Greenville, N.C. – ECU Health Medical Center has been nationally recognized as a national leader in patient experience for the second consecutive year, according PEP Health’s 2025 rankings. PEP Health evaluated more than 35 million online reviews from patients and their families in 2024, offering a real-time look at patient experiences across health care providers nationwide.
ECU Health Medical Center’s recognition was highlighted by top-5 national rankings in several categories including overall patient experience, communication & involvement and emotional support.
“At ECU Health, creating caring experiences for our patients and team members is at the core of our mission,” said Dr. Julie Kennedy Oehlert, chief experience officer at ECU Health. “Our definition of excellence is shaped by feedback from our patients and fostered by the compassion and dedication of our team. Being recognized nationally for our excellence in communication and emotional support is a rewarding acknowledgment of the safe, healing environments we strive to create. We are committed to continually listening and evolving to meet the needs of those we are honored to serve.”

PEP Health’s 2025 Rankings focus on hospitals with at least 750 staffed beds and at least 250 patient experience comments left online between Sept. 1, 2023, and Sept. 1, 2024. These comments, sourced from patients and their families on social media and review platforms, were analyzed against seven internationally recognized domains of patient-centered care: fast access, effective treatment, emotional support, communication & involvement, attention to physical and environmental needs, continuity of care, and billing and administration.
According to PEP Health, research has shown that enhancing patient experience is not only associated with improved care outcomes, but also strengthens financial performance, safety and health equity. Positive patient experiences directly impact CMS Star Ratings, which are closely tied to reimbursement rates and play a critical role in driving new patients and increasing patient retention. ECU Health’s commitment to delivering exceptional care in eastern North Carolina ensures that the most vulnerable populations in receive the support and attention they need.
“This recognition is a testament to the unwavering dedication of our team members who bring compassion and empathy to every patient interaction,” said Brian Floyd, chief operating officer, ECU Health. “Caring for patients during some of life’s most challenging moments is more than a job – it’s a calling. I am incredibly proud of the heart and commitment our team demonstrates every day. Earning this national recognition for patient experience reflects their hard work and the trust our patients place in us, and we will continue to prioritize compassionate, patient-centered care in all we do.”
Greenville, N.C. – ECU Health performed the first ever pacemaker implantation with Elutia’s EluPro® BioEnvelope on Sept. 5. EluPro, a Food and Drug Administration (FDA)-approved device, is the first antibiotic-eluting device designed to prevent post-operative complications for Cardiac Implantable Electronic Devices (CIEDs) such as pacemakers and defibrillators.
“We are proud to be the first to perform a pacemaker implantation with the EluPro BioEnvelope, which is a testament to the work our cardiovascular teams do every day to improve the health and well-being of eastern North Carolina,” said Jay Briley, president, ECU Health Medical Center. “Being the first to perform this groundbreaking procedure with the EluPro BioEnvelope underscores our commitment to bringing cutting-edge solutions directly to the communities we serve. Our patients can access the highest level of care without the need to travel long distances, ensuring that advanced cardiovascular treatments are available right here in eastern North Carolina.”

