NAGS HEAD, N.C. — Jan. 30, 2024 — Outer Banks Health is proud to announce the opening of the Carol S. and Edward D. Cowell, Jr. Cancer Center, a 15,000 square-foot, state-of-the-art facility made possible through the collaboration of Outer Banks Health, ECU Health, Chesapeake Regional Healthcare and the generous support of the Outer Banks community. The center opened its doors to patients on January 29, 2024.
This momentous occasion marks the culmination of years of dedication, perseverance, and community support. Outer Banks Health initiated the endeavor in 2015 with a vision to create a cutting-edge facility that would serve as a beacon of hope and healing for cancer patients on the Outer Banks and the surrounding region.
“The completion of the Cowell Cancer Center was made possible through the unwavering determination of the Outer Banks Health Development Council,” said Ronnie Sloan, FACHE, president of Outer Banks Health. “The council is comprised of dedicated individuals who share a passion for enhancing healthcare in the region and it played a pivotal role in bringing this ambitious project to fruition.”

Led by radiation oncologist, Charles Shelton, the new center boasts a dedicated team, including a director, radiation therapists, a radiation nurse, a genetics extender, a physicist, a dosimetrist, pharmacists and pharmacy technicians, LPNs and RNs, lab technicians, navigators, a social worker, a practice manager, and patient access representatives. While the search for a permanent medical oncologist continues, Dr. Michael Spiritos, formerly of Duke Health, has agreed to serve in that capacity on an interim basis along with Dr. John Barton. Katie Caton, FNP is also on staff as a permanent provider.
Of the 1300 critical access hospitals nationwide, Outer Banks Health Hospital is one of only eight accredited by the Commission on Cancer of the American College of Surgeons and is also distinguished as the only one in the country with an accredited breast program. This notable achievement reflects the commitment of Outer Banks Health to maintaining the highest standards of cancer care.
Outer Banks Health remains focused on expanding its list of services and programs to meet the evolving healthcare needs of the community. The organization’s goals include delivering excellent care locally and collaborating with health organizations throughout North Carolina and Virginia to ensure residents and visitors can access the best possible care.
For more information about the Cowell Cancer Center or to inquire about services, visit OuterBanksHealth.org/services/cancer-care or call (252) 449-7272.
Greenville, NC — Yaolin Zhou, MD, associate professor of Pathology and Laboratory Medicine at the Brody School of Medicine at East Carolina University, director of Quality and Test Utilization, and head of Molecular Pathology at ECU Health, was named to the 2023 Becker’s Hospital Review “Emerging Leaders: Provider Organization Leaders Under 40” list.
The Becker’s Hospital Review list recognizes up-and-coming leaders who are quickly rising through the ranks at their organizations, focusing on development, innovation, and improved outcomes.
The “Emerging Leaders: Provider Organization Leaders Under 40” list honors leaders who are 40 years old or younger for their commitment to optimizing health care. The Becker’s Hospital Review editorial team accepted nominations for this list and curated it to highlight the accomplishments of these rising stars.
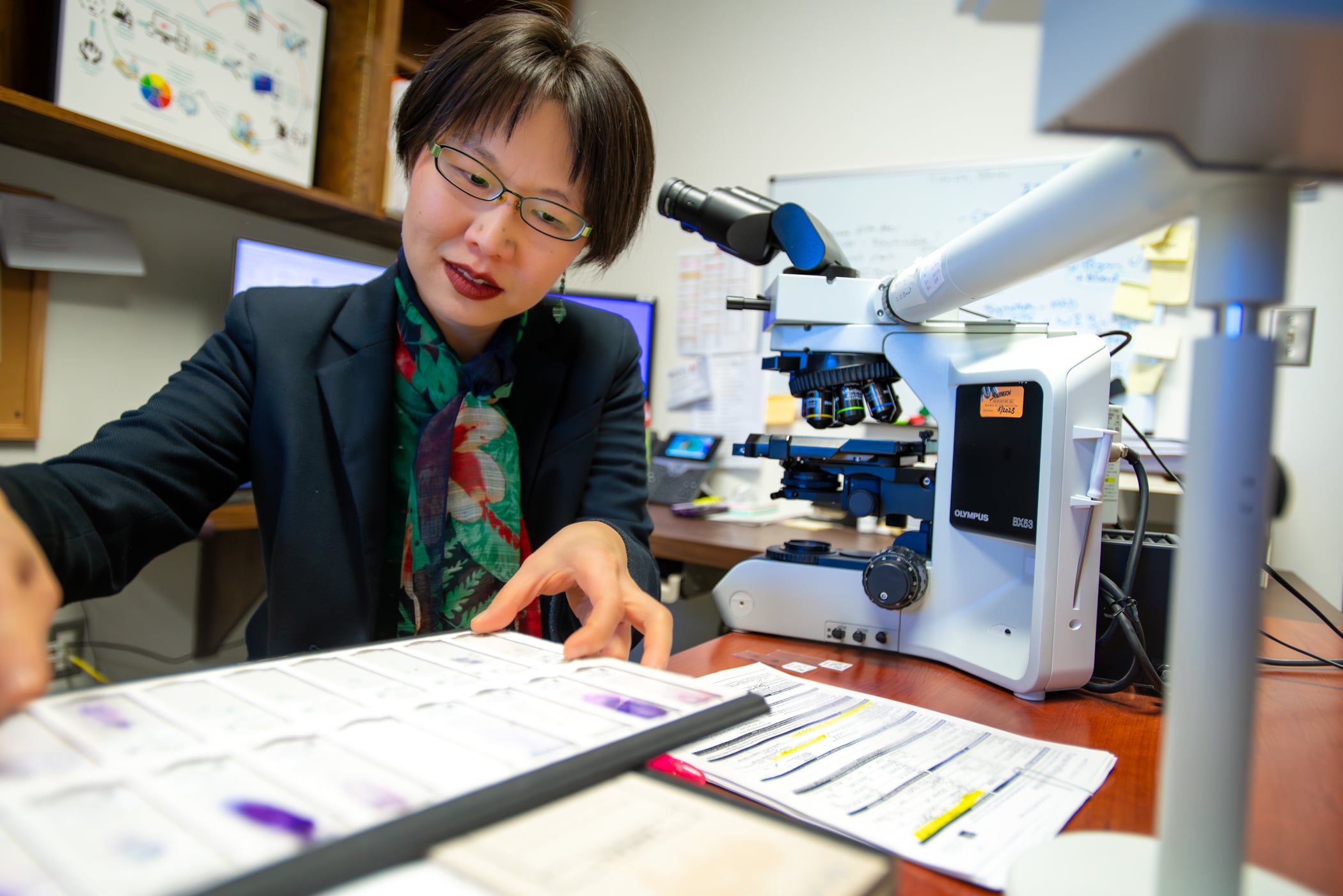
Dr. Zhou trained at some of the most prestigious institutions in the world and chose to come to ECU Health to help address some of the most challenging problems in health care delivery. As the only molecular pathologist in ECU Health’s 29-county service area, she provides expertise that benefits more than 1.4 million individuals in the region.
