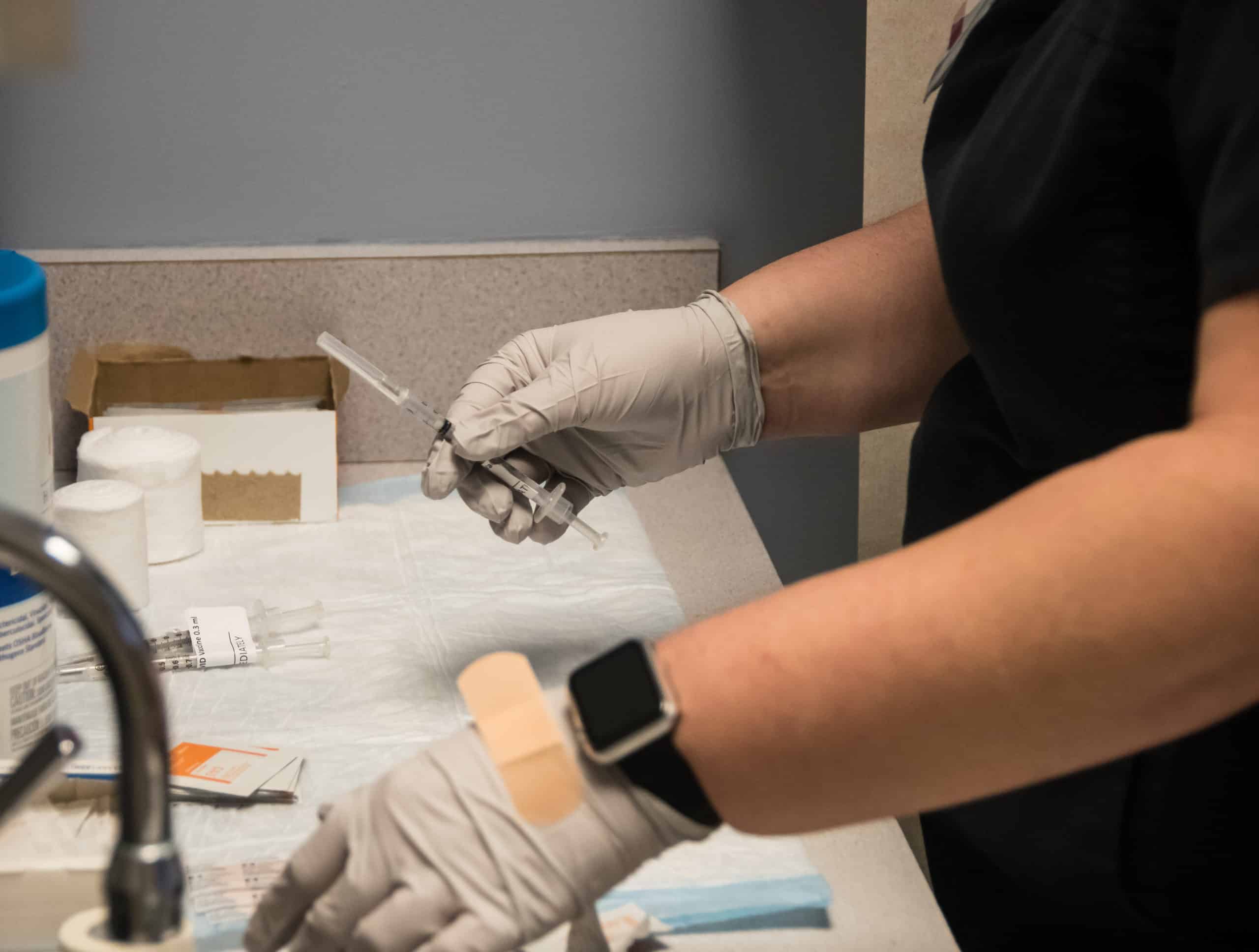
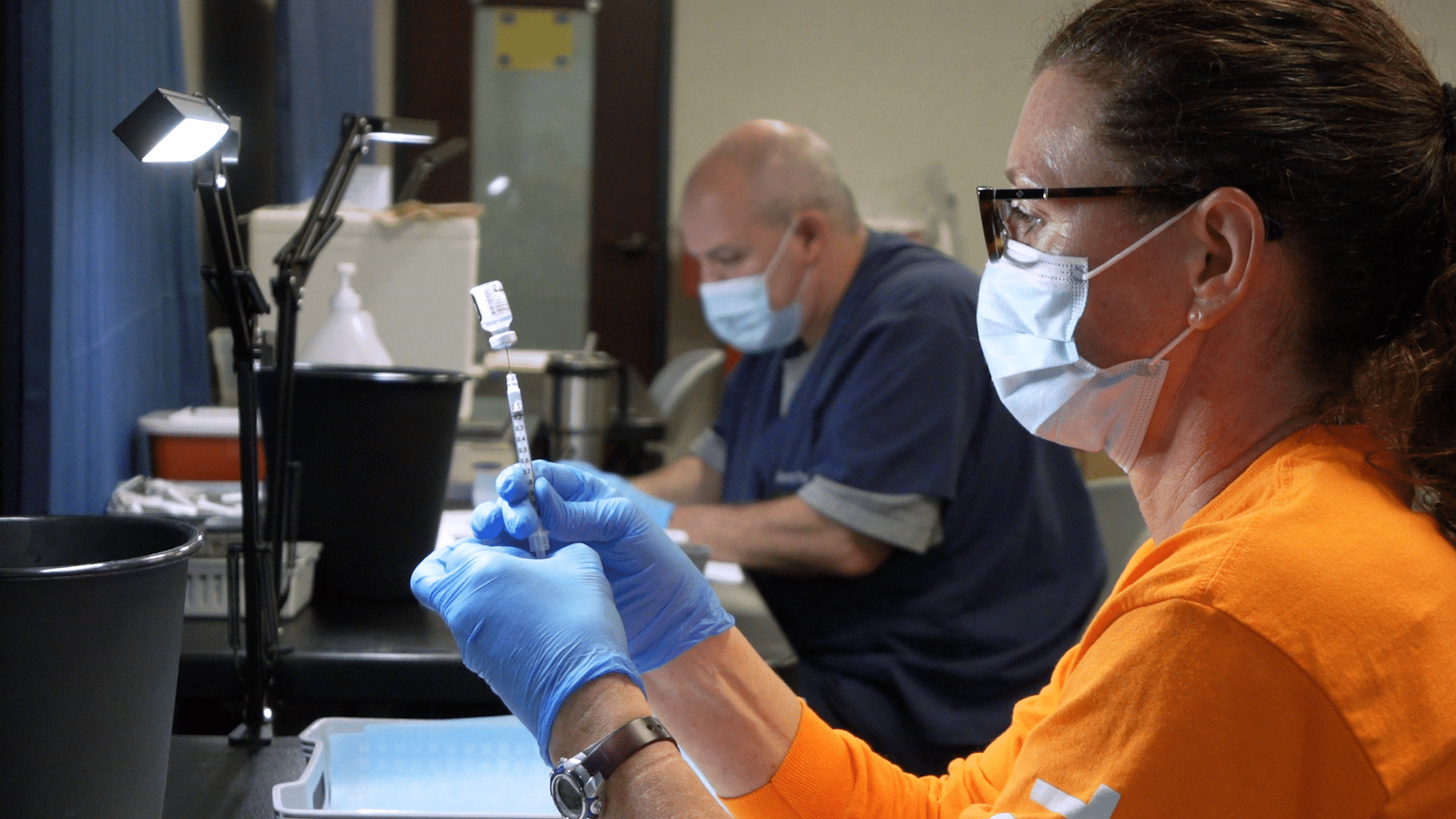
Greenville, N.C. – Oct. 1, 2021 – Community members who received their first two Pfizer-BioNTech COVID-19 vaccine doses at least 6 months ago and meet the specified criteria below can now schedule a COVID-19 booster shot appointment through Vidant Health by visiting VidantHealth.com/Vaccinate or calling 252-847-8000.
PFIZER BOOSTER SHOT FOR 65+ AND HIGH RISK COMMUNITY MEMBERS
Vidant is offering booster shots to eligible community members in accordance with the North Carolina Department of Health and Human Services (NCDHHS) guidelines. Appointments can be scheduled at Vidant clinics throughout the region if it has been at least 6 months since your second dose of the Pfizer vaccine and you meet at least one of the below criteria:
- You are 65 or older.
- You are 18 or older and live in a long-term care facility.
- You are 18 or older, have a medical condition that puts you at high risk for severe COVID-19, and believe the benefit of receiving a booster outweighs the risk of receiving the booster.
- You are 18 or older, are higher risk of exposure due to work or living situations, and believe the benefit of receiving a booster outweighs the risk of receiving the booster.
