Greenville, N.C. – ECU Health is pleased to announce Brian Harvill, CPA, MBA, has officially been named president of ECU Health Roanoke-Chowan Hospital and Dennis Campbell, II, DHA, RN, NEA-BC, has officially been named president of ECU Health Beaufort Hospital, a campus of ECU Health Medical Center, effective immediately.
“As we work toward the realization of ECU Health’s vision of becoming the national model for academic rural health care, the importance of collaboration, teamwork and knowing and understanding the unique needs of the communities we serve cannot be overstated,” said Jay Briley, president of ECU Health Community Hospitals. “I appreciate Dennis’ and Brian’s ongoing commitment and leadership to ECU Health and eastern North Carolina, and I am excited about what formalizing their leadership roles in these areas will mean for the health system and the rural communities we serve.”

Brian Harvill
After serving as interim president at Roanoke-Chowan Hospital since March 2023, Harvill will officially become president of Roanoke-Chowan Hospital while also continuing in his role as president of ECU Health Bertie and Chowan Hospitals. Through his leadership and collaborative approach, Harvill has successfully balanced and led the three hospitals throughout the past six months. His unique skillset and leadership ability has led to the development of a strong culture of team work and excellence in patient and team member experience and quality of care.
Harvill has been with ECU Health for 11 years, serving in financial and administrative leadership roles. Prior to joining ECU Health, he was director of Corporate Accounting for Atrium Health (formerly Carolinas HealthCare System), where he served for 17 years. He has a dedicated focus on serving the people of eastern North Carolina as evidenced by his membership in and leadership of various local professional and civic organizations.
“I am honored to continue collaborating with the entire team at ECU Health Roanoke-Chowan Hospital, which has a rich legacy of providing high-quality care to Ahoskie and the surrounding communities,” said Harvill. “I look forward to continuing in the role of president and working on behalf of our patients and team members as we continue to strive towards the collective mission of improving the health and well-being of the region.”

Dennis Campbell, II
Additionally, after serving as interim president at ECU Health Beaufort since February 2023, Campbell, II will officially serve as president of the hospital. During his time at ECU Health Beaufort, Campbell, II has prioritized developing relationships with important stakeholders and partners in the area including Beaufort Community College and ECU, exemplifying his dedication to investing in the future of health care in eastern North Carolina.
Campbell, II has been with the health system for three years, previously serving as ECU Health Beaufort’s vice president of Patient Care Services. In his time with the system, Campbell, II has been an important voice and visionary through a time of change for ECU Health Beaufort. He played a crucial role in two recent major initiatives for the health system: the transition of Beaufort to become a campus of ECU Health Medical Center and the introduction of the Nurse Travel Staffing program.
“This is a time of great transformation for ECU Health Beaufort and I am deeply appreciative for the opportunity to continue to lead this great team through these exciting times,” said Campbell, II. “I am passionate about serving the Beaufort community and being part of a hospital and care team that tirelessly serves patients and their loved ones during times of great need.”
Tony Khoury, CBI, M&AM, has been appointed by the Pitt County Commissioners to the ECU Health Medical Center Board of Trustees effective June 26, 2023.
 Khoury has over 30 years of business ownership experience, with an emphasis on working with privately held businesses within the manufacturing, wholesale/distribution, construction, health care, and technology sectors. He is a Senior Business Broker and the Founder/Owner of Transworld Business Advisors of eastern North Carolina, headquartered in Greenville.
Khoury has over 30 years of business ownership experience, with an emphasis on working with privately held businesses within the manufacturing, wholesale/distribution, construction, health care, and technology sectors. He is a Senior Business Broker and the Founder/Owner of Transworld Business Advisors of eastern North Carolina, headquartered in Greenville.
Khoury holds an undergraduate degree in Electrical Engineering from Youngstown State University and a Master of Business Administration degree from Duke University’s Fuqua School of Business. Khoury has a strong passion for helping the communities of eastern North Carolina by attracting investment and improving the lives of its residents. He serves on the board of directors of the NC East Alliance, a 29-county economic development nonprofit, as well as on the advisory board of the SBTDC (Small Business Technology Development Center).
The governing board of ECU Health Medical Center sets policies guiding the operation and direction of the hospital and its subsidiaries. The governing board serves on behalf of the community, providing ideas for new programs and supporting existing ones. Members are charged with bringing the community’s voice to the health care system and, in turn, sharing the organization’s story in the community. Board members serve voluntarily and without pay.
KENANSVILLE – You could say Jon Kornegay was born to be a rural doctor. His father was a physician in a small town in Duplin County in eastern North Carolina. His mother was a graduate of East Carolina University’s first nurse practitioner class in 1976.
But it was his experience at ECU’s Brody School of Medicine that sealed the deal.
“Even early on in my medical school I saw the emphasis on service. You see other members (at the school), attending physicians and professors, who live that life and lives of service,” he said recently during a break from his job as a hospitalist at ECU Health Duplin Hospital in Kenansville. “Then you get exposed early on to underserved areas and populations and see how rewarding that can be.”