For high-risk patients, including those with underlying health conditions or advanced age, traditional pacemakers carry a risk of complications such as infection, migration and skin erosion, affecting five to seven percent of patients nationwide, according to the FDA. These issues arise when the body’s immune system treats the device as a foreign object, leading to inflammation, device movement, and, in some cases, serious infections. The EluPro BioEnvelope offers an innovative solution for high-risk patients by combining antibiotic therapy with advanced tissue engineering.
“Eastern North Carolina faces high rates of chronic illnesses like heart disease, diabetes and hypertension, making access to advanced cardiovascular care crucial for our community,” said Dr. John Catanzaro, John “Jack” Rose distinguished professor and chief of the Division of Cardiology at the Brody School of Medicine at East Carolina University and director of the East Carolina Heart Institute at ECU Health Medical Center. “Patients with co-morbidities are at higher risk for infection after procedures like pacemaker implantations, and this new technology is a significant step forward in addressing these challenges, as it not only improves patient outcomes but also helps prevent complications that can arise from traditional procedures. I am grateful to the team that helps bring innovations like the EluPro BioEnvelope to our region, demonstrating our commitment to reducing health disparities and ensuring our patients receive the best care possible.”
ECU Health team members that were part of the new procedure include: John Catanzaro, MD, MBA, Jan Lopes, MD, Mark Dixon, RN, David Rouse, cardiovascular technologist, and Tracy Fulcher, cardiovascular technologist. As the academic health system for eastern North Carolina, ECU Health and the Brody School of Medicine perform nearly 1,000 pacemaker implantations per year and ensure patients benefit from the latest medical innovations without having to travel far from home. This integration of academic expertise and clinical care not only enhances patient outcomes but also serves as a vital resource for training the next generation of health care professionals. ECU Health’s commitment to leading the way in advanced cardiovascular treatments demonstrates our ongoing mission to address rural health disparities and improve the well-being of the communities we serve.
Greenville, N.C. – The Eastern Carolina Injury Prevention Program (ECIPP) at ECU Health Medical Center was awarded the Safe States Injury and Violence Prevention Achievement Award at the Safe States 2024 Injury and Violence Prevention (IVP) Professionals Annual Conference in Portland, Oregon on Aug. 20-22. Safe States recognizes the outstanding achievements of members and partners annually through peer-nominated awards.
“We are incredibly proud of the recognition ECIPP’s initiatives have received,” said Sue Anne Pilgreen, manager, ECIPP, ECU Health. “This award highlights our team’s leadership and expertise in injury prevention and advancing safety practices locally and nationally. While this recognition is encouraging, what truly motivates the ECIPP team is getting to see the impact that this work has on the members of our community as we remain dedicated to promoting safety, encouraging healthy behaviors and reducing injuries.”
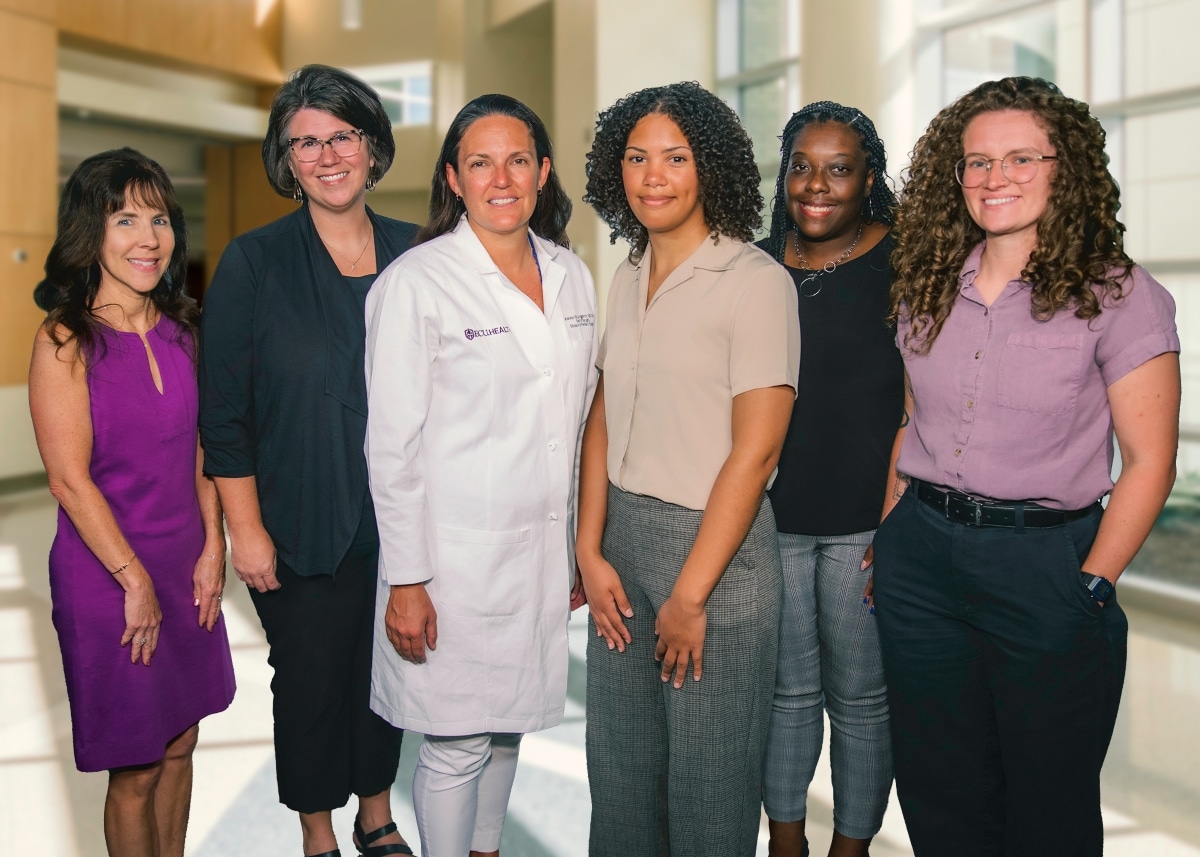
Established in 1995, ECIPP is a collaborative prevention focused health program at ECU Health Medical Center. Partnering with the ECU Health Trauma Center, the James and Connie Maynard Children’s Hospital and the Brody School of Medicine‘s Department of Emergency Medicine, ECIPP is dedicated to improving the health of eastern North Carolina by reducing the incidence and impact of injuries. The American College of Surgeons noted the value of ECIPP’s work in the verification of Maynard Children’s Hospital as a Level I Pediatric Trauma Center.
ECIPP has been instrumental in the development, implementation and interdisciplinary adoption of injury prevention practices for children and adults across eastern North Carolina. ECIPP offers a wide range of prevention programs aimed at addressing the most pressing injury concerns in the region. These programs include education on child safety, teen safe driving, hot car safety, firearm safety, suicide prevention, traffic safety and poison prevention. ECIPP also partners with Greenville Police Department on the Greenville Traffic Safety Task Force, which earned a national achievement award in 2023.
By building innovative partnerships, ECIPP has successfully promoted the adoption of injury prevention practices across various industries. For instance, the firearm safety program collaborates with wildlife organizations and pawn shops to provide education and gunlocks, while partnerships with Community Health Workers help deliver bike safety education and helmets. ECIPP also created an LGBTQ+ youth suicide prevention documentary that has been integrated into college curricula and hospital onboarding processes. From 2020 to 2023, ECIPP reached 86,333 individuals, distributing 2,405 gun locks, 256 medication lock boxes, 3,204 bike helmets and 259 child car seats.
“ECIPP’s strategies and partnerships have been crucial in expanding education and resource access in rural eastern North Carolina communities,” said Catherine Nelson, senior administrator of Community Health Programs, ECU Health. “This award is a testament to our commitment to injury prevention and the positive impact we’ve made for children and families across the region. By collaborating with local organizations and leveraging innovative approaches, we’ve been able to address critical issues, ultimately advancing the health and safety of our communities.”
To learn more about ECIPP, visit the webpage.
Greenville, N.C. – Nineteen ECU Health nurses have been named part of the Great 100 Nurses of North Carolina by the Great 100 Nurses of North Carolina Board of Directors. The recipients are recognized for their outstanding professional ability and contributions to improving health care services in their communities.
“ECU Health nurses have devoted their careers to caring for others and serving our community with exceptional dedication,” said Trish Baise, chief nursing executive, ECU Health. “I am so proud of the amazing nurses recognized by the Great 100. Thank you to this year’s honorees and to every member of the ECU Health nursing team. Your commitment to delivering excellent, compassionate care each day exemplifies our mission and makes a profound difference in the lives of those we serve.”