The booster shot is authorized by the Food and Drug Administration (FDA) for individuals at least 6 months after their second dose of the Pfizer vaccine and is not currently authorized for those who received the Moderna vaccine or Johnson & Johnson’s Janssen COVID-19 vaccine.
THIRD DOSE FOR IMMUNOCOMPROMISED – PFIZER AND MODERNA ONLY
In addition to the new booster shot eligibility, Vidant previously announced it is closely following Centers for Disease Control and Prevention (CDC) guidance to provide third doses to eligible community members. A third dose may prevent serious and possibly life-threatening complications of COVID-19 in immunocompromised people who may not have responded to their initial vaccine series.
Appointments can be scheduled at Vidant clinics and oncology practices throughout the region for community members who meet the below criteria:
- You’ve had an organ or stem cell transplant.
- You’re receiving chemotherapy, other treatment for cancer or tumors, taking biologic agents (Humira, Enbrel, Remicade, etc.), taking high doses of prednisone, or taking similar drugs. Many of these drugs are used for treatment of cancer, Crohn’s disease, rheumatoid arthritis, or psoriasis.
- You have a disease that weakens your immune system (like HIV or a primary immune system disease).
- Your doctor told you that you’re immunosuppressed.
The third dose is recommended for immunocompromised individuals at least 28 days after their second dose of the Pfizer or Moderna vaccine and is not recommended for those who received Johnson & Johnson’s Janssen COVID-19 vaccine. The Pfizer-BioNTech COVID-19 vaccine is also identified by its new brand name Comirnaty.
Please continue checking back to VidantHealth.com/Vaccinate for the latest information on Vidant’s vaccine efforts.
Roanoke Rapids, N.C. – Sept. 10, 2021 – Vidant North Hospital is proud to announce it has received re-certification for its Joint Care Center, an acknowledgement of nationally recognized standards for joint care patients. This marks Vidant North’s third certification since 2017.
Certification is a process through which health care organizations demonstrate compliance with national standards. This certification highlights Vidant North’s Joint Care Center standing as an outstanding resource for in the community and provides the services and treatments nearby, allowing patients the convenience of quality care close to home.

“The Total Hip and Total Knee Replacement certification program is designed to assist health care organizations to provide high quality, comprehensive health care with an emphasis on patient safety,” said Tracy Olesnevich, director of acute care services at Vidant North. “We are pleased to once again receive this recognition of continued excellence in coordinated and comprehensive care for patients receiving joint replacements.”
Since its inception in 2005, the Vidant North Joint Care Center has provided the highest level of care to patients and has helped them return to previous levels of mobility so that they may continue to enjoy the activities that enhance their lives. The convenience of having high-quality joint care close to home is key to Vidant’s mission of improving the health and well-being of eastern North Carolina.
During the certification process, Vidant North’s Joint Care Center is evaluated on quality outcomes including patient experience and satisfaction. Dedicated specifically to joint replacements, Vidant Joint Care gives patients a sense of community by spending time with other patients who are undergoing the same surgeries. The experiences of comradery between patients in this unit is one of the factors why many choose to return to Vidant Joint Care when they have future joint replacement needs.
“Enhancing patient care is at the forefront of Vidant North’s efforts to meet the mission of improving the health and well-being of eastern North Carolina,” said Jason Harrell, president of Vidant North. “We are proud of this certification and the commitment of our team members across all levels and services to make this a reality.”
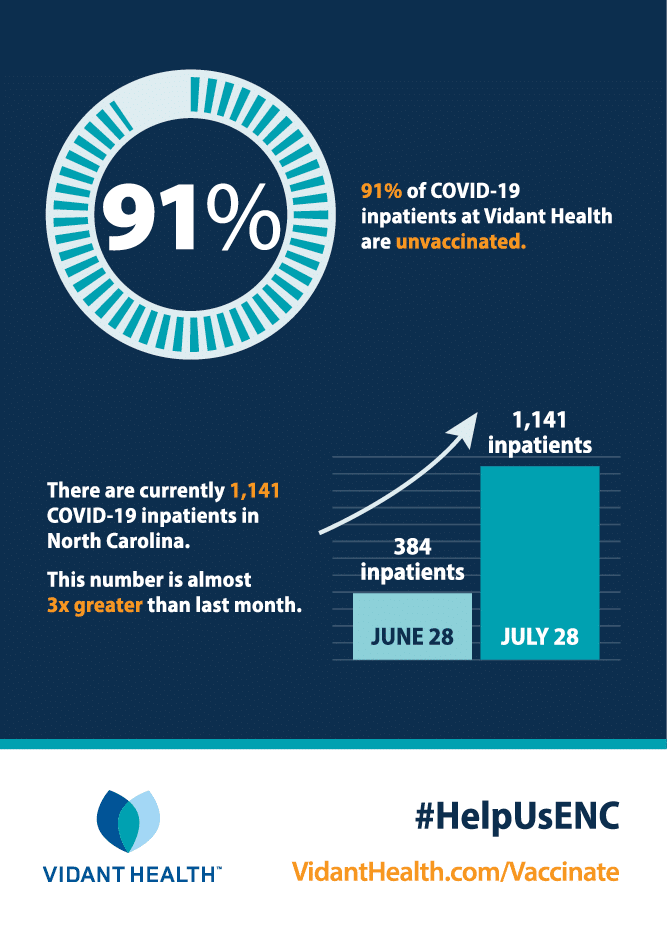
As part of our commitment to protecting and caring for those we love, Vidant will require the COVID-19 vaccine as a condition of employment for all team members, physicians, credential providers and contract workers.