“ECU Health is proud to have Dr. Zhou, a nationally recognized molecular test utilization expert, whose work exemplifies the vital connection between research, education and effective health care delivery,” said Dr. Michael Waldrum, ECU Health CEO and dean of the Brody School of Medicine. “Dr. Zhou’s expertise shapes innovative clinical solutions, addressing unique barriers in rural populations. I am grateful for leaders like Dr. Zhou who are helping to create a healthier present and future for eastern North Carolina.”
Since her arrival in 2020, Dr. Zhou established an innovative molecular consultation service, focused primarily on pre- and post-testing review, to ensure cancer patients receive appropriate molecular tests and treatment. In 2023, she secured a $250,000 industry-funded quality improvement grant to expand her molecular consultation services across practices in eastern North Carolina’s rural 29-county region. This grant aims to identify and address health care disparities in cancer care, ultimately improving patient outcomes.
In addition to her molecular expertise, Dr. Zhou is an internationally recognized quality improvement and test utilization expert. In 2020, she partnered with clinical colleagues to establish a health system-wide initiative to reduce daily repeat lab tests, achieving a 15 to 25 percent reduction in unnecessary repeat daily testing throughout the system. For this multi-specialty and multi-disciplinary collaboration, Dr. Zhou and her team were honored with the prestigious American Society for Clinical Pathology Choosing Wisely Champion Award.
Dr. Zhou is active as a teaching and clinical faculty member and a bioethics and quality improvement instructor at Brody and for ECU Health. She also represents eastern North Carolina on the board of directors for the Association for Molecular Pathology (AMP), the world’s largest association for molecular professionals. Dr. Zhou recently authored an invited guest editorial in the Journal of Molecular Diagnostics, the official AMP journal. This editorial, based on her grant work, presents a national solution to reduce barriers in precision oncology.
“As a cancer survivor myself, I strive to bring quality and equitable cancer care to those I am honored to serve,” said Dr. Zhou. “All patients deserve high-quality and guideline-recommended cancer treatment. Through this recognition, I hope we can bring greater visibility to how we are addressing disparities in cancer care in our patients. Through collaborative efforts, we can develop solutions for providing equitable cancer care on a broader scale – and it starts here in eastern North Carolina.”
NAGS HEAD — About a decade ago, the Outer Banks community suffered higher cancer mortality rates than the state and nation. Not only has that trend reversed, but now for the first time, local cancer patients can receive all their services under one roof.
Over 275 people attended the ribbon-cutting and open house on Jan. 24 for the Carol S. and Edward D. Cowell, Jr. Cancer Center. Located at 4927 S. Croatan Highway in Nags Head, it opens its doors to patients on Jan. 29.
“In 2012, Outer Banks Health didn’t have a cancer services program at all, and we were trailing the state and we were trailing the nation when it came to cancer mortality for all cancers…and we wanted to change that dynamic,” Ronnie Sloan, president of Outer Banks Health, said during brief event remarks.

The Outer Banks’ cancer mortality rate was about 6% and 7% higher than the nation and the state, respectively, Sloan said in an interview at the event.
Now, local cancer mortality rates are 6-7% lower than the state and country. The 5-year mortality for breast cancer rate dropped 50% in recent years. Even as cancer mortality rates have steadily declined across the country, “we’ve outpaced that,” Sloan said.
Carol Cowell cut the ribbon at Wednesday’s event. She made the namesake donation to the Carol S. and Edward D. Cowell, Jr. Cancer Center in Nags Head in honor of her late husband and in appreciation of the local community.
Originally from Brooklyn, New York, Cowell said in an interview that she is a cancer survivor who received treatment in Elizabeth City in 2005. The Outer Banks didn’t offer cancer services then, but she was greatly impressed by “the community sense that you got” from local health care professionals and from the community at large.
Fundraising for the center was similarly a community effort.
“This has been just an amazing journey,” Tess Judge said during her event remarks. Judge is chair of the board of directors for Outer Banks Health and co-chaired the fundraising team with Cindy Thornsvard.
Judge said she lost her mother and a son-in-law to cancer, and her daughter-in-law is struggling with it now, “so cancer services and the wonderful team we have here is just so special not only to me but to many.”
Fundraising for the center began during COVID, and their original goal of $4 million was bumped up to $6 million as the costs of building supplies soared.
According to Sloan, nearly $6.5 million has been raised for the center.
“We did that because of all of you, and the tremendous support this community has given to this cancer center,” Judge said.
