Insley Santifort was born in November of 2020 with no kidney function; from the beginning of her life, she had to be on dialysis. After an unsuccessful initial kidney transplant at another institution, Insley transferred to ECU Health to receive a second kidney transplant in 2024. With the help of her family, her kidney donors, her surgeons and the entire ECU Health transplant team, Insley is now able to do some things she and her family weren’t sure would ever be possible.
In need of a kidney
After Insley’s traumatic birth, wherein she suffered from hypoxic ischemic encephalopathy (HIE) and catastrophic blood loss to her kidneys, she was moved to Maynard Children’s Hospital to receive the best care possible. That’s where she and her family met Dr. Liliana Gomez Mendez, a pediatric nephrologist. “I met Insley shortly after she was born, which was a traumatic birth,” Dr. Gomez Mendez said. “She was transferred to ECU Health, and we knew her kidneys weren’t working, so she started dialysis the first week of her life. When she came to the NICU, no one knew what would happen.” Insley was able to leave the NICU after 55 days, but her status was still tenuous. Dr. Gomez Mendez decided to refer Insley to the organ transplant team.

That team included Dr. David Leeser, the chief of Kidney and Pancreas Transplantation, and Dr. Margaret Romine, who specializes in transplant surgery and serves as the director of the Living Donor Program. “We worked her up and planned for a living donor,” Dr. Leeser said, “But because of reasons beyond their control, the family had to go to another North Carolina transplant center.” Insley’s family put out a call to their friends and family to secure a kidney for their daughter when Insley’s immediate family members weren’t a match. “I was of course tested but was denied based on some findings,” Kayla Santifort, Insley’s mom, said. “My husband wasn’t a match because of blood type, so at that point we had to turn to our community for help.”
Incredibly, they were able to find a donor, and Insley had her first kidney transplant in July 2023. The transplant, however, was not successful. “Her transplant thrombosed within the first 48 hours of surgery,” Dr. Leeser explained. “There are of course risks for this type of surgery,” Dr. Gomez Mendez added. “And so Insley ended up in critical condition.” Insley pulled through, and the kidney regained some function, but it became clear that she was going to need another kidney, and soon. “That’s when Insley’s family came back to ECU Health,” Dr. Gomez Mendez said. “Before we were even discharged from the other hospital, I reached out to Dr. Gomez Mendez and told her we wanted to transfer back to ECU Health,” Kayla said. “Because Insley was a fresh transplant and the kidney was technically working enough to keep her off dialysis, Dr. Gomez Mendez had to get the okay from Dr. Leeser and his team to accept us back.” Dr. Leeser said they would take Insley’s case, although it was anything but uncomplicated. “Insley’s case was not standard, and I think that her case is a true testament to the potential of our program,” Dr. Romine said.
Kayla and Insley’s family found themselves in the same predicament as before: they needed a new kidney and a new donor. “How do you ask someone to put their life on hold and take a part of themselves to give to your daughter to save her life?” Kayla said. Yet, Insley’s family and the transplant team were amazed when more than 100 people came forward to be tested as potential donors. “That’s the most the transplant team ever had,” Kayla said. “We had people from Wayne County, Duplin County and even out of state get tested. It shows how close our communities are.” There were so many volunteers, it took some time to parse through the list. “It’s a huge process of evaluating potential donors, and we were fortunate to have a good donor from that list,” said Dr. Romine.
A new donor
That donor was Jenny Godwin, a former ECU Health team member who worked in the transplant operating room (OR). She also happened to know Kayla from when they worked together at UNC Health Wayne in the emergency department (ED). “We’ve known each other for years,” Kayla said. “Did I think 10 years ago Jenny would be the one to donate her kidney to save my daughter’s life? No. Now I couldn’t imagine life without her and her family.”
When Jenny learned Insley needed a second kidney, something told her to get tested. Kayla, too, had a similar premonition. “I knew they were looking for a small female donor, and I just had this feeling about Jenny,” Kayla said. “I remember I was sitting in my truck when Jenny FaceTimed me to tell me she was a match. There are days now that I cry to know someone like Jenny with kids and a husband was willing to save my child’s life.” Jenny said her experience in the transplant OR helped her feel at peace about the decision to donate. “When I was on the transplant team, I assisted with living donors and witnessed transplants in the OR. After I found out I was a match, I met with the transplant team to discuss my surgery and it was amazing. It felt right.”