This decision is grounded in science, backed by industry leaders such as the American Hospital Association, American Nurses Association and the North Carolina Healthcare Association, and is the right thing to do to ensure the safety of our patients, team members and communities.
Timeline:
- Leaders (managers and above), physicians and credentialed providers – Deadline to complete vaccine series: Oct. 1, 2021
- Team members, new hires, contract workers – Deadline to complete vaccine series: Dec. 1, 2021
Exemptions:
In addition to other important safety measures like the flu vaccine, the COVID vaccine will become a condition of employment; which means in order to be employed by or work at Vidant, team members must be vaccinated by the deadlines outlined above or have an approved medical or religious exemption. Ongoing requirements for those meeting medical/religious exemptions may include weekly testing and potential reassignment away from working on units with immuno-compromised patients.
Meeting the mission to improve the health and well-being of eastern North Carolina means taking all necessary actions to combat and hopefully end the COVID-19 pandemic, which has claimed more than 600,000 American lives. Several hospitals and health systems in North Carolina, and many across the nation, have already announced vaccine requirements for their team members. It is the right thing to do for the safety of all, especially as the variants prove to be more transmissible and severe for those not vaccinated.
 Greenville, N.C. – July 19, 2021 – ECU Health Medical Center (VMC) is proud to announce it recently joined the American Trauma Society’s (ATS) network. VMC is one of only 130 hospitals in the United States designated as a Trauma Survivors Network (TSN) facility. TSN links survivors and their families with others who have shared experiences, providing support and resources to enable victims to rebuild their lives.
Greenville, N.C. – July 19, 2021 – ECU Health Medical Center (VMC) is proud to announce it recently joined the American Trauma Society’s (ATS) network. VMC is one of only 130 hospitals in the United States designated as a Trauma Survivors Network (TSN) facility. TSN links survivors and their families with others who have shared experiences, providing support and resources to enable victims to rebuild their lives.
“We are extremely excited to provide resources patients and families need to recover both mentally and physically,” said Bryan Lake, trauma outreach coordinator at VMC. “Our goal is to compassionately support our survivors and community through all stages of trauma recovery. We have a unique, life-changing opportunity to guide patients and families through uncharted waters and convey the understanding they are not alone in this journey.”
The program aims to help survivors manage day-to-day challenges after a traumatic injury as well as bring together trauma survivors and families to connect with one another and share support and information about the recovery process.
Additionally, the TSN will collaborate with health care providers to deliver specifically tailored care and support to patients and their families and friends after a traumatic injury and will help build a community of advocates dedicated to improving injury prevention efforts and treatment.
“As one of only six hospitals in North Carolina to have earned Level I Trauma Center status, VMC is proud to offer quality care for trauma patients and their families and values this opportunity to further support them beyond the doors of the hospital,” said Lake. “Trauma patients will now have a community of people experiencing similar hurdles while adjusting to life after a traumatic injury.”
When a trauma patient is admitted to VMC, coordinators will introduce patients and families to the program. The network is open to all ages, from children to adults. Participants will be connected with other members both in the local area and around the country through virtual and in-person support groups.
The network is open to survivors, previous trauma patients, families, friends, health care workers and any community members. Those interested in joining the Trauma Survivors Network can visit its website to learn more.