Since 1989, The North Carolina Great 100, Inc. has recognized and honored nurses around the state for their commitment to excellence and to promote a positive image of the nursing profession. Each year, the Great 100 Nurses of North Carolina Board of Directors asks patients, health care workers, friends and family members to nominate an outstanding nurse practicing in North Carolina. Thousands of nominations are reviewed, and 100 nurses are selected and honored at a statewide gala.
The ECU Health nurses chosen as Great 100 Nurses of North Carolina in 2024 are:
Kayla E. Anderson, BSN, RN, CEN
 Kayla E. Anderson, BSN, RN, CEN, is an education coordinator at the Center for Learning and Performance at ECU Health Beaufort Hospital, a campus of ECU Health Medical Center. She has dedicated seven years to ECU Health. She holds a bachelor’s degree in nursing from Winston-Salem State University and is pursuing a master’s degree in nursing education at the University of North Carolina at Wilmington. Board certified in emergency nursing, Kayla also holds provider certifications in Advanced Cardiovascular Life Support (ACLS) and Pediatric Advanced Life Support (PALS), along with instructor certifications in Basic Life Support, Advanced Stroke Life Support and Nonviolent Crisis Intervention. She is an active member of the Sigma Theta Tau International Honor Society of Nursing.
Kayla E. Anderson, BSN, RN, CEN, is an education coordinator at the Center for Learning and Performance at ECU Health Beaufort Hospital, a campus of ECU Health Medical Center. She has dedicated seven years to ECU Health. She holds a bachelor’s degree in nursing from Winston-Salem State University and is pursuing a master’s degree in nursing education at the University of North Carolina at Wilmington. Board certified in emergency nursing, Kayla also holds provider certifications in Advanced Cardiovascular Life Support (ACLS) and Pediatric Advanced Life Support (PALS), along with instructor certifications in Basic Life Support, Advanced Stroke Life Support and Nonviolent Crisis Intervention. She is an active member of the Sigma Theta Tau International Honor Society of Nursing.
Kimberly Askew, RN
 Kimberly Askew, RN, is staff nurse III at ECU Health Roanoke-Chowan Hospital. She began her journey at the hospital 19 years ago as a certified nursing assistant. It was her dream to be a Labor and Delivery nurse like her mother, who has served as a great inspiration for her. In her 15 years of nursing, she has served as a charge nurse, preceptor, childbirth educator, unit educator and an Advanced Life Support in Obstetrics (ALSO) instructor. During her years in Labor and Delivery, she helped the hospital achieve its 4 Star Breastfeeding Friendly designation. Since transitioning to peri-operative services, Kimberly has found enjoyment in creating a safe and comfortable environment for those who choose or require surgical services.
Kimberly Askew, RN, is staff nurse III at ECU Health Roanoke-Chowan Hospital. She began her journey at the hospital 19 years ago as a certified nursing assistant. It was her dream to be a Labor and Delivery nurse like her mother, who has served as a great inspiration for her. In her 15 years of nursing, she has served as a charge nurse, preceptor, childbirth educator, unit educator and an Advanced Life Support in Obstetrics (ALSO) instructor. During her years in Labor and Delivery, she helped the hospital achieve its 4 Star Breastfeeding Friendly designation. Since transitioning to peri-operative services, Kimberly has found enjoyment in creating a safe and comfortable environment for those who choose or require surgical services.
Dennis Campbell II, DHA, RN, FACHE
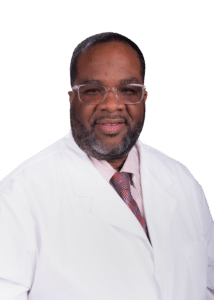
Dennis Campbell II, DHA, RN, FACHE, joined ECU Health Beaufort Hospital in December 2020 as vice president of Patient Care Services. He was named president in September 2023 after serving as interim president since February of that year. Dennis also serves as the interim president at ECU Health North Hospital, a position he has held since August 2024. Dennis began his health care journey as an intensive care registered nurse in 2004. Over the course of a progressive career, he has matriculated to the C-suite while gaining valuable experience in a variety of senior leadership and executive roles in nursing, quality, operations and compliance in North Carolina and Georgia. Dennis is a highly visible and collaborative leader skilled at navigating complex health systems to solve problems and execute strategic plans to deliver desired outcomes. He is a relationship builder who understands the value of relationships in developing strategies to promote health and wellness in the communities served. Dennis holds an associate and bachelor’s degree in nursing, a master’s degree in management and a doctorate degree in health care administration.
Gina Coldwell, BSN, RN-BC
Gina Coldwell, BSN, RN-BC, is a staff nurse II on the Neuroscience Intermediate Unit at ECU Health Medical Center. She has worked on this unit for the past five years. Gina earned her associate degree in nursing from Edgecombe Community College and her bachelor’s degree in nursing from East Carolina University. She is currently enrolled in the Family Nurse Practitioner master’s program at Carson-Newman University. She is medical-surgical board certified. Gina is a proud mother of four adult children and grandmother of five grandchildren.
Katie Elliott, BSN, RN, CRRN