Stephanie Anderson, a community member who had lost people to cancer, hiked the entire Appalachian Trail last year and raised about $10,000 for the center in the process, said Jennifer Schwartzenberg, director of community outreach and development for Outer Banks Health.
The journey to the center
Outer Banks Health hired its first director of cancer services in 2012, said Sloan, who came aboard in mid-2011.
“In 2013, the board of trustees made a fantastic decision,” Sloan said during his public remarks. They chose to purchase the radiation therapy center that was closing about two miles north of the hospital.
“We didn’t want our community to have to drive two hours each way” for treatment, he said.
Dr. Charles Shelton, a radiation oncologist, began working at Outer Banks Health — then called The Outer Banks Hospital — in 2014, and he leads the cancer services team, Wendy Kelly, marketing director for Outer Banks Health, said in an email.
Shelton set a goal of creating and maintaining an accredited cancer program to reduce the high cancer mortality rate among residents of Dare and Currituck counties, Kelly said.
“It’s been a dream of this organization since 2015 to build a facility that would allow patients to receive the highest-quality, compassionate cancer care all under one roof right here on the Outer Banks,” Kelly said.
Supported by its two partners, ECU Health and Chesapeake Regional Healthcare, along with the generosity of the local community, “that dream is now a reality,” she said.
In 2016, the Commission on Cancer of The American College of Surgeons granted a “Three-Year Accreditation with a Commendation” to The Outer Banks Hospital, which the facility has “proudly maintained” since that time, according to Kelly.
“Additionally, we are one of only eight critical access hospitals in the nation with this accreditation, and the only one nationally to have an accredited breast care program,” she added.
Outer Banks Health is one of 20 critical access hospitals in North Carolina, which have 25 beds or fewer and receive cost-based reimbursement, according to the North Carolina Division of Health and Human Services website.
“Outer Banks Health is an approved Medicare and Medicaid provider and participates with most commercial insurance companies,” Kelly said.
Sloan said that the new “comprehensive center” allows them to offer the “best care possible.”
The entire cancer team can quickly make decisions about patients in consult with one another as “concerns pop up,” and having the dedicated center eliminates the need for patients to go from the first to second floor of the hospital for care, then across the busy bypass for radiation treatment, he said.
Kelly expressed gratitude for all the community support of the center, which included the over 275 people who attended the event on Wednesday.
In addition to Shelton, the cancer services team also includes a director, three radiation therapists, a radiation nurse, a genetics extender, a physicist, a dosimetrist, a licensed practical nurse, 11 registered nurses, a nurse navigator, a financial navigator, a lay navigator, a social worker, a practice manager and three front desk monitors, according to Kelly.
“Our search continues for a permanent medical oncologist, and in the interim Dr. Michael Spiritos, formerly of Duke Health, has agreed to serve in that capacity,” Kelly said in her email. “Additionally, Dr. John Barton serves as a medical oncologist at the center.”
“Congratulations Outer Banks Health on this much-needed and impressive expansion,” Robert DeFazio, chairman of the board of directors for the Outer Banks Chamber of Commerce, said during his event remarks.
Greenville, N.C. – Four ECU Health Physicians clinics have been recognized by the American Heart Association and American Medical Association for its commitment to improving blood pressure (BP) control rates, earning Gold-level recognition as part of Target: BP. The Gold award recognizes practices in which high blood pressure is controlled in 70% or more of the adult patients affected.
“Managing and controlling your blood pressure is essential for preventing the development of heart disease and stroke, which continue to be leading causes of death for adults in our country,” said Dr. Jason Foltz, chief medical officer, ECU Health Physicians. “High blood pressure is a leading risk factor of heart disease and stroke that can often be prevented or managed if diagnosed and treated properly. Our region experiences high rates of diabetes, stroke and heart disease, and the Target: BP program allows ECU Health to better help patients lower their blood pressure by putting proven knowledge and guidelines to work on a daily basis.”

ECU Health Physicians clinics achieving Gold Status in Target: BP for 2023 include:
- Firetower Medical Office – 1204 E. Fire Tower Road, Greenville
- Family Medicine Center Purple and Gold Modules – 101 Heart Drive, Greenville
- General Internal Medicine – 521 Moye Medical Center, Greenville
According to the American Heart Association, high blood pressure, or hypertension, is a leading risk factor for heart attacks, strokes and preventable death in the U.S. There are 121.5 million adults in the country living with hypertension – that is nearly half of all adults in the U.S. Unfortunately, less than half of them have their blood pressure under control, making both diagnosis and effective management critical. Heart disease is the leading cause of death both nationally and in the state. Meanwhile, stroke is the fifth leading cause of death in the U.S., yet is the fourth leading cause of death in North Carolina.
Target: BP is a national initiative formed by the American Heart Association and American Medical Association in response to the high prevalence of uncontrolled blood pressure. The initiative aims to help health care organizations and care teams, at no cost, improve blood pressure control rates through an evidence-based quality improvement program and recognizes organizations that are committed to improving blood pressure control.
“By committing to helping more people in eastern North Carolina control their blood pressure and reduce their risks for future heart disease and stroke, ECU Health is taking a key step to helping more people live longer, healthier lives,” said Yvonne Commodore-Mensah, PhD, MHS, RN, FAHA, Target: BP advisory group volunteer and associate professor at Johns Hopkins School of Nursing. “ECU Health’s participation in the Target: BP initiative shows its dedication to turning clinical guidelines into lifelines for patients and their families.”
In honor of Dr. Martin Luther King Jr. Day, community leaders, elected officials and eastern North Carolina residents came together for the 27th annual Community Unity Breakfast, hosted by the Greenville-Pitt County Chamber of Commerce on Monday.