 Roanoke Rapids, N.C. – July 15, 2021 – Vidant North Hospital is proud to announce it has been designated as a primary stroke center by The Joint Commission and the American Heart/Stroke Association, recognizing the hospital’s preparedness and expertise to care for stroke patients. Stroke is one of the leading causes of death in the state, resulting in more serious long-term disabilities than any other disease.
Roanoke Rapids, N.C. – July 15, 2021 – Vidant North Hospital is proud to announce it has been designated as a primary stroke center by The Joint Commission and the American Heart/Stroke Association, recognizing the hospital’s preparedness and expertise to care for stroke patients. Stroke is one of the leading causes of death in the state, resulting in more serious long-term disabilities than any other disease.
According to the North Carolina State Center for Health Statistics, both Halifax and Northampton counties show increase incidences of stroke disease and mortality compared to the North Carolina average. “Here in eastern North Carolina we are at the center of a lot of strokes. North Carolina is about 8 percent worse for stroke mortality than the rest of the nation and in eastern North Carolina it is even a bigger risk,” said Dr. Richard Dalyai, neurosurgeon and surgical director of stroke services at Vidant Health. “Providing high-quality stroke care close to home is central to our mission of improving the health and well-being of eastern North Carolina.”
As a primary stroke center, Vidant North can treat and stabilize patients experiencing an acute stroke and care for more complex patients. Because time is one of the most important factors in treating stroke, it is vitally important to provide stroke care close to home. Vidant North’s stroke certification increases proximity to quality care in the Roanoke Rapids area, which reduces the risk of mortality, permanent brain damage and other side effects including memory loss, difficulty speaking and potential paralysis.
During the certification process, Vidant North was evaluated on performance measures in stroke care, including education for patients and families on stroke risk factors and recognizing symptoms of stroke. Other performance measures included staff education on stroke protocols and the appropriate prescription of medications to address stroke risk factors such as elevated cholesterol.
“Stroke certification from The Joint Commission represents Vidant North Hospital’s commitment to provide high-quality stroke care to not only patients experiencing stroke symptoms, but to all of our patients,” said Jason Harrell, president of Vidant North. “We are proud of being designated a primary stroke center and the commitment and diligent work of our team members across all levels and services to make this a reality.”
Greenville, N.C. – June 28, 2021 – The 2021 Vidant Health Board Quality Leadership Award winners were recently recognized by the Vidant Health Board of Directors for their improvement of patient care. These winning teams are a representation of excellent work across the system that drives the quality goal of zero harm, creates exceptional experiences and improves patient outcomes. Nine nominations were reviewed by the committee and the winning teams are as follows:

- Vidant Edgecombe Hospital: “Impact of a Palliative Care Program in a Community Hospital” was selected for its work in reducing the mortality rate and readmission rate by five percent.
- Vidant Family Medicine – Edenton: “Responding to COVID-19: Building an Airplane While Flying” for its work to establish a fully functioning respiratory clinic by April 9, 2020, that would see patients requiring screening, testing and treatment for COVID-19 infections.
- ECU Health Medical Center, Maynard Children’s Hospital team: “A Sustained Improvement in CLASBI Reduction” for its work to reduce central line associated blood infections in Maynard Children’s Hospital by 50 percent.
To receive this honor, team members submitted projects that demonstrated at least two of the following requirements:
- Quantifiable improvement in an organizational quality priority with sustained excellence over time
- Demonstration of empathy and compassion in patient care
- Implementation of innovative solution to patient care problem
- Community outreach that addresses the social determinants of health in a meaningful way
“We are proud to see team members from across Vidant Health recognized for their hard work and dedication to patient care,” said Dr. Shirley Carraway, Ed. D, chair of the Vidant Health Board of Directors. “The pandemic brought unique challenges to healthcare and these team members continued to innovate and improve the health and well-being of eastern North Carolina, and we are proud to honor them in this way.”
 Greenville, N.C. – June 30, 2021 – ECU Health Medical Center (VMC) is participating in TAKEHeart, a national initiative funded by the Agency for Healthcare Research and Quality, to make a positive impact on the lives of patients by encouraging greater participation in cardiac rehabilitation. The initiative will help easily connect patients with cardiac rehabilitations services to improve their heart health and reduce the risk of future heart issues. As a TAKEHeart partner, VMC cardiac and pulmonary team members will receive advanced training, coaching and technical support as well as shared learning about cardiac rehabilitation best practices.