Katie Elliott, BSN, RN, CRRN, is a staff nurse IV in the Radiation Oncology Clinic at ECU Health Medical Center and has been with the hospital for 15 years. Katie received her associate degree in nursing from Beaufort County Community College and her bachelor’s degree in nursing from Fayetteville State University.”. Katie is a certified rehabilitation registered nurse, serves as a co-chair on the ECU Outpatient Oncology Unit Based Council and is an active member of the Sigma Theta Tau International Honor Society of Nursing. In addition, Katie serves on ECU Health’s Coordinating Council and Environmental Council.
Alex Gilbert, BSN, RN, CCRN

Alex Gilbert, BSN, RN, CCRN, is a staff nurse III in the Surgical Intensive Care Unit (SICU). Alex has worked at ECU Health Medical Center for seven years and has spent time between the SICU and ECU Health EastCare as a flight nurse. Alex earned his bachelor’s degree in nursing from East Carolina University and obtained his critical care RN specialty certification. Alex is active in the community as an EMT-B and volunteering with community organizations in eastern North Carolina.
Rebecca Hagee, BSN, RN
Rebecca Hagee, BSN, RN, is a staff nurse III in the Surgical Oncology Clinic at ECU Health Cancer Center. Rebecca has worked for ECU Health Medical Center for six years. She earned her associate degree in nursing at Pitt Community College, and her bachelor’s degree from the University of North Carolina at Wilmington.
Brittany Harriett, BSN, RN

Brittany Harriett, BSN, RN, is the assistant nurse manager on the Medical Unit at ECU Health Beaufort Hospital. She was the recipient of the 2022 Juanita Jackson award and a nominee for the 2024 Susan Gerard Excellence in Leadership award. She has worked with ECU Health for nine years. Brittany also works part time at the East Carolina University College of Nursing as a nurse consultant. Brittany earned her associate degree in nursing from Beaufort County Community College and her bachelor’s degree in nursing from Capella University. Outside of health care, Brittany is the mom of two active boys. They share a love for baseball, family time and their church.
Tracy Hobbs, BSN, RN-BC

Tracy Hobbs, BSN, RN-BC, is an assistant manager for the 3 East Hospitalist Unit at ECU Health Medical Center. She has worked at ECU Health Medical Center for the duration of her 27-year career. Tracy earned her bachelor’s degree in nursing from Barton College. She is specialty certified in medical-surgical nursing. She is active in endeavors to create positive change for the future of nursing at ECU Health Medical Center.
Kathryn Jarvis, DNP, RN, NPD-BC

Kathryn Jarvis, DNP, RN, NPD-BC, is the senior director for Children’s Services at Maynard Children’s Hospital. She has been a nurse at ECU Health Medical Center for 12 years with experience in pediatrics, nursing education and nursing leadership. Kathryn earned her bachelor’s and master’s degrees in nursing from East Carolina University and her Doctor of Nursing Practice (DNP) degree with a concentration in nurse executive leadership from the University of North Carolina at Wilmington. She has also obtained specialty certification in nursing professional development. In addition to her role as senior director of Maynard Children’s Hospital, Kathryn is a part-time faculty member for East Carolina University’s Doctor of Nursing Practice program. Kathryn thoroughly enjoys her roles, as she has a passion for both nursing leadership and education.
Jennifer Lewis, BSN, RN