The event brings together the community to reflect upon the life and legacy of Dr. Martin Luther King Jr. while celebrating and expanding diversity initiatives in Greenville and Pitt County.
As a sponsor of the event, ECU Health had an opportunity to present a speaker during the event. Brian Floyd, chief operating officer of ECU Health and president of ECU Health Medical Center, represented the system and shared a few words.
Floyd said that events like this are closely aligned with ECU Health’s mission to improve the health and well-being of eastern North Carolina because it focuses on bringing everyone together and supporting those around you.

“Your well-being is attached to much more than your clinical and scientific makeup,” Floyd said. “You can’t be well if you’re socially isolated. You can’t be well if you don’t have the means to support yourself and your family. You really can’t be well if you have no way to help those around you. So our mission, as complicated as it is, is to make people and communities better. This community comes alongside us and helps us do that as well. We all can participate in what others are doing to improve our society, to improve how people come together, and work together to love and support each other.”
Floyd also highlighted his appreciation for ECU Health’s close collaboration with the Brody School of Medicine at East Carolina University, and the relationships with other colleges, universities and high schools. He said the opportunity to develop and grow talent within the system is something he is proud of as well.
All of this leads to a great financial impact on the region, Floyd said, and that can go a long way to effect positive change in the lives of residents in the East.
“We know that education is important to the fabric of society and the wellness of people and the socioeconomic conditions of eastern North Carolina require us to do something about that,” Floyd said. “We’re fortunate that we can stimulate the economy of eastern North Carolina by more than $4 billion per year. That’s not just money – it’s hope, it’s a way to get started, it’s a way to support your family. When you put all of that together, the pillars of what we’re doing for eastern North Carolina, that’s the difference we can make.”
Pastor Eve C. Rogers, senior pastor at New Dimensions Community Church, gave the keynote address for the event. Chad Tucker, director of Volunteer Services at ECU Health Medical Center, serves as co-chair of the Community Unity Planning Committee and introduced Pastor Rogers during the event.
Pastor Rogers spoke on the importance of standing up to injustices in our communities to help create a future everyone can be proud of. She said showing up for the marginalized members of our communities is a responsibility we all carry.
“As we run and purse this race of life, liberty and the pursuit of happiness, I provoke you to show up with soul-force,” Pastor Rogers said. “Exercise and put into plan the opportunity that God gives you, day after day, season after season, time after time again, to show up and do what is right, fair and equitable.”


Greenville, N.C. – East Carolina University and ECU Health are launching an initiative to increase the number of adult gerontology acute care nurse practitioners serving as advanced practice health care professionals in ECU Health’s critical care settings. This effort builds on the collective commitment of both organization to solve the rural health challenges in the region as well as the state.
The effort – conceived by nursing and education leaders from ECU’s College of Nursing and ECU Health – will benefit both the university and the health system, said Dr. Bim Akintade, the dean of ECU’s College of Nursing. An investment of nearly $1.5 million over five years from ECU Health will increase the College of Nursing’s capacity to graduate trained and qualified nurses who can meet the growing need for acute care practitioners to treat the hospital’s sickest patients.

“ECU Health is proud of its close relationship with ECU and the College of Nursing, particularly as it pertains to our efforts to adapt to the national health care workforce shortage,” said Dr. Daphne Brewington, ECU Health’s vice president of nursing. “Our success as an academic health system is predicated on our ability to leverage clinical and academic excellence in order to ensure we can provide high quality health care for the residents of eastern North Carolina.”
Nationally, the aging population is growing, accompanied by the shortage of health care workers. This collaboration not only strengthens the health care workforce in eastern North Carolina but also contributes to improved health outcomes and increased accessibility to specialized care for older adults in the communities of eastern North Carolina.
Through this effort, ECU Health is helping fund the development of a new Adult Gerontology Acute Care Nurse Practitioner Post Graduate Certificate, which will train current nurse practitioners to treat acute care adult patients. The investment also provides funding for a program director who teaches and an additional part-time faculty member as well as administrative support and operational costs.
The program will reserve six enrollments per enrollment cycle for current ECU Health employees, highlighting the importance of providing specialized training that benefits the region.
“Our plan is to take the next few months to work with our partners at ECU Health and find clinical placement sites in critical care environments for ECU Health employees who enroll in the program,” Akintade said. “They need nurses, and training nurses is our business and passion. This collaboration is a win-win and makes complete sense for the University, the Heath System, the region, and the state.
Clinical placements for students employed by ECU Health will take place at ECU Health facilities, which will help to alleviate a major sticking point for training advance practice nurses – finding clinical placements for students in training. It also has the potential to create pathways for those in the program to experience acute care at both ECU Health Medical Center and in ECU Health’s regional community hospitals.
The initiative isn’t limited to the current arrangement and both ECU and ECU Health continue to explore ways to leverage this effort to design innovative solutions that benefit the people of eastern North Carolina.
“Eastern North Carolina depends on institutions like ECU Health and ECU to collaborate on innovative solutions that drive us towards our mission of improving the health and well-being of the region,” said Dr. Trish Baise, ECU Health’s chief nursing executive. “As a health system serving 1.4 million people, we need more nurses at every level in order to meet the region’s immense needs. The College of Nursing is one of the premiere nursing education schools in the nation and our health system is great training ground for developing a health care workforce with a focus on rural health challenges. I am excited to see the benefit this program will have on our patients and team members.”
“I was just doing what is right.”
Sheila Grady, Community Liaison with ECU Health’s Home Health and Hospice, has never been one to seek the limelight in her 29-year career. In fact, she’d rather be behind the scenes, helping people and making a difference.
“She has a heart of gold, and she’s going to do whatever it takes to assist and serve our patients and families,” said Sarah Taylor, Sheila’s supervisor and the manager of marketing and hospice volunteer coordinator. “She understands we are a business, but we’re in a people-serving business and that’s our number one goal.”