“You’d be surprised at how many people decide to donate a kidney,” Dr. Leeser said of Jenny’s generosity. “It takes folks who are committed to making an impact on the world and the greater good in a way that is utterly selfless and remarkable.” Dr. Leeser noted that although it’s very safe to be a living donor, more than 100,000 people are on a waitlist for a new kidney. “If only .03% of the U.S. population donated a kidney, we would wipe out that waitlist in a year,” he said.

The team scheduled Insley’s surgery for several months out, in the hopes that she would heal from her first transplant while avoiding putting her back on dialysis. Finally, in February 2024, Jenny donated her kidney and Insley underwent her second kidney transplant in less than a year. Dr. Matthew Black, the newest partner on the transplant team, worked with Dr. Leeser to prepare Insley for the implant. “The surgery was complex enough to require two attending level surgeons,” Dr. Leeser said. Dr. Leeser acknowledged that it was a challenging surgery, and not just because Insley was a small child. “There was scar tissue, and of course we had to remove the first kidney to put in the new one,” he said. “In a child that size, you worry about blood loss. Everything in a child is fragile, but everything went exceedingly well.” Dr. Gomez Mendez was also pleased with the surgery outcomes: “The kidney began working immediately, and she had no complications.”
A team like no other
Kayla attributes her daughter’s successful outcomes to the transplant team, Dr. Gomez Mendez, the pediatric intensive care unit (PICU) and Insley’s entire ECU Health team. “They are all just phenomenal,” she said. “They were very up front and honest that this was going to be a difficult and lengthy surgery, but after hearing their plans, I knew we were in the best hands. If anyone could explant and transplant her, it was this team.” Jenny felt the same way: “Not all teams get along and you can feel that. This one makes you feel like it’s a family and they’re on the same page, and that shows. The morning of my surgery I felt at ease and peace.”
Dr. Leeser also had a lot to say about the knowledge, skill and teamwork of the ECU Health transplant team: “Dr. Romine runs the donor side of things, and she’s helped to grow our program over the last six to seven years, so we’ve gone from doing around 80 surgeries a year to between 130 and 160 a year. And Dr. Gomez Mendez came to us from the University of California San Francisco, one of the best hospital systems in the world for transplants. She’s exceedingly intelligent and understands the psyche of surgeons. She is as big of a reason Insley’s family wanted to be at ECU Health as anyone else.”
Together, Dr. Leeser said this team is always focused on taking care of the patients and will work through any issues. “You want physicians who push and test each other. Our team has great discussions. Sometimes we laugh, sometimes things are tense, but at the end of the day, we’re all in it together.” That involves everyone, he said, including administrators, surgical coordinators, social workers, nutritionists, nurses, pharmacists and countless others. “This work takes a tremendous amount of support. In the intensive care unit (ICU) we meet with nurses and managers on a regular basis, and we’ve developed strong relationships with our PICU colleagues. We have learned how to work together to bring the most of what each of us can to the patients.”
Dr. Romine agreed, citing the unique nature of their team. “We’re doing what bigger systems are doing with less resources. That’s only possible with a team that buys into the goal,” she said. These services are especially important, as they provide vital services to a region in need. “One of the things I’m proud of is that there’s such a need medically and a lot of patients who otherwise would have to go to elsewhere don’t have to. I love that our program is allowing access to care that wouldn’t otherwise be there.”
The result of this teamwork is positive patient outcomes, including those for Insley. “She went home after five days in the hospital and she’s done superbly well,” Dr. Leeser said. “When you have renal failure, you don’t feel well and things don’t taste good, so Insley wasn’t eating much before the surgery. Insley is now able to enjoy some foods.” Kayla also sees the change in Insley’s quality of life. “If you look at Insley and know her story, you know how much she and our family have suffered. She couldn’t go swimming or go to the beach, or even take an actual bath when she was on dialysis. We’re going to the beach this weekend to celebrate Jenny and her family.” It’s those little things Kayla said people take for granted but are so special now.
