Success stories start as dreams we harbor in our youth. Career days such as the third Future Health Professionals Conference Nov. 23 help fill in the critical details that make it believable.
Nearly 100 students from 11 counties in central and eastern North Carolina made the trip to Greenville and the Health Sciences Campus of East Carolina University for the event hosted by ECU Health and the university.
D.H. Conley senior Chance Frederick of Greenville was one such student, but one of only a handful who had taken part in the very same event last year.
“I was really amazed the first time by everything they offered me, especially the hands-on experience in the dental clinic. It really made me want to come back,” he said. “And just being able to network and meet people, to see these faces that I just know will be really beneficial for my future, I can’t get that anywhere else.”
Investing in the Future of Health Care
Students listened to medical professionals speak about their career arcs, then walked to nearby schools of medicine, dental medicine and nursing to tour facilities and experience hands-on curriculum at training stations and simulations.
“Engaging high school students early is crucial to addressing the national health care shortage, especially in rural areas like eastern North Carolina,” said Koai Martin, an equity and special projects consultant for ECU Health.
Both the health system and the medical school have a demonstrated history and mission of training and employing health care professionals to work in underserved areas of the state. Efforts such as the Future Health Professionals Conference help “create a pipeline of providers and health care professionals who understand the unique challenges of rural health care,” she said.
“Ultimately, it’s about investing in the future of health care while uplifting the region our ECU Health and ECU medical school proudly serve,” Martin said.
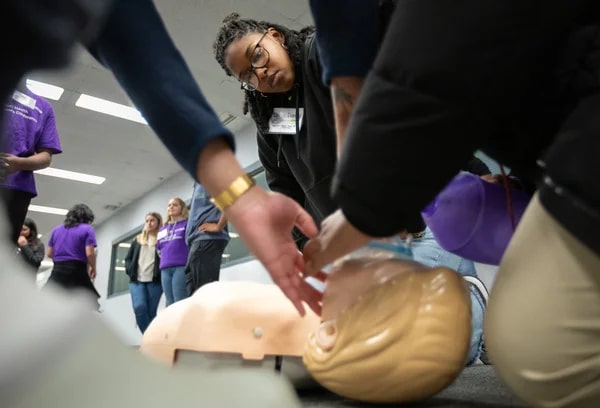
Several students from the Brody School of Medicine led hands-on life support demonstrations and Stop the Bleed simulations. Dr. Calvin Blocker, a resident physician at the school and ECU Health, discussed the epidemiology and pathophysiology of strokes and methods for detecting and identifying stroke symptoms that concluded with an interactive experience involving the examination of brain models and specimens to show areas commonly affected.
“The Future Health Professionals Conference gives high school students insight into the daily lives of our students and the responsibilities of practicing professionals,” said Milton Bond, who directs the medical school’s Pathways to Health Careers Program. “It is important for ECU to commit resources to support initiatives like this to invest in building the future health care workforce.”
In the Middle of the Journey
“I knew I wanted to be a dentist from about 10 years old, but I didn’t get to do anything like this, and no one in my family was in the medical or dental field,” said Dr. Scarlett Walston, a clinical assistant professor in the School of Dental Medicine. “I think it’s really cool just for them to be able just to explore. Maybe one of them falls in love with dentistry, and maybe we’ll see them in the application cycle in a few years.”

Walston said preparing for the DAT — the Dental Admissions Test — is something some committed students begin even in high school. Outreach such as the conference can give young students a shot of hope at a time when they might feel bewildered and disadvantaged navigating such a competitive track.
“Helping the next generation find their path is always important,” she said.
Jennifer Kovacs is a career nurse and health sciences high school teacher who brought eight students to the conference from Dare County. She says health care is a wide-ranging industry that employs trades and hourly workers alongside highly trained specialists.
“There are so many opportunities. If blood and sickness are too much, there’s a cubicle you can sit in and be by yourself and still contribute to health care,” Kovacs said. “There’s a microscope; be a researcher developing a new drug or running lab tests. You can sterilize surgical equipment — another surgery cannot begin until you’ve sterilized from the last one.”
Her students, she says, are weighing careers on several factors. Passion is one, but years spent in college and student debt factor into plans.
“Health care is not just doctors and nurses. It is other clinicians. It is secretaries. It is custodial, meal services, environmental services. And it is a family. … and therefore you can get students involved in any of those aspects,” she said.
Frederick, the 17-year-old senior, put his statistical chance of eventually becoming a dentist at the dizzying tip of the range, 99%.
“I’ve wanted to be a dentist ever since I was 3 years old,” he said. “That was the age of my first dental appointment. If I’ve been into it for 14 years at this point, I think I can take the next 14 to make it happen.”
And he expects to make this dream a reality right in his hometown, at East Carolina University.
“Today, I got to meet with a bunch of second- and third-year dental students. I got to walk right into the lab and immerse myself, and they made me feel included,” he said. “So even though I haven’t started, I saw what it was like to be in the middle of the journey, and it makes me feel like, you know what, I can really do this.”