Jennifer Lewis, BSN, RN, is the outreach coordinator for ECU Health Medical Center Cancer Care. Jennifer has practiced nursing for 27 of the 32 years she has worked for ECU Health. Prior to transitioning to her current role in 2021, Jennifer worked at ECU Health Beaufort Hospital, a campus of ECU Health Medical Center in various inpatient and outpatient settings. Jennifer earned her associate degree in nursing from Beaufort County Community College and her bachelor’s degree in nursing from the University of North Carolina at Wilmington. Jennifer believes in the value of cultivating strong partnerships with churches, businesses, schools and civic organizations to promote awareness regarding the prevention and early detection of cancer.
Jessica Noble, MSN-NE, RNC-EFM

Jessica Noble, MSN-NE, RNC-EFM, is a registered nurse with over 20 years of experience in maternal health. She currently serves as the perinatal nurse champion and navigator for ECU Health, advocating for equitable perinatal care in eastern North Carolina. Jessica holds a bachelor’s degree in nursing from East Carolina University and a master’s in nursing education from the University of North Carolina at Wilmington. Jessica leads the “I Gave Birth” bracelet program and contributes to the Perinatal Quality Collaborative of North Carolina initiatives. An active member of the Association of Women’s Health, Obstetric and Neonatal Nurses, she has presented at conferences, co-authored a North Carolina Medical Journal article and serves on the North Carolina Department of Health and Human Services Maternal Health Task Force.
Amber Oakes, BSN, RN
Amber Oakes, BSN, RN, is a staff nurse IV in the Gynecologic Oncology Clinic at ECU Health Medical Center. Amber has worked at ECU Health for 14 years. Amber earned her associate degree in nursing from Pitt Community College and later obtained her bachelor’s degree in nursing from Western Carolina University.
Lou Ann Proctor, BSN, RN, CCRN

Lou Ann Proctor, BSN, RN, CCRN, is a staff nurse IV in the Pediatric Intensive Care Unit at ECU Health Medical Center and has been a nurse for 35 years. She holds a bachelor’s degree in nursing from the East Carolina University College of Nursing. She has been a member of American Association of Critical Care Nurses – Critical Care Registered Nurse for 18 years, Pediatric Advanced Life Support (PALS) instructor, charge nurse and a preceptor.
Deborah Rice, BSN, RN
Deborah Rice, BSN, RN, is a staff nurse III in the Palliative Care Unit at ECU Health Medical Center. She has worked for ECU Health for more than four years. Deborah earned her bachelor’s degree from East Carolina University. Deborah works as a charge nurse, clinical coach and quality lead for her unit. Deborah also works as an adjunct clinical instructor for Pitt Community College and is a member of North Carolina Nurse Association.
Elizabeth Seawell, MSN, RN-BC, NPD-BC

Elizabeth Seawell, MSN, NPD-BC, RN-BC, is the manager of the ECU Health Medical Center Trauma Program. Elizabeth has worked at ECU Health Medical Center for 16 years with experiences as a surgical/trauma staff nurse and professional development specialist. Elizabeth obtained both her bachelor’s degree in nursing and master’s degree in nursing education from East Carolina University. Elizabeth has specialty certifications in medical-surgical nursing and nursing professional development. Elizabeth is actively involved in the development and growth of the eastern North Carolina Nursing Honor Guard, Trauma Survivors Network, Professional Practice Council and other local community activities.
Myra Barnes Thompson, MSN, RN, CNML

Myra Thompson, MSN, RN, CNML, is the nurse manager of the Medical Intensive Care Unit and the Continuous Renal Replacement Therapy Program at ECU Health Medical Center. Myra has worked at ECU Health Medical Center for 17 years. Myra earned her bachelor’s degree from East Carolina University and her master’s degree from Western Governors University. Myra obtained her specialty certification as a certified nurse manager and leader from the American Organization for Nursing Leadership.
Virginia C. Tripp, BSN, RN, NPD-BC

Virginia “Ginny” Tripp, BSN, RN, NPD-BC, practices as a professional development specialist in the Center for Learning and Performance at ECU Health Medical Center. Ginny has been a registered nurse for 30 years and has served at ECU Health Medical Center for the past 15 years. She earned her associate degree in nursing at Craven Community College and her bachelor’s degree in nursing at East Carolina University. Ginny has obtained specialty certifications in the fields of case management and in nursing professional development. Ginny’s passion is to elevate the profession of nursing and encourage and support others in achieving their highest potential. Her highest purpose is to please God and fulfill her God-given calling in nursing by being a blessing in others’ lives each day. She is an active member of the ECU Health Medical Center Nursing Professional Development Council.
Kelly Trout, RN, OCN