Greenville, N.C. – June 30, 2021 – ECU Health Medical Center (VMC) is participating in TAKEHeart, a national initiative funded by the Agency for Healthcare Research and Quality, to make a positive impact on the lives of patients by encouraging greater participation in cardiac rehabilitation. The initiative will help easily connect patients with cardiac rehabilitations services to improve their heart health and reduce the risk of future heart issues. As a TAKEHeart partner, VMC cardiac and pulmonary team members will receive advanced training, coaching and technical support as well as shared learning about cardiac rehabilitation best practices.
“Patients are more likely to survive an acute heart episode when they engage in cardiac rehabilitation,” said Stacey Greenway, director of cardiovascular disease management programs at VMC. “We know that only a small percentage of patients complete cardiac rehabilitation. Participating in TAKEHeart means bringing best practices and strategies in cardiac rehabilitation to Vidant and eastern North Carolina to improve outcomes for patients suffering from a cardiac episode.”
Approximately 1 million Americans have a coronary event or surgery each year, but only 20 percent are referred to cardiac rehabilitation. Among Medicare-eligible heart attack patients, only 6.5 percent complete the recommended cardiac rehabilitation sessions. Cardiac rehabilitation eases patients into heart-healthy exercises, nutrition education and education on how to manage risk factors such as stress. People who have cardiac rehabilitation after a heart episode have lower mortality rates, fewer hospital admissions and readmissions and higher quality of life.
The eastern North Carolina population faces a disproportionate risk of heart disease. According to the Agency for Healthcare Research and Quality, patients who complete cardiac rehabilitation sessions have a 47 percent lower risk of death and a 31 percent lower risk of a heart attack than those who attend only one session.
“One of the most important benefits to patients participating in a cardiac rehabilitation program is learning how to take charge of their own health and become more engaged partners with their health care team,” Dr. Noel Peterson, cardiologist at Vidant Health, said. “Our care teams are excited to continue to partner with patients and provide advanced cardiac rehabilitation services to eastern North Carolina.”
Cardiac rehabilitation is a combination of medical care and counseling to improve cardiovascular health after a heart attack, heart failure, angioplasty, or heart surgery has taken place. It may include exercise counseling and training, lifestyle education (e.g., nutrition and reducing risk factors) and efforts to manage stress.
“It is broader than just diet and exercise,” said Greenway. “Factors like learning how to be more proactive about health and providing better access to resources can make an impact. Living in a rural area can create a barrier to resources, which makes these initiatives so critical to this region. By providing improved access to rehabilitation services, we can help patients find creative ways to improve their heart health through ongoing education and lifestyle changes.”
 Greenville, N.C. – June 21, 2021 – Vidant Health, the Eastern Carolina Injury Prevention Program (ECIPP), Veteran’s Affairs (VA) and the Greenville Police Department (GPD) are proud to announce the formation of the Pitt County Firearm Safety Coalition (PCFSC), a non-partisan, apolitical group with the goal of reducing injuries and death from firearm violence through education and safe storage techniques.
Greenville, N.C. – June 21, 2021 – Vidant Health, the Eastern Carolina Injury Prevention Program (ECIPP), Veteran’s Affairs (VA) and the Greenville Police Department (GPD) are proud to announce the formation of the Pitt County Firearm Safety Coalition (PCFSC), a non-partisan, apolitical group with the goal of reducing injuries and death from firearm violence through education and safe storage techniques.
PCFSC will partner with stakeholders representing various sectors in the community, including the VA, GPD, East Carolina University, health care providers, Child Protective Services, Pitt County Health Department, faith-based groups, wildlife and hunting organizations, gun manufacturers and schools to identify solutions and impactful interventions.
“Firearm injuries have increased at an alarming rate in our state and in our region in recent months,” said PCFSC member Dr. Shannon Longshore, who serves as medical director of Injury Prevention and Pediatric Trauma for ECIPP. “We know each injury and each life lost is devastating to our community. The Pitt County Firearm Safety Coalition works together to prevent firearm injuries with proven solutions such as safe handling and storage and by addressing issues we see locally.”
Firearms are among the top five leading causes of injury-related deaths and account for half of all suicides, according to the Center for Disease Control and Prevention National Center for Injury Prevention and Control. Safe storage of firearms decreases the risk of accidental discharge by a child. Additionally, evidence suggests those living in households where firearms are stored and locked have a lower risk of suicide than those where firearms are stored unlocked.