Greenville, N.C. – ECU Health and the national nonprofit Undue Medical Debt are pleased to announce an initiative that will help eliminate more than $186 million worth of past-due hospital medical debt for more than 32,000 qualifying patients. Debt relief letters will arrive over the course of December’s holiday season into the New Year on a rolling basis given the size of this relief effort
Eligible community members do not need to apply, and there is no application process. Instead, community members who qualify for this one-time debt relief will receive a branded letter from Undue Medical Debt indicating which past-due hospital debt or debts have been eliminated. Undue Medical Debt works with hospital systems and other providers across the country to purchase past due medical debt belonging to those least able to pay in large portfolios for pennies or less on the dollar and then erases the debt.

ECU Health’s collaboration with Undue Medical Debt pre-dates North Carolina Department of Health and Human Services’ medical debt relief initiative which spans all hospitals in the state and lays out a plan for medical debt relief coupled with changes to Medicaid/Medicare reimbursement policy and financial aid standards in 2025.
Under Undue Medical Debt guidelines, those who qualify for this medical debt relief have hospital medical debts that are 5% or more than their annual income or earn at or below four times poverty-level income. The current federal poverty level is an annual income of under $31,200 for a family of four which means a qualifying family of four would make under $124,800. Community members do not need to take any action, as the eligible hospital medical debt will automatically be eliminated for those who qualify.
“We’re grateful to collaborate with ECU Health to help ease the burden of medical debt in eastern North Carolina,” said Undue Medical Debt CEO and President Allison Sesso. “Helping community members burdened by medical debt takes thoughtful collaboration and I’m proud of the results: over 30,000 people helped this holiday season. We hope this program provides financial and emotional relief to recipients and encourages them to continue engaging with the healthcare system.”
The collaboration with Undue Medical Debt is one of many ways in which ECU Health is living its mission to improve the health and well-being of eastern North Carolina. The initiative aligns with the health system’s commitment to serving underserved communities in the East, many of which have disproportionate numbers of low-income and uninsured or underinsured people. The initiative is also in alignment with ECU Health’s long-standing practice of non-predatory billing practices, which emphasize charity care, zero-interest payment plans, transparent pricing and dedicated resources to help patients navigate financial requirements.
“At ECU Health, our commitment to our mission and patients is at the heart of all we do,” said ECU Health Chief Operating Officer Brian Floyd. “We have always been guided by a deep desire to support our patients in whatever way we can, and this collaboration with Undue Medical Debt will make an enormous impact on so many in our largely underserved region. We could not be more thankful to find an organization like Undue Medical Debt which shares our vision for making high-quality rural health care accessible here in eastern North Carolina.”
In recognition of the one-year anniversary of Medicaid expansion in North Carolina, Gov. Roy Cooper visited ECU Health Medical Center in Greenville to reflect on the impact of expansion and celebrate a year of reaching North Carolinians in need.
Since Medicaid expansion officially launched in North Carolina on Dec. 1, 2023, more than 80,000 eastern North Carolinians and nearly 600,000 people statewide have benefited from access to vital health insurance. Along with Medicaid expansion, the state also passed the Healthcare Access and Stabilization Program (HASP), which provides critical relief to rural hospitals.
Gov. Cooper said Medicaid expansion’s reach in rural communities, like ECU Health’s 29-county service area, has been especially impactful in the last year.