Kelly Trout, RN, OCN, is a staff nurse III in the Medical Oncology Unit at ECU Health Medical Center. She has been a nurse on Medical Oncology for 15 years and has obtained specialty certification as an oncology certified nurse. She serves as a charge nurse and clinical coach on her unit. She is also the head of the Medical Oncology Retention Council and has started programs on her unit, such as the HOPE Christmas workshop for immunocompromised oncology patients. She is an active member of the Oncology Nursing Society.
Greenville, N.C. – East Carolina University’s College of Nursing and ECU Health are launching an Adult Gerontology Acute Care Nurse Practitioner program, a new graduate-level certificate program that will prepare more specialized nurse practitioners in acute care settings across the state.
“We have a lot of nurse practitioners in North Carolina who are doing amazing work to care for patients in ICUs and other very demanding care sites, we also want to expand the knowledge, skills and abilities of current practitioners because the need is so high and the shortage of providers is so great,” said Dr. Julie Linder, chair of the Advanced Nursing Practice and Education department. “This new program will provide the didactic and clinical experiences necessary to meet the needs of our patient populations.”
According to the American Association of Nurse Practitioners, only 6.1% of nurse practitioners specialize in adult gerontology acute care.

The aging population is growing nationally, along with an ongoing shortage of health care workers. The collaboration between the College of Nursing and ECU Health bolsters the health care workforce in eastern North Carolina, enhances health outcomes and increases access to specialized care for older adults in these communities.
“ECU Health values its strong partnership with ECU and the College of Nursing, especially in addressing the national health care workforce shortage,” said Pam Rudisill, vice president of nursing excellence at ECU Health. “Our success as an academic health system relies on bridging clinical and academic excellence to provide high-quality care to eastern North Carolina. Eastern North Carolina depends on collaborative solutions from institutions like ECU Health and ECU to meet the needs and improve the health and well-being of our region.”
ECU Health’s Chief Nursing Office will support their employees by offering tuition reimbursement as a commitment to support the certificate program and help employees advance their education and skills.
The first cohort of ECU’s Adult Gerontology Acute Care Nurse Practitioner certificate program will begin classes in Spring 2025. Students who complete course requirements on the recommended plan of study should graduate in May 2026. Upon graduation, these students will be eligible to take a specialty exam to become certified as Adult Gerontology Acute Care Nurse Practitioners.
The application deadline for that first cohort is Dec. 15, 2024, and applicants can find application requirements and procedures, along with required courses in the curriculum, here.
The certificate program is a post-master’s program, which means applicants must already be recognized as an advance practice nurse. The education students will receive will provide them with the skills to work in acute care settings. ECU offers pre-requisite courses if prospective students have not already completed them.
“We invite prospective students to contact us in the event they need pre-requisite courses prior to beginning their core class work,” Linder said.
ECU’s College of Nursing and ECU Health previously developed pathways for the development of the future of nursing care in eastern North Carolina with the establishment of an academic-practice partnership, seeded by a $1.5 million investment from ECU Health over five years. This investment has provided the ECU College of Nursing with the opportunity to hire faculty, staff, and purchase resources to support students in the Adult Gerontology Acute Care Nurse Practitioner certificate program.
The first cohort will comprise approximately 12 students, with a minimum of six seats dedicated to ECU Health employees and other slots open to applicants interested in advancing their career in critical care.
ECU will join three other nursing programs in North Carolina to offer the AGACNP certification.
Greenville, N.C. – After six years with ECU Health, including serving as president of ECU Health North Hospital since August 2020, Jason Harrell has announced his retirement effective Aug. 8, 2024. ECU Health has begun a national search for the next president of ECU Health North Hospital. Dennis Campbell II, DHA, RN, NEA-BC, will serve as interim president of ECU Health North Hospital in addition to his current role as president of ECU Health Beaufort Hospital.

Jason Harrell
“On behalf of ECU Health, I would like to thank Jason for his service and dedication to advancing our mission over the years,” said Van Smith, president, ECU Health Community Hospitals. “Jason has had a distinguished 40-year career in health care, and we are grateful for his service to ECU Health. During his time at ECU Health North, Jason’s leadership, collaboration and focus on the priorities of access, quality, experience and safety have been unwavering. ECU Health North Hospital team members, patients and the community have benefitted from Jason’s leadership accomplishments.”
Campbell, II will serve at ECU Health North on an interim basis until the national search is completed. He has been with the health system for four years, previously serving as ECU Health Beaufort’s vice president of Patient Care Services before taking on the role of president in September 2023.