A gift that saves lives
Those little things wouldn’t be possible without generous donors like Jenny, as well as Insley’s first kidney donor, and the National Kidney Registry. “I want to raise awareness about organ donation, and not just after someone passes away,” Kayla said. “Living donation allows you to give a part of yourself while you’re still alive to save someone else. As a nurse and the mom of a transplant patient, the importance of organ donation has never been more real.” Jenny, too, was eager to speak about her experience so others can consider doing what she did. “If anyone is on the fence, I am happy to talk with them. It’s important we have living donors.” Dr. Leeser emphasized that the National Kidney Registry is a great place for potential donors to explore their options. “Someone might want to donate to their family member, so we put the donor in the registry. Even if they don’t match with their intended person, they can still donate their kidney to someone who needs it, and their intended recipient receives a voucher so they receive a kidney from a well-matched donor on the registry.” Dr. Gomez Mendez also wanted people to know that kidneys donated from living donors perform better than those from deceased donors. “The only way for Insley to have the best outcomes was from a live donor,” she said. “A live kidney will last more than a deceased donation.” The National Kidney Registry’s website reports that the average length of time a kidney from a deceased donor lasts is 10-15 years, while it’s closer to 20-40 years when it’s from a living donor.
Because of Jenny’s gift of a kidney, and because of the hard work of Dr. Leeser, Dr. Romine, Dr. Gomez Mendez and the many others on the transplant team, Insley now has a chance at a normal life. “I’m so happy we are at a point where Insley has a fully functioning kidney. It was a long battle, and I’m happy to see her thriving and being a little kid,” said Dr. Gomez Mendez. Kayla attributes Insley’s success to the care she received from ECU Health. “I’d recommend ECU Health and the children’s hospital to anyone,” she said. “To watch her go from an unhealthy quality of life to growing and thriving – that reward is more than anyone could ask for.” Dr. Leeser is quick to share the credit for Insley’s and other patients’ success with the program and team, which they’ve worked to build over the last seven years. “I’m very proud of the program,” he said. “I would argue we’re the best program for kidney transplant in the state, and we’re on the precipice of doing even more.”
If you are interested in learning more about how to donate a kidney, you may visit https://www.kidneyregistry.org/, or if you’d like to learn more about ECU Health’s transplant services, visit here.
On April 3, hospitals across the HonorBridge service area participated in a Pause to Give Life event to recognize the importance of organ donation.
A Donate Life flag was flown outside of ECU Health Medical Center to honor donors, their families, those who are waiting, and recipients who received the gift of life. Typically an outdoor ceremony, this year’s event was hosted in the Interfaith Chapel at ECU Health Medical Center due to inclement weather.
A moment of silence was held at 10:08 a.m. to signify that one donor can save eight lives.
Last year, ECU Health Medical Center had 31 organ donors and 75 organs were transplanted while 17 were sent out for research. The Medical Center had 49 tissue donors with 140 tissues recovered. Additionally, there were 80 eye donors with 98 corneas transplanted, 28 placed for research and 16 whole globes were recovered. This marked a record number of transplants performed at ECU Health Medical Center, including 130 kidney and kidney-pancreas transplants and 5 pediatric transplants.

During the event, Jenny Godwin, a former nurse at ECU Health Medical Center, spoke about the importance of organ donation. In February, Godwin donated a kidney to the 3-year-old daughter of a co-worker and said she felt called to step up for a friend.
“We knew I was going to be a match when I went in for testing. It was this feeling that me and my husband had and we felt very passionate about doing this,” Godwin said. “It’s the first time I’ve been able to experience peace throughout the whole experience so it was amazing.”
In her time at ECU Health, Godwin worked on transplant teams and she said it was a full-circle moment to be on the other side as a patient.
She said the opportunity to be an organ donor has given her a sense of accomplishment and fulfillment.
“People always say it’s better to give than receive and I can tell you it’s been an awesome feeling to know that I have given her life,” Godwin said. “I mean, she’s 3 years old and has her whole life ahead of her. It’s really awesome to know that I was able to be a part of that.”