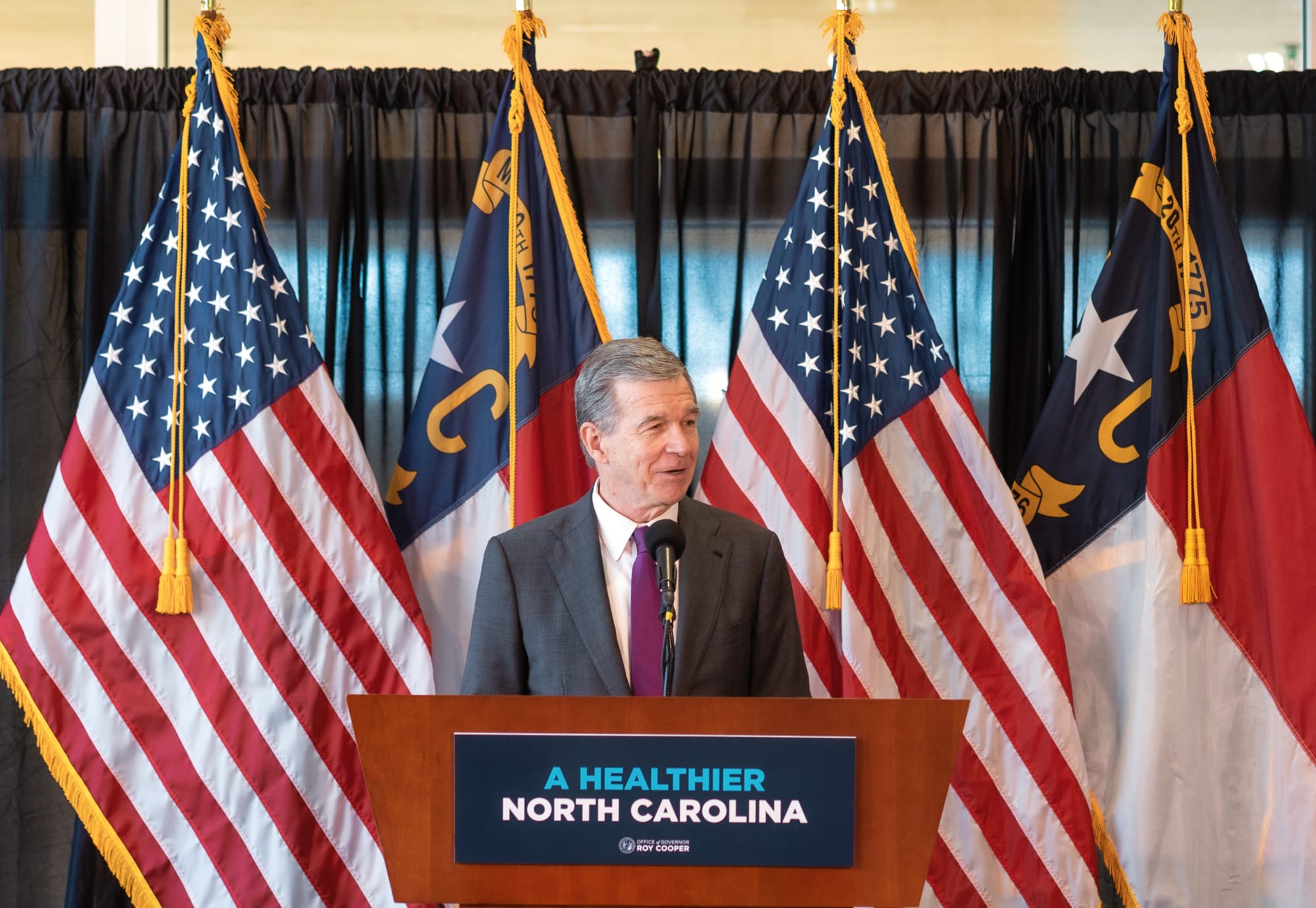
“The last year showed us that this is something that people desperately needed, particularly here in rural North Carolina,” Gov. Cooper said. “I grew up in Nashville and we know that rural North Carolinians have been helped more by Medicaid expansion than anyone else. I hold close to my heart the mission of getting people healthier. I knew getting Medicaid expansion passed and signed into law was the most important thing we could do to accomplish that.”

This milestone reflects the culmination of more than six years of advocacy by ECU Health, driven by the challenges faced by uninsured and underinsured patients.
Dr. Michael Waldrum, ECU Health chief executive officer and dean of the Brody School of Medicine at East Carolina University, said Medicaid expansion and HASP funding is creating real differences for patients, health care workers and the future of health care in places like eastern North Carolina.
“Medicaid expansion has helped improve access to primary care, empowering people to take control of their health and their lives,” Dr. Waldrum said. “It is also an investment in rural health organizations like ours. At the same time and in partnership with the state, ECU Health and the Brody School of Medicine are also committed to doing their part to support primary care expansion efforts in rural health care.”
He highlighted the expansion of the Rural Family Medicine Residency program, which will train nine rural residents per class across three training sites in the East and the upcoming Center for Medical Education Building on Brody’s campus. This investment has helped and will continue to help ECU Health and Brody serve the combined mission of improving the health and well-being of eastern North Carolina.
Dr. Karen Coward, a family medicine physician with ECU Health, is a Kinston native and practices in Tarboro. She said she knew by age 10 she wanted to be a family physician in her home community. She attended Brody and stayed true to her dream of serving eastern North Carolina.
She said before Medicaid expansion, many of her patients would rely on the emergency department for care. Even if a patient was connected with primary care, it was difficult for them to follow through with appointments or afford medications. Chronic conditions like diabetes, hypertension or even cancer would go unchecked. Now, she said, she’s seen a life-changing shift.
“Patients who once cycled through the emergency department are now establishing relationships with primary care providers like me,” Dr. Coward said. “They are keeping their appointments, following through on recommendations, treatments, and gaining access to medications and specialist referrals that were previously out of reach. For many, this will mean earlier diagnoses and interventions, reducing the burden of advanced diseases.”
Kody Kinsley, secretary of the North Carolina Department of Health and Human Services, joined the event and said that in the past year over $58 million in dental claims alone were filed, millions of prescriptions were filled and hundreds of millions of dollars in claims supporting hospital care were taken care of through Medicaid expansion.
He said this comprehensive health insurance is already making a real difference for individuals and families.
“Medicaid expansion is life changing for families,” Sec. Kinsley said. “It is peace of mind for people as they sit up late at night thinking about how the next day will impact them. Will a sickness impact their family? Will they end up in debt? They don’t have to worry about that anymore.”

The event also included remarks from a Medicaid expansion beneficiary, Darcy Guill from Ayden, who shared her gratefulness for regular care she’s receiving, specialists she’s able to visit and prescriptions she can fill, thanks to Medicaid expansion.
As we look back over the previous year, we’re proud to build the national model for rural health care here in eastern North Carolina at ECU Health and we’re grateful for the support the region and health system through Medicaid expansion and HASP.