Dennis Campbell II
During his time at ECU Health Beaufort, Campbell, II has prioritized developing relationships with important stakeholders and partners in the area including Beaufort Community College and ECU, exemplifying his dedication to investing in the future of academic health care in eastern North Carolina.
“Dennis’s leadership skills and deep understating of the needs of our team members and the communities we serve in eastern North Carolina will be invaluable assets to ensure the stability and ongoing success of ECU Health North Hospital during this time of transition,” Smith said. “I appreciate Dennis’s willingness to serve the system in this capacity.”
OUTER BANKS, N.C., July 24, 2024 — Outer Banks Health and Dare County Department of Health & Human Services have joined forces with Blue Zones, the global leader in longevity research and community well-being transformation, to launch Blue Zones Ignite™ Outer Banks.
Blue Zones uses an evidence-based, environmental approach to making healthy choices easier where they live and spend most of their time. Blue Zones will work with Outer Banks Health, the County, and other community leaders to conduct an in-depth feasibility assessment to determine how to make it a healthier place to live, work, and thrive. Together with the community, the Blue Zones team will assess readiness and build a plan for change.
The launch of Blue Zones Ignite is a dream come true for Christina Bowen, MD, Outer Banks Health Center for Healthy Living Medical Director, and ECU Health Chief Well-being Officer.

“We know that 20% of health and longevity is tied to genetics; while 80% is tied to where and how we live. Blue Zones Ignite Outer Banks is going to inspire us to celebrate and promote our strong sense of community while we find ways to make it even easier to eat healthy foods, move naturally and connect with our purpose – just a few of the ways we’ll continue to enhance our well-being and make this an even better place to live and work,” shared Dr. Bowen.
The Blue Zones Approach
Blue Zones employs a proven solution in collaboration with communities to help people live better and longer lives. The company’s work is based on research and principles developed by National Geographic Fellow and New York Times bestselling author Dan Buettner, who identified the cultures of the world – or blue zones regions – with the healthiest, longest-living populations.
The Blue Zones approach focuses on the single largest determinant of health: the place we live. Instead of focusing solely on individual behavior change, Blue Zones helps communities make permanent and semi-permanent changes to policies, systems, streets, surroundings, and social networks so it’s easier for residents to eat wisely, move naturally, and connect more with others as they move throughout their day. By improving the Life Radius®—the area close to home where most Americans spend 90% of their lives—Blue Zones transformations have been able to move the needle dramatically in improving overall population health and well-being. Communities that have participated in the Blue Zone’s Ignite project have seen double-digit drops in obesity and smoking rates, economic investment in downtown corridors, grant funding awards to support policies and programs to improve health equity, and measurable savings in healthcare costs.
“Together, Outer Banks Health and Dare County Health and Human Services are steadfast in our shared mission to enhance the health and well-being of all residents, so that they can live a happy, healthy and long life,” said Dr. Sheila Davies, Director Health & Human Services.
Ben Leedle, CEO of Blue Zones and Co-founder of Blue Zones Project, said: “We are excited to partner with forward-thinking leaders in the joint effort of improving well-being in the Outer Banks. That improvement, at the community level, leads to healthier and happier residents, better and more productive workforces and student bodies, and a more vibrant economy. We are excited to collaborate to create a transformation plan that can generate lasting positive change and ignite a community-wide movement towards sustained well-being.”
The Blue Zones expert team will connect with Outer Banks leaders and organizations to begin immediate work assessing the strengths, needs, and challenges that residents are facing today. Blue Zones will then create a policy-focused transformation plan that, once implemented, can drive widespread improvements in well-being, reductions in healthcare costs, and improve economic vitality in the region.
Greenville, NC — Andy Zukowski, ECU Health chief financial officer, was recently honored by Becker’s Hospital Review as one of 36 Rural Hospital CFOs to Know. Zukowski has served as CFO since 2022 and oversees the financial operations at both ECU Health and the Brody School of Medicine at East Carolina University.

Andy Zukowski, ECU Health chief financial officer
“It’s an honor to be nationally recognized for the work we do here at ECU Health,” said Zukowski. “Our goal at ECU Health is to build the national model for high-quality rural academic health care and being good stewards with our resources is a key component of that. I am proud to work alongside mission-driven individuals who commit their time, expertise and energy to serving the people of rural eastern North Carolina.”
Rural hospitals are an essential component of today’s health care environment, dedicated to serving populations that often encounter obstacles to convenient, quality and affordable care. These institutions play a critical role in ensuring healthcare access for underserved communities. The CFOs highlighted on the list are instrumental in ensuring the financial health of their organizations. Applying their expertise in financial planning, these executives help bring cost effective, innovative, up-to-date and accessible healthcare to their communities.
“Andy’s passion for serving others and mission-focused mindset align with ECU Health’s mission to improve the health and well-being of eastern North Carolina,” said Dr. Michael Waldrum, CEO of ECU Health and Dean of the Brody School of Medicine. “As the largest health care provider, employer and medical educator in the region, ECU Health has a unique role to play in the communities we serve – and Andy recognizes that this depends on the organization’s sustainability. ECU Health is proud to help lead the way in creating jobs and encouraging economic growth to help improve the rural communities we serve, many of which experience socioeconomic distress and health disparities.”
Becker’s is delighted to feature these accomplished leaders, who are critical to the successes of their respective organizations. The Becker’s Hospital Review editorial team accepted nominations for this list and curated it to highlight the fantastic accomplishments of rural hospital CFOs.
Greenville, N.C. – ECU Health Medical Center Electrophysiology Lab is the first hospital lab in North Carolina to earn accreditation by the Intersocietal Accreditation Commission (IAC) in Cardiac Electrophysiology in the areas of Testing and Ablation, Device Implantation and Left Atrial Appendage Occlusion. IAC accreditation is a “seal of approval” that patients can rely on as an indicator of consistent quality care and a commitment to continuous improvement.
Accreditation by the IAC means that ECU Health Medical Center Electrophysiology Lab has undergone an intensive application and review process and is found to be in compliance with published standards, thus demonstrating a commitment to quality patient care. Comprised of a detailed self-evaluation followed by a thorough review by a panel of medical experts, the IAC accreditation process enables both the operational and technical components of the facility to be assessed, including representative case studies and their corresponding final reports.