Godwin said she was tired for the first couple weeks after surgery but a little more than a month removed, she’s feeling great and back to her old self – including running around with children of her own.
Dr. David Leeser, chief of transplantation at ECU Health Medical Center, also spoke during the event and said it’s important to recognize those who have said “Yes” to organ donation, whether it is as a living donor or a donation after a person has passed. He also said with 100,000 patients across the country and 3,000 patients here in North Carolina waiting for a donation, it’s crucial to raise awareness of the need for organ donation.
He said transplantation takes a village and none of what he does as a transplant surgeon is possible without the many teams working to make each surgery possible.

“The transplant team is huge – you have organ procurement organizations like HonorBridge, they spend 24 hours a day, seven days a week ready to come to hospitals, meet with families and get donors,” Dr. Leeser said. “Once they have the donor, they arrange having surgeons available to take out the organs for transplant and figure out who the organ is going to and all the pieces that go into getting the organ to the recipient hospital before the transplant even occurs. Each transplant program has social workers, dietitians, nurses and physicians – everyone is so crucial to make sure a transplant is successful. We stand on the shoulders of so many dedicated professionals that do the hard work of getting our patients ready to go to the operating room.”
At ECU Health, we are grateful for the over five million North Carolinians who have registered as organ, eye and tissue donors. We also appreciate the efforts of our North Carolina Department of Motor Vehicles partners, who ask the questions every day as part of their job. Together, we are united in a mission to save and heal lives and create a culture where donation becomes a fundamental human responsibility.
Those interested in learning about organ donations or interested in becoming an organ donor can visit ECU Health’s donor registration portal or the Donate Life website for more.
Read more
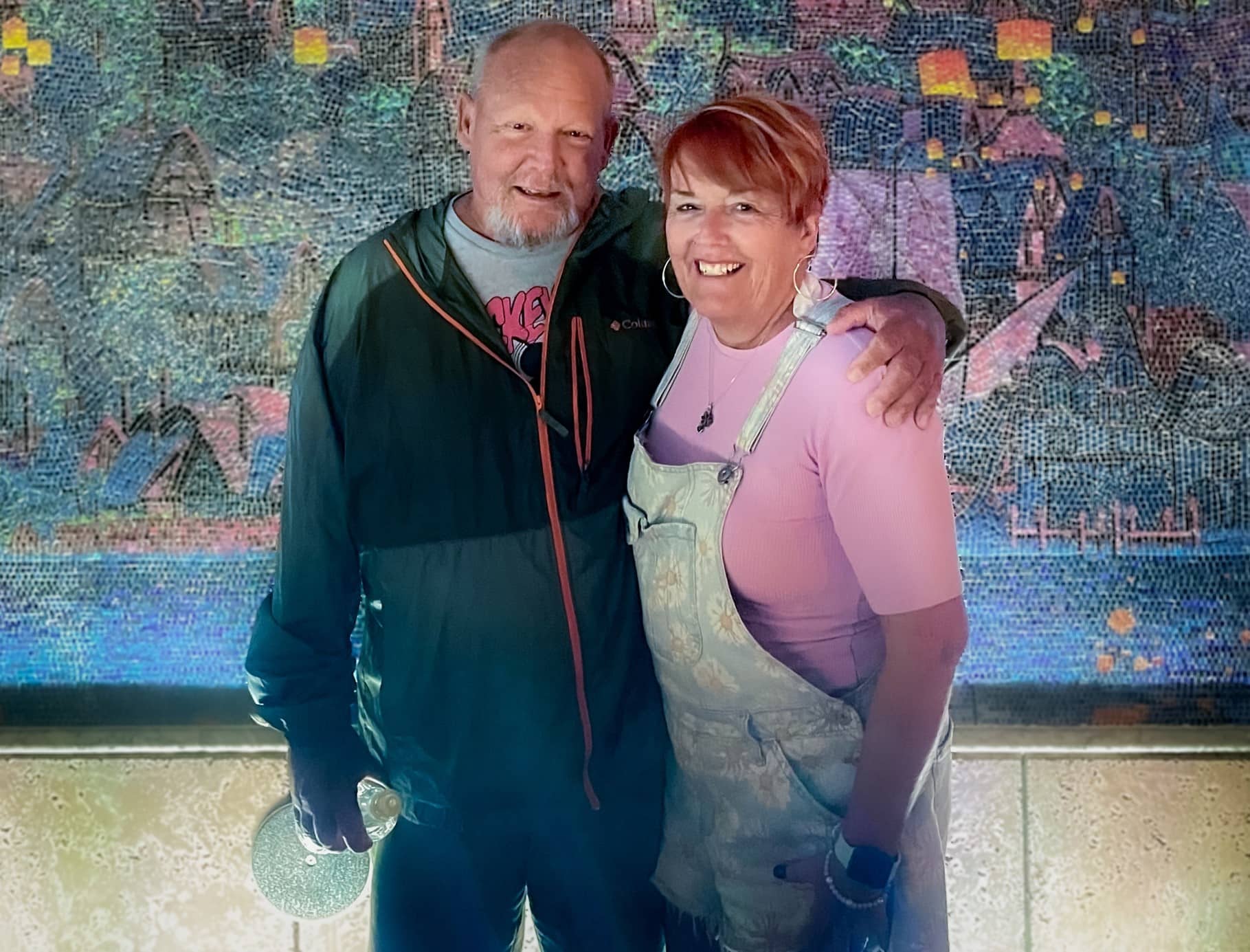
Sharon and Steve McNally of New Bern have been married for more than 40 years. Now, Steve carries a little piece of his wife Sharon with him everywhere he goes.
Steve is diabetic and in 2015, he went through his first round of transplants at a hospital in their then-home state of Pennsylvania.
“It was supposed to have been a kidney and pancreas at the same time,” Steve said. “When they got me on the operating table, the pancreas wasn’t viable. So they said, ‘We’re going to do the kidney alone and we’ll get you a pancreas.’ What happened then was the hospital eventually became decertified and couldn’t do pancreas transplants anymore.”