Seven key priorities served as the central discussion point as community-based health partners joined ECU Health and Pitt County Department of Social Services (DSS) in October for the second session of a conference series designed to support the emergency department and improve access to non-emergent care across eastern North Carolina.
The seven key priorities, identified during the first conference session in early October, represent the unique viewpoints from stakeholders across the community and all of whom share a common goal: reduce unnecessary utilization of the emergency department in Greenville.
The seven priorities include:
- Placement/disposition – getting patients placed in the appropriate care settings outside the emergency department such as skilled nursing facilities, in-home care, adult care homes, foster homes, etc.

- Navigating the system – defining roles and responsibilities of each agency
- Collaboration – improve collaboration among systems and across agencies
- Crisis system – more clearly defining how the system operates and clarifying any confusion that may exist
- Community options and wraparound support – ensure a robust support system in the health care setting and in the community to ensure people get the help they need
- Access to services – provide clarity on where patients need to go to access care
- Regulatory – reduce barriers and create efficiencies in key operational areas like timely discharge and clinical assessments
“This was a moment for us as a health care community to not only clearly define the challenges facing the patients we serve, but to also explore how we can implement solutions that improve the emergency care realities here in eastern North Carolina,” said Jacob Parrish, vice president of capacity and throughput at ECU Health, who served as one of the conference organizers. “The challenges facing emergency departments both locally and nationally cannot be solved solely by the hospitals themselves. These conversations help us take our words and put them into collaborative action.”
Health care and community partners in attendance at the conference included ECU Health, DSS Directors from across eastern North Carolina, Juvenile Justice, Trillium Health Services, Public School leaders, NC DHHS, payors, faith leaders, and other eastern North Carolina hospitals and key stakeholders. The conversation focused on both adult and pediatric/adolescent patient populations who present at the emergency department but could be better served in a different setting.
The importance of education and outreach served as a common theme throughout the discussion. Organizations talked not only about the importance of providing critical information directly to patients, but also emphasized the importance of educating themselves on the role that other organizations and agencies play in the care continuum.

ECU Health highlighted the growing demand for emergency department services and the urgent need to streamline care in the community for non-emergent cases. The discussions underscored how patients with non-critical issues are often funneled to emergency departments due to limited access to routine and primary care resources and crisis services, creating unnecessary strain on EDs. ECU Health Medical Center, for example, remaining full nearly half the year due to high patient volumes, which often exceed its 974-bed capacity. This backlog directly impacts how long some patients may wait in the ED.
“Our commitment to improving emergency care access and efficiency for our patients is unwavering,” said Dr. Leigh Patterson, chief of services for emergency medicine at ECU Health Medical Center. “The collaboration we’re seeing across health care and alongside our community partners demonstrates a shared dedication to creating lasting solutions that serve the unique needs of eastern North Carolina.
By addressing the root causes that lead to emergency department overutilization, we’re working to not only improve the experience for our patients but also strengthening health care in our region.”
ECU Health and Pitt County DSS will host a third session of the conference to further discuss action items and strategies to support more collaboration in the community.
Greenville, N.C. – ECU Health has earned 2024 College of Healthcare Information Management Executives (CHIME) Digital Health Most Wired recognition as a certified acute and ambulatory Level 8. The Digital Health Most Wired program conducts an annual survey designed to identify and recognize health care organizations that exemplify best practices through their adoption, implementation and use of information technology and included more than 48,000 represented facilities in 2024.
“I am incredibly proud of our team’s dedication and innovation, which have been instrumental in achieving the 2024 Most Wired Award,” said Donette Herring, chief information officer, ECU Health. “Our efforts to improve the well-being and efficiency of our clinical team members and adoption of artificial intelligence were top priorities this past year. These achievements underscore the team’s commitment to innovation, education and the seamless integration of technologies across the organization. We look forward to building on these successes and exploring new opportunities to advance ECU Health’s strategies and improve operational performance.”

ECU Health ranked above peers in categories across eight key areas including: infrastructure, security, administrative/supply chain, analytics/data management, interoperability/population health, patient engagement, innovation and clinical quality/safety. Participants receive a comprehensive benchmarking report enabling them to evaluate their current information systems’ health. This report assists in devising strategies to elevate the quality of health care organizations to enhance industry-wide care standards. The assessment covers digital health performance. The survey assesses the adoption, integration and impact of technologies at all stages of development, from early development to industry leading.
ECU Health has piloted several initiatives to enhance patient care and streamline operations. The clinical communication program has enhanced the timeliness of communication and care coordination among team members, as well as increased workforce mobility, evidenced by high utilization in medication administration, documentation, and secure messaging. The MyChart Bedside program allows patients to access real-time education, lab results and pertinent care information directly from iPads, enhancing patient understanding and engagement. In the Emergency Department, the ‘Hello World’ initiative improves patient engagement through enhanced texting capabilities, keeping patients informed on next steps.