“ECU Health is dedicated to setting a national standard for rural health care and high-quality cardiovascular care,” said Jay Briley, president, ECU Health Medical Center. “Achieving IAC accreditation for the ECU Health Medical Center Electrophysiology Lab not only underscores our commitment to excellence but also highlights the unique advantage of offering advanced care in a rural setting. This milestone reaffirms our mission to enhance the health and well-being of eastern North Carolina by providing the latest technology and medical services close to home.”
Each year, more than one million cardiac device and ablation procedures are performed for the treatment of heart rhythm disorders worldwide. Cardiac electrophysiology procedures are performed by facilities that specialize in the diagnosis and treatment of heart rhythm disorders to relieve symptoms or regulate heart rate and rhythm. Cardiac electrophysiology is comprised of specialized diagnostic testing and therapeutic procedures performed by highly skilled health care professionals. The training and experience of the cardiac electrophysiology specialist performing the procedure, the type of equipment used and the quality assessment metrics each facility is required to measure, all contribute to a positive patient outcome.
“As a cardiologist and electrophysiologist, I know first-hand the importance of having high-quality cardiovascular services close to home for those who live in eastern North Carolina,” said Dr. John Catanzaro, professor and chief, Division of Cardiology, the Brody School of Medicine at East Carolina University, director of East Carolina Heart Institute, ECU Health Medical Center. “This new accreditation underscores our dedication to delivering exceptional patient care through adherence to the highest standards of quality and safety. Patients across eastern North Carolina can take heart knowing the ECU Health Medical Center Electrophysiology Lab has the highest-quality expertise and personnel available to care for them.”
Greenville, N.C. – Michael Waldrum, MD, MSc, MBA, ECU Health chief executive officer and dean of the Brody School of Medicine at East Carolina University, has been named chair-elect of the AAMC (Association of American Medical Colleges) 2024-25 Board of Directors. The incoming board’s term begins Nov. 12, 2024, and will end November 2025, after which Dr. Waldrum will assume the role of board chair.

Dr. Michael Waldrum
Dr. Waldrum was named chief executive officer of ECU Health in 2015 and named dean of Brody in 2021. He previously served as president and CEO of The University of Arizona Health Network and as CEO of the University of Alabama Hospital at Birmingham. Dr. Waldrum is a specialist in critical care medicine and pulmonology and is trained in internal medicine. He received his medical degree from the University of Alabama at Birmingham School of Medicine and completed his residency at the Mayo Clinic in Minnesota.
Dr. Waldrum has served as chair of the AAMC’s Council of Teaching Hospitals and Health Systems (now called the Council of Academic Health System Executives) since 2022, where his unique rural health care perspective helped shape discussions around the complex issues facing rural communities across the nation and how academic medicine can help solve those challenges.
“I am extremely honored to serve as chair-elect of the prestigious AAMC Board of Directors, which has long been a powerful voice in academic medicine,” said Dr. Waldrum. “I look forward to continuing to work closely with highly respected academic health leaders from across the nation who are passionate about ensuring quality health care is available to all, including those living in rural communities. While there are certainly complex challenges facing health care nationally, the AAMC’s collective expertise helps chart new paths forward that improve the lives of many. It is humbling to be a part of this important work.”
The AAMC is a nonprofit association dedicated to improving the health of people everywhere through medical education, health care, medical research, and community collaborations. Its members are all 158 U.S. medical schools accredited by the Liaison Committee on Medical Education; 13 accredited Canadian medical schools; approximately 400 teaching hospitals and health systems, including Department of Veterans Affairs medical centers; and more than 70 academic societies. Through these institutions and organizations, the AAMC leads and serves America’s medical schools and teaching hospitals and the millions of individuals across academic medicine, including more than 193,000 full-time faculty members, 96,000 medical students, 153,000 resident physicians, and 60,000 graduate students and postdoctoral researchers in the biomedical sciences. Following a 2022 merger, the Alliance of Academic Health Centers and the Alliance of Academic Health Centers International broadened the AAMC’s U.S. membership and expanded its reach to international academic health centers.