Then, they joined the transplant list with a health system in Maryland and Steve received a pancreas transplant 30 days later. In the meantime, the new kidney had been damaged due to the lack of a functioning pancreas, but Steve said it was largely working fine until mid-2023. By that time, the McNallys had moved from Pennsylvania down to New Bern.
With Steve’s kidney function worsening, there was little time to spare. He could join another transplant list that may take eight to 10 years to find a donor, start dialysis or personally find a match to donate a kidney.
Sharon said she knew she had to step up for her husband and get tested to see if she could be a match.
“It wasn’t really hard for me because a lot of people say, ‘Oh my gosh, you’re so amazing’ or so this and that but I don’t really feel that way,” Sharon said. “I feel like we’ve been married 40 plus years. We have grandkids and kids together and how could you watch someone get more and more ill and not do something if you can? So I didn’t really think about it.”
Testing started for the two in June and preparation began right away. They found out in October they were a match and an ECU Health team performed the transplant on Nov. 7.
“I’m glad that this was something I could do,” Sharon said. “There’s a lot of people that probably couldn’t have, even if they wanted to.”
For Sharon’s part, she went home the next day while Steve stayed a couple extra days for monitoring before heading home. While they each needed some help early on after coming home, they were both happy to support each other, as they’ve been doing for more than four decades.
Dr. Margaret Romine, transplant surgeon at ECU Health, and Dr. David Leeser performed the transplant along with other members of the ECU Health transplant team. She said she was most proud that the team could take on a case like the McNallys, especially given Steve had been through a kidney and pancreas transplant previously.
“They had already been through a lot before even coming to us but they had such great attitudes and were great patients to care for,” Dr. Romine said. “We have such a great team and that really sets us apart from other programs. It’s not just about what the surgeon thinks – the nephrologists play a huge role. Our coordinators, nurses, pharmacists, social workers all play a huge role. We can’t do what we do without the entire team. Whenever we make a big decision to take on a patient like him, it’s done as a team.”
Steve and Sharon both said they were happy with their experience at ECU Health and shared appreciation for the care team that helped guide them through the process and into recovery.