Additionally, regional facilities have expanded the tele-sitter program, optimizing resource allocation for patients who need monitoring but not constant one-on-one attention. The implementation of flowsheet macros has been a major efficiency booster, saving nurses millions of clicks and positioning ECU Health as a leader in this innovative adoption. ECU Health is also advancing artificial intelligence (AI) integration across its operations. The launch of the AI Center of Practice (AICoP) has gathered over 200 members across departments to foster collaboration and AI best practices.
“We are proud to recognize your ECU Health’s exceptional dedication to digital health excellence,” said CHIME President and CEO, Russ Branzell. “ECU Health’s pioneering performance in the industry not only inspires other organizations by example, but also provides patients around the world with better care.”
D’Nise Williams is the program coordinator for the Eastern Carolina Injury Prevention Program’s (ECIPP) Teen Safe Driving Program. This year marks the 12th year in a row her team has received grant funding from the Governor’s Highway Safety Program (GHSP). The ECIPP is a community collaboration between ECU Health, Maynard Children’s Hospital, the ECU Health Trauma Center and the Brody School of Medicine at East Carolina University. Its goal is to improve the health of eastern North Carolina residents by reducing the incidence and impact of injuries, and it accomplishes this goal through programs like the Teen Safe Driving Program.
The Governor’s Highway Safety Program is the State Highway Safety Office for North Carolina, and it is dedicated to reducing the number of traffic injuries and fatalities in the state. It promotes highway safety through a number of grants and safe driving initiatives like Click It or Ticket and Speed a Little, Lose a Lot. Many of the grants address behavioral approaches to traffic safety, and the grant the ECIPP received focuses on vulnerable road users—in this case, teenage drivers.

The program’s grant runs for a one-year cycle, and each year, educational efforts focus on two counties, which are selected through examination of county crash rate data. “We look at which counties would benefit from interventions to reduce crash rates, even by a small percentage,” Williams said. With the help of the GHSP grant funding, the Teen Safe Driving Program has been able to expand its services from Pitt County to Beaufort, Lenoir, Martin, Craven, Wayne, Nash, Greene, Duplin and Halifax counties, with hopes to further expand into Onslow County this year. “GHSP has been funding this project for more than a decade,” said Jennifer Delcourt, the vulnerable road users coordinator with the Governor’s Highway Safety Program. “This speaks to the impact of the project and the success of staff in reaching teens and parents with important traffic safety information in eastern North Carolina.”
According to data collected between 2016 and 2021, speeding, lane departure and distracted driving were the top factors in car crashes. To combat this, the program focuses on “5 to Drive rules for new drivers,” as developed by the National Highway Traffic Safety Administration (NHTSA), which include no drinking and driving, buckling up, no use of phones while driving, no speeding and no more than one passenger at a time.
The Teen Safe Driving Program partners with high schools, as well as driver’s education programs, within the identified counties, to promote these safe driving practices for teenagers. “We do lunchtime education tables, partner with health science or P.E. classes, provide parent education curriculum and partner to bring the Cinema Drive interactive 3D movie experience to schools, which is an interactive driving experience that follows someone who has been drinking and driving. We have goggles and an interactive steering wheel, and you can pick out distractions as you drive with and without the goggles,” Williams explained. “The goal is to raise awareness that as a driver, you’re wielding tons of metal on the road, and you need to be your best self mentally.”
The program also provides targeted campaigns for teen drivers, including social media ads, billboards movie theater ads, mall campaigns and gas station TV ads. None of this would be possible without the funding from GHSP.
In 2023, the program achieved just over two million views in their mall campaign, 617 students in driver’s education classes, 7,168 students in lunchtime table education and 6,822 impressions via social media messages. These efforts have yielded positive results for the program. Teens are given pre- and post-intervention surveys to gauge their responses to the education, and there are also pre- and post-driver observations at the conclusion of driver’s education classes. “We usually see a change in behaviors, although it varies by county,” Williams said. “Last year we marked a 6% decrease in distracted driving in Pitt and Duplin counties, but the year before we recorded a 15-20% decrease in our counties of focus.”
Williams said that while it can be challenging to initially establish relationships with schools, once the partnership is established, the Teen Safe Driving Program is invited back year after year. Her goal is to continue to offer school interventions that result in safer driving behaviors, but she also has new ideas. “I want to work on targeted interventions for neurodivergent teens, like teenagers with ADHD or autism. We have so many teens who have trouble focusing already, and a teenager’s frontal lobe, which is responsible for making good decisions, isn’t fully developed,” Williams said. She also wants to establish a partnership with teenagers to create an advisory board for the program. “I’d like to think I’m ‘hip,’” Williams laughed. “But I would love to consult with other teenagers to get their input on what messaging reaches their age group.” Sue Anne Pilgreen, the executive director for the Safe Communities Coalition, the manager of the Pediatric Asthma Program and the manager of the ECIPP, echoed this sentiment. “Teens today aren’t the same as they were 12 years ago, and as they have changed, so has our program. We continue to focus on the historical distractions such as underage drinking and texting while driving, but we now know that mental well-being and substances such as marijuana can also impact teen driving.” Williams said consulting teens about what resonates most with them will help her find innovative and creative ways to reach and engage a teen audience.