When Aaron Hair contacted Sheila about having two memory bears made after the death of his father, her drive to do what’s right while serving patients and their families got people’s attention.
“My dad was diagnosed with cancer two years ago,” explained Aaron. “When the decision was made that he would stop treatment, he was admitted to palliative care at the Medical Center, but his doctor and nurses recommended the hospice house in Greenville.”
While his father was in the hospice house for less than 24 hours before passing away, Aaron recognized the hospice team members made a difficult situation easier to bear.
“They made us feel at ease and explained everything,” Aaron said. “From the facility to the staff, they were all top notch.”
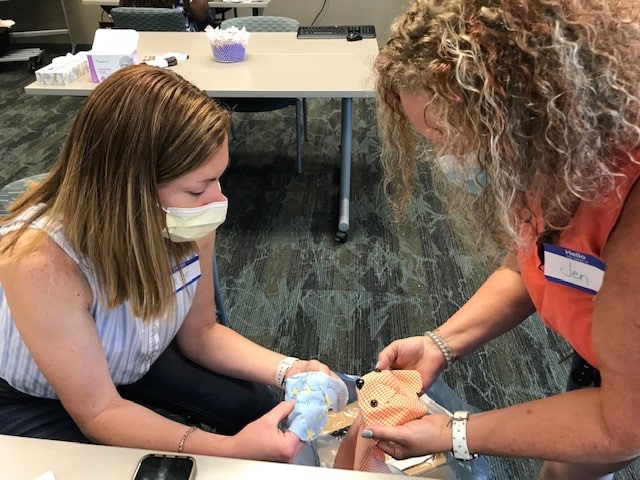
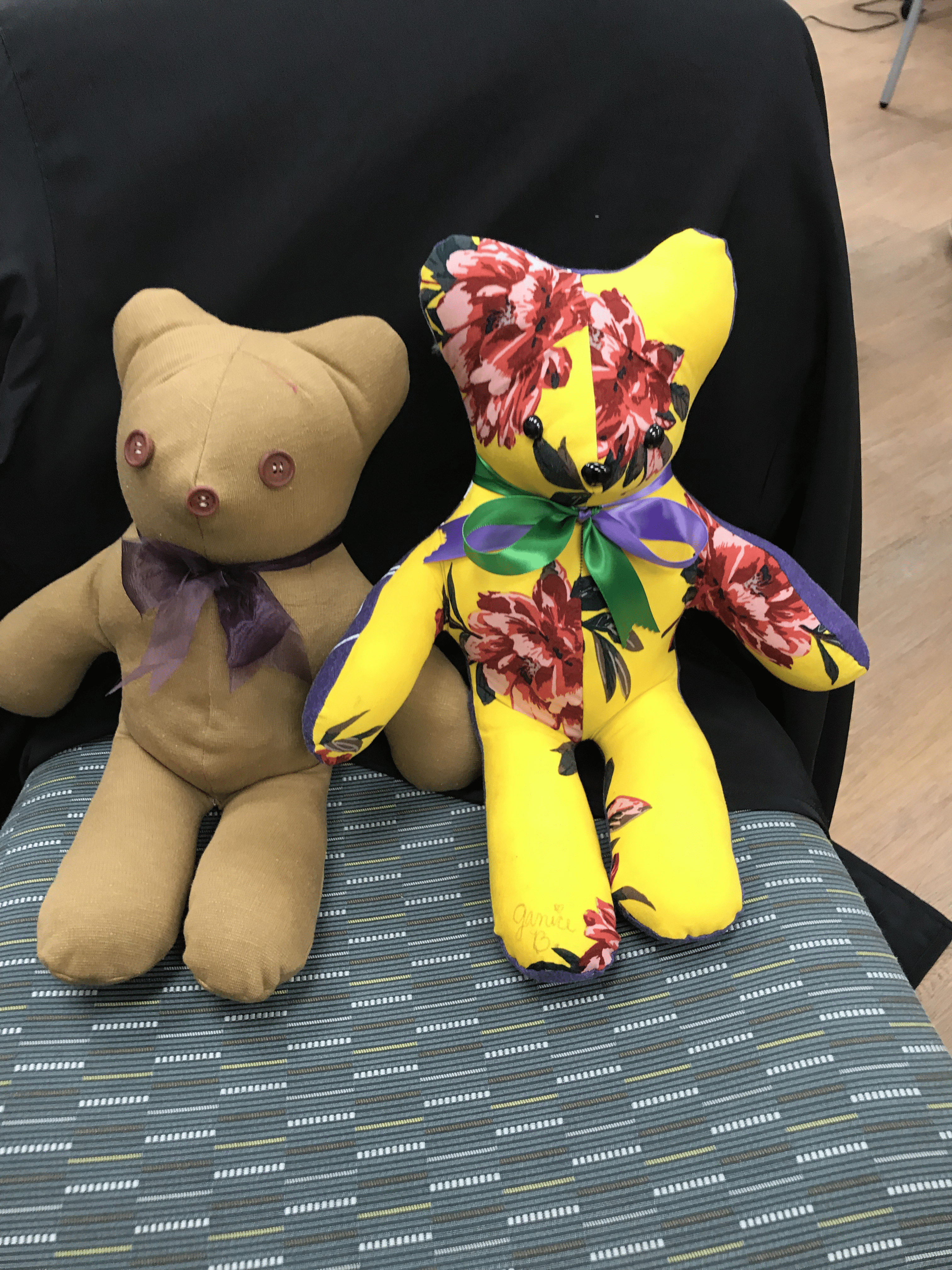
After his father’s death, Aaron and his family wanted to make use of the Memory Bear program, a service of ECU Health’s Home Health and Hospice team that makes teddy bears or pillows using an article of clothing from the family member who passed away. Sheila has run the program for the past two years.