ECU’s medical school was established in 1974 after successfully making the argument – contentious at the time – that it could fill a need in North Carolina to train more primary-care physicians, rather than medical specialists, and find more doctors willing to serve in places like Kenansville.
Since then it has made good on that promise: according to the American Academy of Family Physicians, Brody ranks second in the nation among medical schools in the percentage of family physicians it graduates. The school admits 86 students to each class, all from North Carolina; this year, 52% of Brody’s graduates entered primary-care residencies.
“Developing great primary-care providers for rural areas is at the core of what we do at Brody and within ECU Health,” says Dr. Michael Waldrum, dean of Brody and CEO of ECU Health. “We have students, professors, residents and doctors who really understand that side of health care, and their work in that space leaves a legacy that we can all be proud of.”
A reliable supply of physicians and medical professionals is a critical part of the economy of any rural community:
- Having primary care close to home means residents are more likely to seek treatment for medical problems before they become crises and less likely to have to leave home to get treatment, resulting in fewer missed days of work and better quality of life;
- A healthy medical community is an important selling point for developers recruiting new businesses and for families trying to decide where to move;
- Rural hospitals are among the biggest employers in a county; since 2005, 12 rural hospitals have closed across the state, part of a troubling national trend;
- And medical professionals contribute in other ways. Kornegay also serves as the county’s EMS medical director; one of his colleagues also serves as county health director; other medical professionals serve on chambers, chair charitable boards, and coach sports teams.
Kornegay knows work in rural health care is not for everyone: Physicians can generally make more in cities in highly specialized fields; rural areas don’t offer the same amenities. Overcoming those barriers, he says, will require a variety of approaches, including improved salaries, help with loan repayment, retention bonuses and Medicaid expansion.
But in the meantime, Kornegay finds some people fall in love with work in rural areas, for the quality of life, the chance to get to know patients and neighbors in a deeper way, and for the opportunity to solve a wide range of health concerns.
Kornegay, certified as both an internist and a pediatrician, will often move from a geriatric patient in an ICU to a newborn down the hall.
“If you can get doctors into rural settings for a little while – get to know the environment, get to build their social network, get that experience … you have a chance to keep ‘em,” he says.
Something’s working in Duplin County. All five full-time physicians in Kornegay’s group at Duplin Hospital either went to med school or did their residency at Brody. They join a cadre of other ECU grads in health care and other fields who put down roots in the county.
“There’s a lot of purple and gold here,” says Kornegay. “That’s for sure.”
Further reading on Higher Ed Works
“Eastern North Carolina needs us”: The economic impact of ECU
Greenville, N.C. – ECU Health Medical Center recently earned accreditation from the Commission on Cancer (CoC), a quality program of the American College of Surgeons (ACS). This accreditation means patients will receive comprehensive, personalized care provided by a team of specialists working closely together, access to information on clinical trials and new treatment options, ongoing monitoring of care and lifelong follow-up, mental health support, financial guidance, survivorship care and other long-term services.
“I am proud of our ECU Health team members and physicians who work hard to provide the most advanced cancer care to eastern North Carolina,” said Brian Floyd, president of ECU Health Medical Center and chief operating officer of ECU Health. “Cancer is a terrible disease that has touched most, if not all, of us in some way. As a regional academic medical center, ECU Health Medical Center strives towards excellence in all it does. This accreditation is a testament to the tireless efforts of our cancer care teams, who make a difference in the lives of so many in our region.”