Pilgreen championed Williams’s efforts to reach teen audiences across eastern North Carolina. “We are so fortunate to have D’Nise’s mental health background and expertise to better inform the education that we are offering, and to ensure that we are connecting with teens on a ‘real life’ level. My perception of a teens experience isn’t necessarily reality, and D’Nise knows that hers isn’t either. D’Nise is very intentional in bringing youth voices to her work, and structuring her programming and activities in a way that best impacts them.”
Williams emphasized that while the program’s focus on safe teen driving centers on a few counties each year, she is always available to speak to groups and do targeted programming and interventions. “I never turn down the opportunity to encourage kids to be safer,” she said.

Dr. Jacob Pierce
Fall is upon us, and along with the cooler weather and changing leaves, we are expecting to see an increase in respiratory viruses. While it might be too late for ECU football’s conference championship dreams, it’s not too late to increase your chances of staying healthy this respiratory viral season. Respiratory viruses may be an inconvenience for many of us, but they can be devastating for those with certain conditions. Fortunately, vaccines and treatments are available for the major respiratory viruses expected to be circulating this Fall and Winter.
Testing positive for influenza, COVID-19, RSV and other respiratory viruses can be unsettling, but it’s important to remember that we’re equipped with the knowledge and tools to handle it effectively. If you test positive, reach out to your health care provider immediately. For those who are a bit more vulnerable—like older adults, people with underlying health conditions or a weakened immune system—getting early treatment really makes a difference. It can help keep symptoms from getting worse and get you back on your feet faster.
Medications available today for some respiratory viruses like COVID-19 can significantly reduce the severity of symptoms and lower the risk of hospitalization. As an infectious disease physician at ECU Health, I have seen firsthand how devastating these respiratory viruses can be for at-risk individuals. This underscores the importance of acting quickly and taking advantage of these treatments when eligible.
Treatment is just one part of the equation; preventative measures remain as vital as ever. The 2024–25 COVID-19 and influenza vaccines are available this Fall, and staying up to date with vaccinations is one of the most effective ways to protect yourself and those around you. We also now have FDA-approved RSV vaccines for all adults ages 75 years and older. The Centers for Disease Control and Prevention (CDC) also recommends the vaccine for adults ages 60-74 years who are at increased risk of severe RSV.
It is important to recognize that some of the most vulnerable in our community – such as newborns or individuals on chemotherapy don’t have a strong enough immune system for vaccines to work. They rely on the healthy among us to get vaccinated and keep them safe. I know that some of you reading this may have concerns about vaccinations. I encourage you to discuss which vaccines might be right for you with your health care provider. I get my vaccines every year, not to protect myself, but to protect anyone in our community who cannot get them for whatever reason.
Additionally, basic hygiene practices, like frequent handwashing, avoiding close contact with sick individuals and wearing masks in crowded or high-risk areas, continue to be simple yet powerful tools in preventing the spread of respiratory viruses.
By staying informed, acting quickly when needed and embracing preventive measures, we can navigate this season safely and protect the health of our community. It’s not just about avoiding illness; it’s about doing our part to ensure the well-being of those around us. Together, we can make a difference in managing this year’s respiratory viral season and look forward to baseball season.
Dr. Jacob Pierce is the medical director of infection prevention at ECU Health and a clinical assistant professor at the Brody School of Medicine at East Carolina University.
Across the ECU Health system, hospitals recognized Veterans Day with events honoring those who have served our nation and thanking those who have chosen to serve in a new way at ECU Health.
At ECU Health Medical Center in Greenville, team members gathered around the flagpole just after 9 a.m. to come together, connect with other veterans, and appreciate one another’s service to the country and eastern North Carolina.
Dr. Virginia Hardy, vice president and chief inclusion and belonging officer at ECU Health, hosted the event and welcomed in team members.
“Today, we celebrate not only your past service, but also your legacy of courage and honor,” she said. “Our veterans remind us that our freedom is not just a right, it is a responsibility. Freedom today means different perspectives, engaging and constructive dialogue and ensuring that every voice has been heard.”

Cameron Graham, manager of electrical and mechanical systems in Plant Operations at ECU Health, gave a roll call for each branch of the United States military with veterans responding with their branch battle cry.
He shared that his service in the Navy helped shape his perspective as a leader and in his daily work at ECU Health.
“My brother was in the service, also in the Navy, and he was kind of my hero, so I followed his tracks,” Graham said. “When I attained the rank of Chief, we used to do what was called an initiation. You’re taught humility, to never forget from whence you came, and those who made you who you are. That has served me well, not only in the military but at ECU Health as well.”
Wayne Waters, a mechanic with Plant Operations at ECU Health, led the Pledge of Allegiance during the event. He served in the National Guard and said he took lessons from his time in the service that he sees in his work each day at ECU Health.
“A lot of my family in the past had been military, so growing up it was just the right thing to do. I’m just proud to be a part of the service,” Waters said. “Being young and going in, it helped me with structure in my life. It really taught me to be team player, being part of a team and working together.”
Trish Baise, chief nursing executive at ECU Health, said as the daughter of a veteran, she’s proud to participate in these events and recognize others for their service and sacrifice.