Sarah noted that it was Sheila’s leadership that made the Memory Bear program what it is today.
“Now we have workshops in Greenville and Kenansville, and we’re serving all hospice patients on our service. And there’s a lot of love put into these bears,” Taylor said.
The work, Sheila emphasized, is done entirely by volunteers.
“These are nurses who pick up materials and drop off bears after their shifts,” Grady said. “Some are retired from health care, and some are retired teachers. They come from all walks of life, and they don’t ask for a dime.”
Aaron contacted Sheila directly to request two memory bears, one for each of his daughters. The challenge, however, became how to get his dad’s shirts to the seamstresses.
“I live in Johnston County but was working in Havelock. It would have been challenging to get the shirts to Greenville,” Aaron explained. As they talked, Sheila learned that his commute took him right by her office in Duplin County. “She gave me her personal cell phone number, and I called her when I was on the way so we could plan a meet-up. She didn’t have to do that.”
As for Sheila, it was just an example of her drive to do the right thing.
“He was a young man who lost his father,” she said. “He was an only child, and he was asking for something for his family.”
Once she got the shirts, Sheila realized that Aaron had only asked for bears for his daughters, but nothing for his mother.
“She called me and said, ‘You didn’t mention making anything for your mom,’” Aaron said. “But I only asked for two bears because that’s the limit set on the brochure, and I wasn’t going to ask for more than that.”
Sheila, however, emphasized that the two-bear limit is a flexible parameter. ”We listen to the person’s story and we make what is right for each person. I knew we needed to make a pillow for his mom.”
A few days later, the seamstress working on the project contacted Sheila with another observation.
“She said, ‘This man didn’t ask for a thing for himself,’ and she told me they had enough material to make a pillow for Aaron, as well,” she said. “So that’s what they did.”
When it came time to deliver the items, Sheila again went out of her way to ensure they were delivered prior to a planned trip out of town. When she brought the items out, Aaron learned that not only had the bears and pillow for his daughters and mom been created, but that a pillow had been made for him as well — made from the shirt his dad wore the last time the two of them went fishing together.
“I hadn’t thought about myself,” Aaron admitted. “It was heartwarming for someone to think about that.”
Sheila confirmed that it was common for family members not to think of requesting a pillow or bear for themselves, even when it’s someone familiar with the program.
“One of the nurses who hired me for this job – her husband died suddenly. I reached out to her and told her, ‘I want to make a bear for you,’ and the nurse said she had never even thought about it. We made her a bear, and later she sent us a picture of her in bed with the bear made from her husband’s pajamas,” Grady said. “Below the picture she wrote, ‘I still have him with me.’ That’s what the Memory Bear program is all about.”
After his meeting with Sheila, Aaron knew what he wanted to do.
“When I left the parking lot that day, I went home and called my brother-in-law, who works for ECU Health, to get Mrs. Grady’s supervisor’s name so I could let them know what she had done,” Aaron said. “Mrs. Grady is a loving and caring lady who I feel I have known my whole life.” He ended up writing an email that garnered a lot of attention.
“I had no idea he would write that email,” Sheila said. “I don’t do this for the recognition.” She was recognized, however, at a surprise gathering in her Kenansville office on Oct. 9. “I was shocked, and it’s difficult to surprise me,” Sheila laughed. “When I saw my husband and family in my office that day, I knew something was up.”
However, she is quick to pass credit to others.
“The team makes this happen,” Sheila said. “The nurses, PTs, aides, OTs and social workers. The chaplains. The seamstresses who make the bears. They’re the real heroes.”
That her home office in Kenansville has won multiple Patient Choice Awards this year bears that statement to be true.
Sheila also emphasized that the ECU Health hospice service, which is made unique by the Memory Bear program, is deeply important.
“I wasn’t sure I’d like the hospice setting when I was first hired,” she admitted. “But I want to make a difference in people’s lives, and that’s what we do. Now I educate people about our home health and hospice services and assist with referrals, and I love it because I know I am making a difference.”
Her supervisor, Sarah, agreed: “We can walk the journey with these patients and their families, and Sheila is the type of person who is going to make sure the family is OK and she can bring them some peace.” Sarah also noted that the Memory Bear program has gained a positive reputation in the community: “Now we have people say, ‘Oh, you’re the hospice with the memory bears?’ and that’s awesome.”
Sheila has plans to retire in mid-November, although she’s not retiring from the Memory Bear program just yet.
“I have another grandchild on the way, so I’ll be spending time with my family, but I come from a long line of people who believe work is a good thing,” Grady said. “I’ll volunteer with the Memory Bear program for sure.”
Greenville, N.C. – The Greenville Traffic Safety Task Force was awarded the Peter K. O’Rourke Special Achievement Award at the Governor’s Highway Safety Conference in New York City, which recognizes notable achievements in the field of highway safety by individuals, coalitions, organizations, nonprofit groups, businesses, media, government agencies, universities or programs. The task force was created in partnership by Greenville Police Department and ECU Health Medical Center’s Eastern Carolina Injury Prevention Program (ECIPP).
“We are honored to receive an achievement award that recognizes the efforts of the Greenville Traffic Safety Task Force to improve pedestrian and driver safety,” said Ellen Walston, Injury Prevention Program Coordinator, ECIPP. “The Greenville Traffic Safety Task Force has served as a model of success across the state and is successful because of our community partners who want to see Greenville become safer for drivers and pedestrians. Receiving this award is not just a recognition of our efforts, it’s a testament to our proven results of unwavering commitment to making our roads safer for all.”