As a CoC-accredited cancer center, ECU Health Medical Center applies a multidisciplinary approach and treats cancer as a complex group of diseases that requires consultation among surgeons, medical and radiation oncologists, diagnostic radiologists, pathologists, and other health care professionals that specialize in caring for cancer patients. Cancer patients benefit from having access to clinical trials, screening and prevention events, palliative care, genetic counseling, rehabilitation, oncology nutrition, and survivorship services.
“Eastern North Carolina faces a disproportionately high rate of cancer, and as the largest health care provider in the East, ECU Health is committed to maintaining excellence in the delivery of comprehensive, compassionate, patient-centered, high-quality care for patients with all types of cancer,” said Dr. Darla Liles, Cancer Committee chair at ECU Health, professor and chief of the Division of Hematology and Oncology at the Brody School of Medicine at East Carolina University. “This accreditation demonstrates our holistic approach to cancer care that includes preventive measures, educational resources, clinical trials, support and survivorship services and treatment with the latest technologies and highest clinical standards.”
According to the American Cancer Society, more than 1.9 million new cancer cases and approximately 609,820 deaths from cancer are expected in 2023 in the United States. Of those, 67,690 new cases are expected in North Carolina. Residents in eastern North Carolina have access to ECU Health’s cancer care network that spans across nine hospitals – including the Eddie and Jo Allison Smith Tower at ECU Health Medical Center in Greenville that is home to both inpatient and outpatient cancer services – five radiation oncology sites, three joint ventures and numerous outpatient clinics.
“The Commission on Cancer brings together experts and advocates from across the country to develop standards for cancer care so that patients with cancer receive the highest quality care coordinated by a team of dedicated physicians and specialists,” said Timothy Wm. Mullett, MD, MBA, FACS, professor, general thoracic surgery medical director, Markey Cancer Center Affiliate and Research Networks University of Kentucky, and chair of the Commission on Cancer.
As the fall season begins and young students head back to school, safety is top of mind for the Injury Prevention and School Health programs at ECU Health Medical Center.
Laurie Reed, nurse manager for the School Health Program, said starting the school year out on the right foot begins with staying healthy. Reed said it is important for parents to make sure children have an annual physical exam with a primary care provider to make sure they are healthy and have what they need to be successful in the classroom.
For students entering public schools for the first time, a health assessment is required by a physician within 12 months of starting school. Reed said providers need to fill out a form and have it submitted to the school.

“If their child has had a physical in the last year, it may just be a matter of taking that form to the provider’s office to have them complete it,” Reed said. “If they haven’t had that physical in the last year, it’s really important that they go ahead and reach out to their child’s doctor to get that appointment scheduled.”
Additionally, she noted the importance of students being up-to-date on their vaccines to help keep them in school. Reed said there are specific vaccines and boosters for children as they reach kindergarten, 7th grade and 12th grade, all of which should be part of their annual physicals.
Reed said it’s important to understand that these vaccines and boosters are all part of keeping young students healthy and in the classroom.
“These are actually diseases that are still out there and that children actually could get if they don’t receive vaccines,” Reed said. “Of course, in a school environment where children are in close conditions, it’s a public health concern if we would have a student that would come down with one of these illnesses. If other students are not vaccinated, then, of course, then it could it could spread within a school setting. Generally, just for their overall good health, it’s just very important that students are receiving their vaccines on a routine basis.”
Reed encouraged families to contact their local school nurse or the Maynard Children’s Hospital for more information.
School bus safety
Another important aspect of back to school safety focuses on our roads.
Ellen Walston, Injury Prevention Program coordinator at ECU Health Medical Center, urged motorists to use caution when driving near school buses and in school zones.
Walston said that distracted driving is a problem and to combat that challenge, some modifications have been made in school zones in the area. These updates include mounted speed boards and flashing beacons at crosswalks to alert drivers to pedestrians.
“It is really important that we emphasize distractions within school zones and any time that you’re driving,” Walston said. “Students are also distracted when they’re walking to and from school. So any education we can provide around that is important and that applies to the driver as well as a pedestrian.”
Richard Hutchinson, director of transportation for Pitt County Schools, said it’s crucial for drivers to follow the law and stop when a bus is at a pick up or drop off spot to keep children safe.
Hutchinson shared that over 3,000 stopped school buses are passed each day in North Carolina and this creates a risk for children. He asked that drivers follow the law, stop and wait for the school bus to continue.
“As soon as you see the amber lights come on, it would be good to slow down and be prepared to stop,” Hutchinson said. “If the busses come to a stop, you should come to a stop, even if that stop arm has not come out yet. That’s just going to help keep everyone safe.”
Resources
For the second year, Susan Callis, recreational therapist with ECU Health, volunteered her time to serve as a swim partner in The Crossing on Aug. 12.
The one-mile event is held annually at Lake Gaston, and participants can swim, float, paddle or walk the distance to raise funds that support the Lake Gaston community.
Last year, Callis worked with Brent Carpenter, a former ECU Health outpatient, to help him swim the distance.
“It was his idea,” Callis said of participating in the swim event. “He grew up around Lake Gaston and knew about the event.”
Carpenter sustained a spinal cord injury 17 years ago after diving into a swimming pool, but Callis became more acquainted with him while he was participating in outpatient aquatic therapy after he broke his femur while water skiing.