She said the sense of service in those who serve in the military does not fade and we see that each day in eastern North Carolina and at ECU Health.
“Our neighbors, friends and family members who have served often return home to continue their legacy of services,” Baise said. “They become teachers, first responders, health care professionals and community leaders. The sense of commitment is part of what makes eastern North Carolina unique – a place where selflessness and service are not just values, but a way of life.”
At ECU Health, we’re grateful today and every day for the service of our veterans. We’re proud of the more than 550 ECU Health team members and 60 medical students, faculty and staff at the Brody School of Medicine who have decided to continue their service to others after their time in the military.



Halloween is a night filled with fun, creativity, and spooky thrills, but it is also an important reminder of easy safety tips, especially for pedestrians. It is essential for parents, guardians and children to take proactive measures to ensure everyone is safe while enjoying the festivities.
“One of the most effective ways to increase visibility and reduce risks is for children and accompanying adults to wear reflective items,” advised Ellen Walston, injury prevention program coordinator at ECU Health.
Selecting costumes that fit properly can help prevent tripping hazards. Parents should ensure that their child’s costume is the appropriate length and consider opting for face paint instead of masks to avoid obstructed vision.

Simple additions, such as a reflective vest or armband for parents, can significantly enhance safety for both children and adults. Additionally, carrying flashlights or glow sticks can alert oncoming traffic to the presence of trick-or-treaters. In neighborhoods without sidewalks, staying as far from traffic as possible and utilizing crosswalks when crossing streets is crucial.
Walston emphasizes the importance of communication between drivers and pedestrians.
“Parents should also encourage children to make eye contact with the driver,” said Walston. “It is important that both the driver and the child are aware of one another.”
Safety in numbers is another critical aspect of Halloween safety. Walston recommends that children trick-or-treat in groups rather than alone. Parents should supervise younger children, while older kids should stay together with their peers.
“Children should travel in groups with smaller children, with their parents available for supervision,” Walston said.
This approach not only improves safety but also builds a sense of community among families, according to Walston. Furthermore, parents should remain vigilant about their surroundings and teach their children to be aware of potential dangers.
Once the trick-or-treating is done, parents should thoroughly inspect all candy before allowing children to indulge. Walston advises disposing of any candy that are missing wrappers or anything that appears to have been tampered with. Walston also suggests avoiding homemade treats unless they come from someone you know.
By taking these precautions and remaining vigilant, families can enjoy a safe and festive Halloween experience. With a little preparation and awareness, you can embrace the Halloween spirit without compromising safety.
Access East is a 501(c)(3) that strives to improve health access to, and coordination of, quality care in eastern North Carolina. Access East serves as an important part of the ECU Health system of care, offering support for under- and uninsured individuals and helping navigate the health care system through service lines such as Access East Care Management, HealthAssist, ACA Navigators and Health Opportunities Pilot.
Out in the field
One such facet of their service comes through the Farmworker Program, which works not only to help enroll members of the ENC H-2A (temporary visa) farmworker community in low-cost insurance, but also to direct them to available community health care options, and to provide emergency medical training like wound care or cardiopulmonary resuscitation (CPR). In just under two months, the program has reached more than 2,000 farm workers.
Juan Allen, a community coordinator and Affordable Care Act (ACA) navigator for the program, plays a key role in helping the farmworker community receive the services and care it needs. “I’ve been with Access East for seven or eight years,” Juan said. “I was born and raised in El Salvador on a farm, which is what got me interested in doing this work.” The goal of the program, he said, is to help members of the migrant farming community prevent injuries and illness. “Last year we lost four farm workers to heat stroke, and someone else passed away because no one in the field knew CPR,” he explained.

“So, we go out to the farms and do CPR training, heat exhaustion and heat stroke education, Stop the Bleed training, education about tobacco sickness and anything else they need.” Juan said there is also skin cancer education and screenings, dental cleanings, mental health support and vaccines. “During COVID, we were coordinating vaccines, so that with providers’ help, we got 80-100 people vaccinated per day.”
Juan has also trained as an instructor for the Mental Health First Aid (MHFA) trainings, which is an evidence-based, early-intervention course that, virtually or in-person, uses community-specific scenarios, activities and videos to teach people the skills they need to recognize and respond to mental health and substance use challenges. The ECU Health Foundation awarded funding to Safe Communities Coalition, a non-profit that works alongside the Eastern Carolina Injury Prevention Program (ECIPP) to prevent injuries. “Juan has reached a population (farmworkers) that we have struggled to reach, yet we knew desperately needed the education,” said Sue Anne Pilgreen, the executive director for the Safe Communities Coalition, the manager of the ECIPP and the manager of the Pediatric Asthma Program. “This past fiscal year, we have trained a total of 196 people in MFHA, and 92% felt like they could recognize someone who was suicidal after completing the class.”
“Juan is one of the hardest workers I know,” said Shantell Cheek, the director of Access East. “He has a passion to really help those who are underserved, and he is a true link between Access East, ECU Health and the Farmworker Program.” Wherever there is a need, she said, Access East and the Farmworker Program is there.