Now, they are looking forward to a spring working outdoors, something they both love but missed out on last year.
Sharon said if she could share one message, it would be on the importance of organ donation.
“Organ donation is just such a wonderful thing. I mean, three different times it saved my husband,” Sharon said. “You know, a lot of people don’t want to do something like that even after they’re gone because it just it seems weird to them. But honestly, I think it’s a wonderful thing.”
On Wednesday, ECU Health Medical Center partnered with Honorbridge to celebrate National Donate Life Month and recognize organ and tissue donors, their families, those who are waiting for life-saving and life-changing donations, and recipients of organ and tissue donations.
The occasion was marked at 10:08 a.m. as the Donate Life flag was raised in front of ECU Health Medical Center, followed by a 30-second moment of silence. These two numbers are significant as the time symbolizes that one donor can save eight lives while the moment of silence recognizes the 3,000 North Carolinians waiting for an organ donation.
Dr. Walter Pofahl, chief medical officer for ECU Health Medical Center, said eastern North Carolina is home to a disproportionately high number of those 3,000 in North Carolina. Dr. Pofahl shared that last year ECU Health Medical Center had 31 organ donors, transplanted 90 organs while 18 were sent out for research. It also had 56 tissue donors with 141 tissues recovered and 90 eye donors with 84 corneas transplanted and 21 placed for research.
A daughter’s gift

During Wednesday’s event, Darice Fonville shared her inspiring story of donating her kidney to her mother in February.
Fonville said her mother had suffered from chronic kidney disease for about 20 years and as she began to struggle more, they learned she would need to find a donor or start dialysis. She knew that dialysis can be very difficult for patients, and she wanted to help her mother any way she could. So Darice decided to get tested to see if she would be a match.
“I was actually at work when I got the call, and they let me know we were a match,” Fonville said. “As soon as I got that call, everybody in the office already knew how excited I was. I put work on pause to go call my mom. She already knew, and she was nervous. I was excited. I knew it was a done deal. We were just going to go through with it.”

She said she never had any hesitation when she knew she could give something back to her mother and improve her life. She said the transplant team at ECU Health Medical Center put everyone at ease and allowed Fonville and her mother to be together shortly before surgery to spend time with one another.
How to give
Dr. Pofahl said while it is important to identify as an organ donor when you receive your driver’s license or state identification card, it’s just as important to share your wishes with those close to you.
“It’s not always easy, but having that discussion is important,” Dr. Pofahl said. “In that critical time when decisions are being made around donation, if your loved ones understand what your wishes are upfront and ahead of time, that makes the process a lot easier.”
While only about 50 percent of adults in North Carolina are registered organ donors, there are 3,000 people waiting for organ and tissue donations in North Carolina and more than 100,000 waiting for a donation across the country.
Learn more about how to become an organ donor and the impact you can make as a donor on Donate Life’s website.
Resources
With our continued focus on the imperatives of quality, experience and finance, ECU Health’s transplant program at ECU Health Medical Center has consolidated their treatment and office spaces into the newly renovated 3 South. The area is now known as the 3 South Transplant Clinic.
The transplant program performs an average of 80 to 100 living and deceased donor kidney and pancreas transplants per year. Patients that are seen in the clinic include pre-transplant (patients being evaluated for transplant), living donors and post-transplant. This program and the services offered have continued to grow over time, but have been limited by clinic space. To enhance patient and team member experience, the pre- and post-transplant clinics have now consolidated into one, centrally-designed space on 3 South, as they have been operating in separate clinics at the Cancer Center and ECU Physicians.