“Increasing the time and distance between someone with suicidal intent and firearms can reduce suicide risk,” said PCFSC member Tiffany Chavis, senior social worker, suicide prevention coordinator, Durham VA Health Care System. “Providing education and resources to keep firearms safely secured, especially during mental health crises, is crucial in reducing the number of suicides. The Pitt County Firearm Safety Coalition demonstrates how well partners can work together for shared purpose, even if the populations differ.”
PCFSC has launched a firearm safety awareness campaign: “Lock It For Love – Firearm Safety is OUR Responsibility” to encourage the safe storage of firearms in order to reduce the number of firearm injuries in the region. GPD recently partnered with Project ChildSafe to get free gun locks, which will be distributed to local firearms owners/families.
“As police officers we often encounter people during some of the worst times of their lives, but our jobs take on an entirely new meaning when a child loses their life, especially to unnecessary gun violence,” said Chief Mark Holtzman of GPD. “The Greenville Police Department is humbled to be a partner in the Pitt County Firearm Safety Coalition to raise awareness for this very important cause. There is strength in numbers, and the safety and well-being of the members of our community is truly a collaborative effort. Together, we hope to make a difference and save lives.”
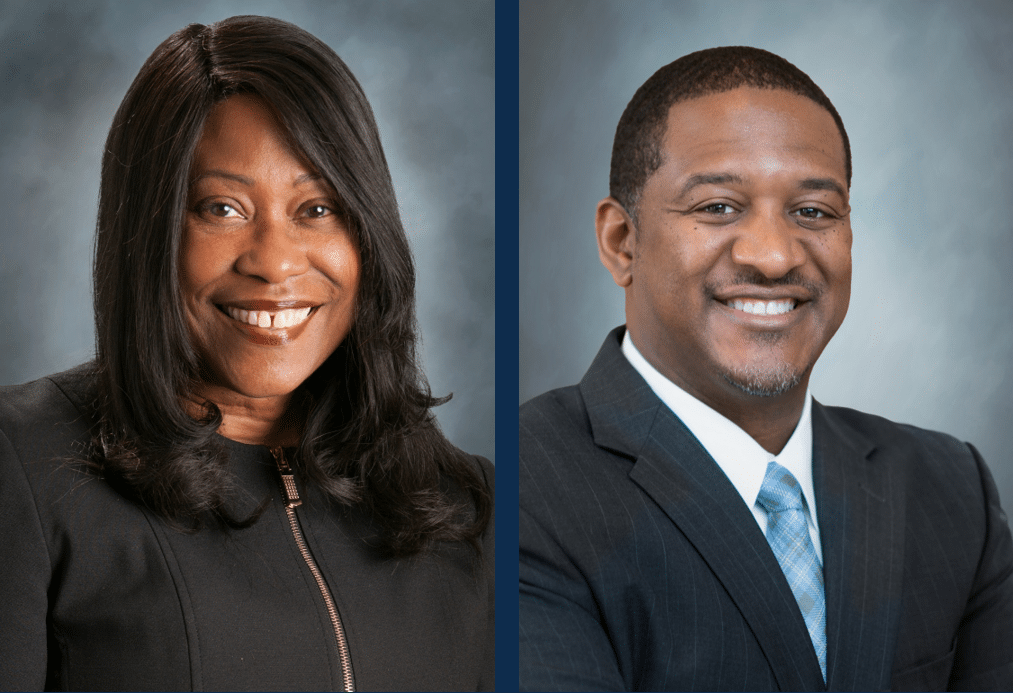
Greenville, N.C. – June 9, 2021 – Vidant Health is pleased to announce that effective June 21, Charlene J. Wilson, Ed.D(c), MPA, CCP will assume the role of Chief Human Resources Officer and Mark F. Dunn, CPC, MSL will become Vidant’s first Chief Diversity, Inclusion and Talent Management Officer. These decisions were made following an extensive interview process with members of the Vidant Health Board of Directors and leaders from across the organization.
“This is an exciting time for our organization as we continue to make important strides in our mission to improve the health and well-being of eastern North Carolina,” said Vidant CEO Dr. Michael Waldrum. “Both Charlene and Mark understand the importance of Vidant’s role as a major employer in the region and our commitment to recruiting and retaining high-quality team members. I want to thank John Marques, who will be retiring at the end of June, for his leadership as Chief Human Resources Officer over the past six years and for building a solid foundation upon which we can continue to grow.”
Incoming Chief Human Resources Officer

Charlene J. Wilson
As incoming CHRO, Wilson will oversee and provide strategic direction for the teams and programs within, HR Service Delivery, Talent Acquisition, HR Information Systems, Total Rewards, HR Business Partners and Team Member Relations.