The program, which initially was established to help H-2A workers get visas and enroll in the ACA, has grown significantly. “We still do the ACA enrollment,” Cheek said. “But Juan provides care coordination, and different entities like the North Carolina Department of Health and Human Services and the North Carolina Growers Association partner with us. We now help these individuals get medications they need, assist them when they go to the hospital and are being discharged, set up with primary care providers and provide the education like CPR and skin cancer. And it’s not just the migrant workers; it’s their families too. Wherever there is a need, anywhere across the state, they call Juan.”
Partnering with the Brody School of Medicine
 She emphasized that Juan tirelessly creates partnerships with regional and community organizations. Shantell also highlighted Access East’s, and Juan’s, ongoing collaboration with East Carolina University’s Brody School of Medicine. “During their first or second year of medical school, students can select a project to work on and Juan’s name often comes up when they mention an interest in the communities we serve.”
She emphasized that Juan tirelessly creates partnerships with regional and community organizations. Shantell also highlighted Access East’s, and Juan’s, ongoing collaboration with East Carolina University’s Brody School of Medicine. “During their first or second year of medical school, students can select a project to work on and Juan’s name often comes up when they mention an interest in the communities we serve.”
Deanna Torres, a second-year medical school student at the Brody School of Medicine, worked with Juan this past summer as a part of a project required of the school’s four Distinction tracks. Deanna opted to apply for the Service-learning track, which is what led her to Access East. The other tracks include Health System Transformation and Leadership, Medical Education and Teaching and Research.
Deanna said she has always had a passion for grassroots community service. “I’m undecided on my specialty right now, but I know I want to help underserved, minority populations.” Deanna grew up participating in a variety of community service activities, including a medical mission to Honduras and a Benedictine Volunteer Corps trip to the Rosebud Indian Reservation in Mission, South Dakota. Once she entered medical school, Deanna continued her journey in service by joining the Service-learning track. “It isn’t required to join a track,” Deanna explained. “But when I was applying to medical schools, the Service-learning track was a major factor in deciding to come here.”
Students in the Service-learning track work extensively with medically-underserved, marginalized and rural populations during their medical school career. They attend a lecture series specific to that track, but they are also required to participate in a service-learning internship during the summer after their first year of medical school. “We select an organization to partner with, and then we create a longitudinal service-learning project aligned with that organization,” Deanna said. While the internship only lasts a summer, the students’ work on their projects continues until they graduate.
Making a difference
With Juan as her mentor, Deanna said she gained an insider’s perspective on a migrant farmworker’s daily life. “I saw how migrant farmworkers are processed after entering the country. I saw how farms are laid out, and I got to see their living conditions, which aren’t always great. I’ve lived in North Carolina my whole life, and I didn’t know how many farmworkers we have in this region or what their needs were.” This exposure led Deanna to her project’s focus, which is “Increasing Mental Health Services to Hispanic Migrant Farmworkers in Pitt County.” The migrant workers, she discovered, often struggle with mental health issues, like depression. “They leave their home country and their families, work in the heat and have no car or independence, and that can be challenging. I want to advocate for the lack of awareness and communication about mental health in the Hispanic community,” Deanna said.
Juan has been instrumental in helping Deanna make the connections and partnerships necessary to work on her project. “He’s a popular man,” she laughed. “Any time I mention Access East, everyone knows him.” Deanna said she appreciated Juan being willing to mentor her, despite his busy schedule. “As a medical student, it can feel daunting to reach out because everyone is busy, but he was always available and offered me resources, took me to the farms and provided logistics. He knows all about these things.”
Dr. Jennifer Crotty, a pediatrician and an associate professor in the Department of Pediatrics at the Brody School of Medicine, as well as the director of the Service-learning distinction track, facilitates connections between students in the Service-learning track and community partners. “The track primarily focuses on local impact and grassroots efforts,” Dr. Crotty said. Of how she came to direct this specific track, she cited her background in pediatrics. “I realized that to have healthy children, we need healthy families and communities,” she said. “That’s why we want to do this advocacy work.” Access East has been a significant partner in this work. “Access East addresses the things we know need to be addressed. When students work with them, they see the time and energy and resources it takes to do medicine in these rural communities.” While she has never met Juan personally, she knows her students get a great experience when they work with him. “He always finds a place for our students, and the students always say their experience was amazing.”
This work is valuable, Deanna said, because it puts a face and name to abstract medical concepts students learn in school. “It puts a story to what you’re learning,” she said. “It shows us that a patient isn’t just one disease, but they are dimensional, and it helps us be better physicians who treat in a holistic manner. This community needs us to advocate for them.” Dr. Crotty agreed, saying that having students participate in these service learning partnerships through ECU Health make them better physicians, no matter what specialty they choose. “They take the knowledge they gained through service learning to wherever they’re going. I love that someone in their surgery residency is thinking about whether their patient has enough food at home. We graduate good doctors because our students are exposed to these types of things, and they know how to handle it.” Juan said that ultimately, this work gives migrant farmworkers a voice. “They’re only here for eight months and they don’t know their rights,” he said. “Access East is vital to reach out to farm workers so we can be a go-between them and the health system.”