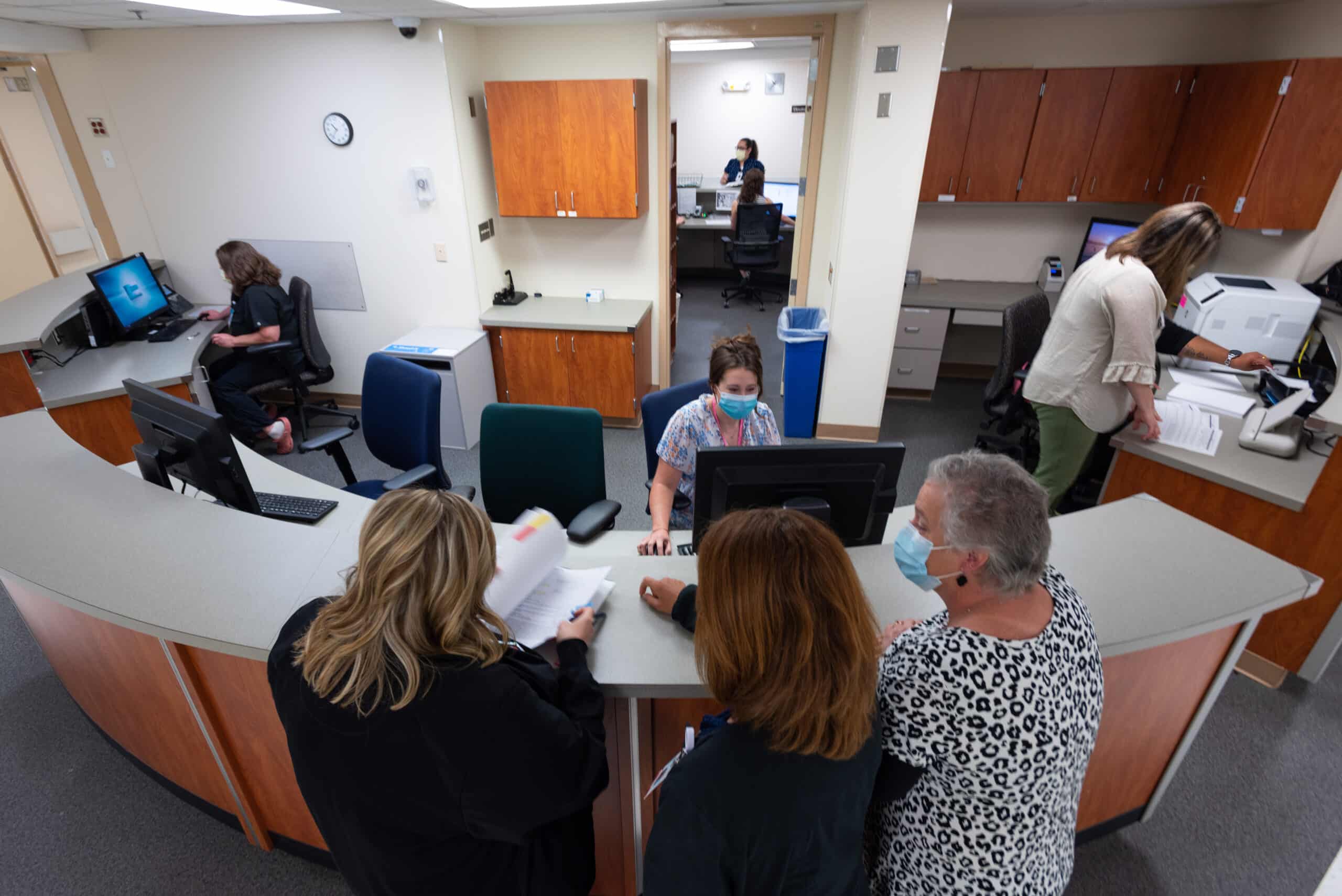
Previously, the transplant team worked in separate clinics, sometimes limited to three rooms. 3 South Transplant offers 18 patient exam rooms, which in addition to consolidating space for patients, will also help to shorten wait times for new referrals and follow up appointments.
Another benefit of 3 South is the accessibility of team members such as dieticians, social workers, pharmacists, nurses and physicians, which provides patients the accessible support of various teams of health care workers critical to patients’ transplant journeys.
Lastly, this consolidation allows for expansion of potential future services such as phlebotomy, expanded pharmacy services, infusion services and vascular access.
In 2022, as we build the future of ECU Health, the exceptional care and services we provide have a positive impact on the communities of eastern North Carolina that we serve through our considerations of patient quality and experience.
For more information on transplant services at ECU Health, visit the transplant section of our website.