The Greenville Traffic Safety Task Force was honored for bringing together a range of community stakeholders and leaders to quickly implement needed roadway safety countermeasures. For many years Greenville was ranked number one for highest volume of crashes in cities with populations of 10,000 or more by the North Carolina Department of Motor Vehicles. With an average of over 400 crashes per month in a city of less than 100,000, leaders in the community sought a creative solution. Thus, Greenville Police Department and ECIPP at ECU Health Medical Center formed the Greenville Traffic Safety Task Force.
The Greenville Traffic Safety Task Force is now comprised of partners from ECIPP, Greenville Police Department, City of Greenville’s Engineering Department, ECU Health Police, ECU Police, North Carolina Department of Transportation and Greenville Metropolitan Planning Organization. Partners are responsible for enforcement data, bicycle and pedestrian safety, crash reduction and roadway changes, school safety and policy changes. Each partner has a stake in the task force’s success.
“The Greenville Police Department is honored to work with this task force and take part in receiving this achievement,” said Deputy Chief Chris Ivey, Greenville Police Department. “The efforts of the Greenville Traffic Safety Task Force are key in ensuring traffic safety of our community and encouraging good driving habits. We see the value in traffic safety and recognize that enforcement and collaboration with our partners on the task force can save lives.”
The multidisciplinary group identified and implemented solutions including high-visibility crosswalks, traffic delineators and increased enforcement in crash-prone areas. Together, these countermeasures and community support led to a sizable reduction in crashes, providing a model for other cities and communities. The Greenville Traffic Safety Task Force also installed bollards, or vertical posts, which are used to guide left turns from middle lanes at busy areas. In 2021, Greenville moved from the number one ranking for crashes in the state to the number seven slot. In 2022, Greenville has moved to the number eight slot.
“Traffic safety takes effort from a number of different partners,” said Stacey Pigford, Civil Engineer II, City of Greenville. “Our department is proud to work with the Greenville Traffic Safety Task Force on a cause that has produced such positive results, and to see those results recognized.”
The task force was previously awarded the 2019 North Carolina Governor’s Highway Safety Program Community Collaboration Award, the Safe States Injury and Violence Prevention Achievement Award in 2022 and the 2023 inaugural North Carolina Vision Zero Safety Award.

Dr. Michael Waldrum
For those of us fortunate enough to be involved in rural health care, the third Thursday of November is a special time to pause, reflect and look forward. Designated as National Rural Health Day in 2011, this particular Thursday has served as an important moment to honor the contributions of rural health care workers, including the 14,000-plus ECU Health and Brody School of Medicine at East Carolina University team members who care for eastern North Carolina.
You don’t have to look far to see the impact of rural health care. All around us are doctors, nurses, allied health professionals, professors, students and others who make high-quality health care possible here in eastern North Carolina. Today is a day to celebrate them and their tireless dedication to serving a region of 1.4 million people.
ECU Health’s vision to become the national model for rural academic health care is necessitated by the shared challenges rural communities across America face. An estimated 62 million people call rural America home, and they all experience health care in similar ways: fewer resources, higher burdens of diseases like diabetes and heart disease, difficulty accessing care and a higher number of under and uninsured people when compared to urban communities. Eastern North Carolina is no different.
These are undoubtedly complex challenges, but they can be solved through innovation and ingenuity. For example, the American Association of Medical Colleges estimates a shortage of more than 124,000 physicians by 2034, a reality that will disproportionately impact rural communities. We can anticipate the impending shortage, understand the disproportionate impact it will have on our communities and utilize the unique resources available at our academic health system to address these challenges.
Studies show that family medicine residents who spent 50% or more of their training time in rural settings were at least five times more likely than residents with no rural training to practice in a rural setting. Brody and ECU Health together launched the Rural Family Medicine Residency program in 2021, and the results are immediately evident with multiple residents already committed to continue practicing in one of ECU Health’s rural family medicine clinics.
There are countless other examples like the Rural Family Medicine Residency program that showcase the value of an academic and health care delivery system. When we created ECU Health, the vision was to create a premier academic health care enterprise that could serve as a national model for other rural health systems to learn from. We are on our way to realizing that vision, and I am proud of our work so far. Our progress would not be possible without the incredible team members who have dedicated their careers to improving the lives of others.
I encourage our community members to thank a health care worker this week. Our lives are better because they choose to serve here in rural eastern North Carolina.
Resources
Rural Family Medicine Residency Program
Rural Family Medicine Residency Program takes unique approach to training physicians
Dr. Audy Whitman is an eastern North Carolinian, through and through. He was born in the farming town of Seven Springs – a town of roughly 80 people – in Wayne County.
Like in many towns in eastern North Carolina, its citizens struggle with poverty and access to health care. It is there, in Seven Springs, where Dr. Whitman’s rural upbringing helped him discover a love for medicine that influences his work today.
Today, Dr. Whitman is a family medicine physician for ECU Health and clinical assistant professor at the Brody School of Medicine at East Carolina University, but back in Seven Springs, he was a helping hand in the tobacco fields, braving the eastern North Carolina heat and humidity.
“There is no more powerful motivator in the universe, in my humble opinion, than standing in the middle of a tobacco field in the late summer with 99 percent humidity, no shade and it’s 100 degrees outside,” Dr. Whitman said. “Your hands are caked with tobacco gum. The nicotine is soaking through your skin, so you feel nauseous all the time. Those long days taught me a great work ethic but they were also powerful motivators.”
Rural health care realities
Americans who live in rural areas make up 20% of the United States population and residents in these areas face a myriad of challenges: shorter life expectancy, higher mortality, higher rates of poverty, fewer local doctors and greater distances to travel to see health care providers. Only 10% of U.S. physicians currently practice in rural areas.
Physician shortages are no secret across the country, with the Association of American Medical Colleges estimating a shortage of up to 124,000 physicians by 2034, and rural areas are at an even greater risk.