“I am honored to step into the Chief Human Resources Officer role,” said Wilson. “At Vidant, we know high-quality team members are the driving force behind high-quality care. Our patients, their families and the communities we serve depend on us to provide the best care possible. I am proud to work on behalf of our 13,000 team members to ensure Vidant is a premier employer not just in the region, but in the state.”
Joining Vidant in 2016, Charlene has served as Vice President of Human Resources for ECU Health Medical Center and was appointed as Vice President, HR Business Partners in August 2020, leading and collaborating with HR leaders and teams in a variety of initiatives including HR transformation, operational efficiency across the system and workforce strategy and management.
With over 20 years of experience in human resources leadership, Wilson has worked at hospitals and health systems across the country. She received her bachelor’s degree from Hampton University and her master’s degree from Villanova University. Charlene is currently pursuing her doctorate in organizational leadership from Grand Canyon University.
New Chief Diversity, Inclusion and Talent Management Officer

Mark F. Dunn
Over the past five years, Vidant has placed a continued focus on diversity, equity and inclusion. As Chief Diversity, Inclusion and Talent Management Officer, Dunn will lead Vidant’s diversity, equity and inclusion vision and strategic direction by collaborating with several functions within the organization and out in communities across the region to align and implement inclusive-focused initiatives and programs.
In his new role, Dunn will continue to lead Organization and Leadership Development and Workforce Experience and Development. These teams contribute to building an engaged workforce culture by focusing on the equitable development of team members within Vidant.
“I am grateful for this opportunity to lead the organization in the areas of diversity, inclusion and talent management,” said Dunn. “This work is one of my life’s passions and I am excited to step into this position where I will lead with a servant’s heart and collaborate with key partners to reach the organization’s equity and inclusion goals.”
Dunn joined Vidant in 2019 as the Vice President of Organization and Leadership Development, which led to additional oversight of Talent Acquisition as well as partnering with Office of Experience in the equity and inclusion space.
He has family ties to eastern North Carolina and received his bachelor’s degree from University of North Carolina, along with his master’s degree in leadership and organizational change from Pfeiffer University. Prior to joining Vidant, Dunn led the functions of talent management and learning and organizational development within the higher education and health care industries.
 Greenville, N.C. – June 2, 2021 – Vidant Health is proud to announce that EastCare – the premier medical transportation agency in the region – recently became one of the first medical flight programs in North Carolina to carry O Negative Whole Blood, which will help improve patient survivability in eastern North Carolina. Whole Blood contains all the components of blood that the body loses during trauma events and helps replenish all necessary blood components.
Greenville, N.C. – June 2, 2021 – Vidant Health is proud to announce that EastCare – the premier medical transportation agency in the region – recently became one of the first medical flight programs in North Carolina to carry O Negative Whole Blood, which will help improve patient survivability in eastern North Carolina. Whole Blood contains all the components of blood that the body loses during trauma events and helps replenish all necessary blood components.
“Vidant Health serves a vast rural environment with long distances in between towns and sometimes between providers,” said Chuck Strickland, Outreach Coordinator. “Trauma patients often need immediate treatment, and that’s what the O Negative Whole Blood allows us to do. Helicopters carrying O Negative Whole Blood can increase the chance of survivability of trauma patients in eastern North Carolina while being transported from these rural areas to hospitals.”
O Negative is the rarest blood type and compatible with all other blood types, making it an important life-saving intervention for those suffering from serious traumatic events. EastCare collaborated with the Brody School of Medicine at East Carolina University to obtain the O Negative Whole Blood from the American Red Cross.
Recent studies show that patients who receive Whole Blood products early typically require less blood transfusions while in the hospital. This may also improve 24-hour patient survival by 23 percent and reduce the patient’s length of stay, according to a recent study.
“O Negative Whole Blood is vitally important to our collective mission because it is a universal donor,” said Dr. Darla Liles, ECU Professor of Medicine and Chairman of the Vidant Patient Blood Management Committee. “This blood can be administered quickly in the field when a patient has suffered a serious trauma and is bleeding too rapidly to make it back to the hospital. Our Vidant Patient Blood management committee is thrilled to work with EastCare to create this unique program, which has the potential to save lives here in eastern North Carolina.”
O Negative Whole Blood is carried on all 5 EastCare helicopters and can be utilized on ground ambulances as needed. In addition to the Whole Blood innovation, EastCare will continue to carry Fresh Plasma and Packed Red Blood Cells.