19, including the Delta variant.
There are now booster recommendations from the Centers for Disease Control and Prevention (CDC) and approval from the Food and Drug Administration (FDA) for all three available COVID-19 vaccines. Individuals can receive any brand of the COVID-19 vaccine for their booster shot, regardless of which brand they received initially.
THIRD DOSE FOR IMMUNOCOMPROMISED – PFIZER AND MODERNA ONLY
In addition to the new booster shot eligibility, Vidant previously announced it is closely following CDC guidance to provide third doses to eligible immunocompromised community members. A third dose may prevent serious and possibly life-threatening complications of COVID-19 in immunocompromised people who may not have responded to their initial vaccine series.
Appointments can be scheduled at Vidant clinics and oncology practices throughout the region for community members who meet the below criteria:
- You have had an organ or stem cell transplant.
- You are receiving chemotherapy, other treatment for cancer or tumors, taking biologic agents (Humira, Enbrel, Remicade, etc.), taking high doses of prednisone, or taking similar drugs. Many of these drugs are used for treatment of cancer, Crohn’s disease, rheumatoid arthritis, or psoriasis.
- You have a disease that weakens your immune system (like HIV or a primary immune system disease).
- Your doctor told you that you are immunosuppressed.
The third dose is recommended for immunocompromised individuals at least 28 days after their second dose of the Pfizer or Moderna vaccine and is not recommended for those who received Johnson & Johnson’s Janssen COVID-19 vaccine. The Pfizer-BioNTech COVID-19 vaccine is also identified by its new brand name Comirnaty.
Please continue checking back to VidantHealth.com/Vaccinate for the latest information on Vidant’s vaccine efforts.
Greenville, N.C. – Oct. 1, 2021 – Community members who received their first two Pfizer-BioNTech COVID-19 vaccine doses at least 6 months ago and meet the specified criteria below can now schedule a COVID-19 booster shot appointment through Vidant Health by visiting VidantHealth.com/Vaccinate or calling 252-847-8000.
PFIZER BOOSTER SHOT FOR 65+ AND HIGH RISK COMMUNITY MEMBERS
Vidant is offering booster shots to eligible community members in accordance with the North Carolina Department of Health and Human Services (NCDHHS) guidelines. Appointments can be scheduled at Vidant clinics throughout the region if it has been at least 6 months since your second dose of the Pfizer vaccine and you meet at least one of the below criteria:
- You are 65 or older.
- You are 18 or older and live in a long-term care facility.
- You are 18 or older, have a medical condition that puts you at high risk for severe COVID-19, and believe the benefit of receiving a booster outweighs the risk of receiving the booster.
- You are 18 or older, are higher risk of exposure due to work or living situations, and believe the benefit of receiving a booster outweighs the risk of receiving the booster.
The booster shot is authorized by the Food and Drug Administration (FDA) for individuals at least 6 months after their second dose of the Pfizer vaccine and is not currently authorized for those who received the Moderna vaccine or Johnson & Johnson’s Janssen COVID-19 vaccine.
THIRD DOSE FOR IMMUNOCOMPROMISED – PFIZER AND MODERNA ONLY
In addition to the new booster shot eligibility, Vidant previously announced it is closely following Centers for Disease Control and Prevention (CDC) guidance to provide third doses to eligible community members. A third dose may prevent serious and possibly life-threatening complications of COVID-19 in immunocompromised people who may not have responded to their initial vaccine series.
Appointments can be scheduled at Vidant clinics and oncology practices throughout the region for community members who meet the below criteria:
- You’ve had an organ or stem cell transplant.
- You’re receiving chemotherapy, other treatment for cancer or tumors, taking biologic agents (Humira, Enbrel, Remicade, etc.), taking high doses of prednisone, or taking similar drugs. Many of these drugs are used for treatment of cancer, Crohn’s disease, rheumatoid arthritis, or psoriasis.
- You have a disease that weakens your immune system (like HIV or a primary immune system disease).
- Your doctor told you that you’re immunosuppressed.
The third dose is recommended for immunocompromised individuals at least 28 days after their second dose of the Pfizer or Moderna vaccine and is not recommended for those who received Johnson & Johnson’s Janssen COVID-19 vaccine. The Pfizer-BioNTech COVID-19 vaccine is also identified by its new brand name Comirnaty.
Please continue checking back to VidantHealth.com/Vaccinate for the latest information on Vidant’s vaccine efforts.