The Brody School of Medicine was founded over 40 years ago to train primary care physicians to provide care for rural eastern North Carolina. These challenges inform the medical school’s mission and its proven track record is best represented by the fact that Brody is No. 1 in North Carolina and No. 2 in the United States in the percent of graduates in the last decade who chose careers in family medicine.
Programs like the Rural Family Medicine Residency Program take that work a step further by focusing on initiatives that help place providers in rural areas. Studies show that family medicine residents who spent 50% or more of their training time in rural settings were at least five times more likely than residents with no rural training to practice in a rural setting.

“Rural health care is under duress, and our rural communities need solutions,” said Dr. Michael Waldrum, ECU Health CEO and dean of the Brody School of Medicine. “The Rural Family Medicine Residency Program is another great example of ECU Health and Brody understanding what the community needs are and creating new pathways to educate physicians to meet the community’s needs and improve the health and well-being of those communities.”
Setting a path forward
After Dr. Whitman was approached to create and administer the program, things moved quickly. A “national guru for all things family medicine” made a visit to eastern North Carolina to consider the best locations for residents to begin their rural training. Dr. Whitman and team reached out to other universities and health systems with established programs and traveled to learn about rural organization structure and rural curriculum best practices. Two years later, the Rural Family Medicine Residency Program had its first cohort ready for training.
The first year of the program features training at ECU Health Medical Center, a Level I Trauma Center, and helps set the residents up for success when they get to the rural environments in their second year.
“Anything and everything you can imagine seeing in residency training, you’re going to see at the medical center,” Dr. Whitman said. “We provide this very intense, inpatient-heavy first-year experience for these rural residents where they get to see really sick, really complicated patients with lots of resources at their disposal so they can learn how to take care of these really complicated patients. After their first year of training, when they’ve taken all of these lessons learned, they can go out into these rural communities and apply those lessons learned where they’re the only show in town.”
Dr. Whitman added that while Greenville and eastern North Carolina are rural, the more than 1.4 million patients served through the ECU Health system creates a high volume of patients at ECU Health Medical Center, and the exposure to so many patients during their training is also hugely beneficial for the rural residents.
“An institution like ECU Health boasts a 974 bed, Level I academic medical center where residents train alongside some of the best and brightest health care minds in the state,” said Dr. Jason Higginson, executive dean at Brody. “Medical residents can then serve in our more rural hospitals to apply that knowledge to underserved populations, building a connection to the community in which they serve and making a real difference in the lives of patients.”

Dr. Zeel Shah
Drs. Zeel Shah and Jim Jaralene Porquez are part of the inaugural cohort for rural family medicine residents. Dr. Shah practices and trains at Roanoke-Chowan Community Health Center in Ahoskie and Dr. Porquez at Goshen Medical Center in Beulaville, both of which are Federally Qualified Health Centers (FQHC) that serve at-risk and underserved rural populations. The mission and vision of these FQHC organizations align with the mission and vision of ECU Health. Together, they seek to augment scarce health care resources in rural communities, improve the health metrics of the communities they serve, and encourage the residents that train in these rural communities to establish roots and continue serving these rural communities after graduation from their residency training program.
Dr. Shah said the year in Greenville was a great experience before continuing her residency training with a focus on serving the rural community of Ahoskie.
“In Greenville you have a lot of resources, but it’s a learning curve to rotate through the different specialties,” Dr. Shah said. “In Ahoskie, the challenges are different. Social determinants of health care, such as finances and distance, play a significant role, and you don’t have the same resources. You learn quite a lot about how to make your limited resources go a long way by relying on creative strategies while using medical expertise you picked up in Greenville.”
Now, as third year residents, Drs. Shah and Porquez feel established in their respective communities and have built trusting relationships with patients, families and fellow team members. Both said the community aspect and truly knowing their patients are among the most rewarding parts of their rural experience. For Dr. Porquez, feeling love, trust and appreciation from her patients has made her time in Duplin County special and a place that she plans to call home after her residency.
“What really drew me into my community clinic in Duplin County specifically, is that my patients are very appreciative of what I do for them,” Dr. Porquez said. “They care so much about my time, my effort and my expertise, and I think in just a couple of years I have built that strong trust and relationship with them. I feel like I don’t just treat them with their disease, but I go further than that. I treat them as a whole, and I get to know their whole well-being. I see them as a whole person and not just the disease that I treat.”
Early milestones

Dr. Jim Jaralene Porquez
For Drs. Shah and Porquez, the personal connections built through the program are so strong that both have decided to practice in eastern North Carolina following the completion of the program in 2024. Their graduation, along with the other residents in the first cohort, will represent a significant milestone in the program’s short history and help ensure rural communities have access to specially trained, high-quality rural family medicine providers.
Dr. Whitman said he’s proud to see two members of the first cohort choose to stay and make a difference in communities like the one in which he was raised. The successful launch has the team thinking bigger for the program, and recruitment for the next cohort, featuring a new site and more residents, is underway. The Roanoke Rapids area will benefit from the program and begin seeing its first residents from the program in 2024, and the program in general will grow from its current size of 10 residents to a total of 27 residents over the next three years.
“Moving forward, I see nothing but growth for us,” Dr. Whitman said. “We are truly doing mission-driven work and trying to bridge the chasm of health care disparities of urban centers and rural areas here in North Carolina.”
Dr. Waldrum agreed and said he sees the program as the beginning of something special for eastern North Carolina and rural medicine.
“My hope is that we can take the knowledge gained through the Rural Family Medicine Residency Program and apply those lessons towards other specialized clinical areas of expertise in the near future,” Dr. Waldrum said. “We are proving that we can be highly successful in creating rural residency tracks and our historic success training rural providers who go on to practice here in North Carolina is a further testament of our ability to create unique solutions that meet the needs of those we serve.”