“I had observed him in outpatient therapy working on swimming and water safety skills to gain more strength and endurance,” Callis explained. After Carpenter was discharged from outpatient therapy, he continued to use the therapy pool and work with Callis to practice because he wanted to complete an open water swim. “This wasn’t a part of his therapy,” Callis said. “It was a personal goal, so I agreed to help him train to meet that goal. I wasn’t on the clock, but I chose to volunteer.”
Callis said her interest in aquatic therapy began after graduating from East Carolina University with a degree in recreational therapy, but she always loved the water.
“I grew up with a pool. I’m a water person. Most of my vacations are around the water,” Callis said.
During her first job after college, Callis took senior citizens to the local YMCA pool for exercise.
“I was not formally trained,” she admitted. “But I saw how free and happy the people were in the water and how they moved easier. I thought, ‘this is awesome.'”
From there, Callis found out about a water therapy conference in Washington, D.C. and her supervisor gave her the time off to attend. It was then she realized this was what she wanted to do. That confidence in her newfound passion led her to a job with ECU Health.
“I had a job but was looking to move back to Greenville,” Callis said. “I knew the hospital was building a pool facility and I asked the manager of the recreational therapy department what I needed to do to be eligible to apply for a job with them. He told me, and I went home and worked on those things. When it came time to apply for the job, I got it and I’ve been here ever since.”
That was in 1997, and Callis has been an essential player in ECU Health’s aquatic therapy.
“It was the right fit. I coordinate the aquatic therapy program and we’re fortunate to serve through the entire continuum of care, from acute to outpatient and community-based services,” Callis explained.
While she wasn’t initially looking to serve as an able-bodied swim partner in The Crossing, Callis said it’s been a good change of pace to her daily routine. This year, Callis agreed to be the able-bodied swim partner for an adult woman with cerebral palsy.
“Training her has challenged my problem-solving skills to help her be as independent as possible while improving her endurance,” Callis said. “When working with individuals with physical disabilities, the swim strokes are similar, but you have to adapt them to the diagnosis and the individual’s needs. I’ve had to figure out the logistics of things like getting my swim partner in and out of the lake, moving wheelchairs and coordinating volunteers. It’s fun because I’m training too!”

After last year’s success, this year, Callis helped coordinate five swimmers with physical disabilities to complete the event.
“With five swimmers, I needed help,” Callis said. She reached out to her team, and several were eager to help.
Kristin Jones, recreational therapist, Tasha Williams, clinical nurse specialist and Karen Pickles, physical therapist, also volunteered their time to help train and support the swimmers.
“Kristin and Karen were in the water to support the swimmers by paddle board and kayak, in addition to me,” Callis shared. “Tasha offered help with wheelchairs and transfers and cheered us on as we swam.”
That team support means a lot, but Callis said it’s not surprising that her colleagues jumped in to help.
“All of these swimmers except one have been our patients in some capacity over the years,” Callis explained. “It’s fulfilling to see a patient go from a new injury, when they’re at their most vulnerable, to having goals and flourishing. It’s nice to see it come full circle. These were once our patients, and now they’re our peers in the community.”
Callis added that while it’s rewarding the see a former patient thrive, she knows the value of them setting their own goals and putting in the work to reach them.
“The swimmers do this not because it was prescribed, but because it’s what they want to do,” she said.
Speaking about The Crossing after the event was completed, Callis said it was a huge success.
“All five swimmers completed their one-mile swim, and they were greeted on the other side by friends, family and their ECU Health family,” Callis said.
The date for next year’s event is already set, and Callis said that while she wants to help coordinate, she mostly wants to swim the one mile herself alongside the swimmers she’s helped train. In the meantime, Callis has other plans. Her next project is partnering with the city of Greenville to offer adaptive kayaking clinics. Whatever she does in the future, Callis said the work she’s done to support swimmers has been invaluable.
“It makes me happy,” she said. “It gives me such satisfaction, and reminds me that this is why I do what I do.”
Although Ellen Walston, the Injury Prevention Coordinator at the Eastern Carolina Injury Prevention Program (ECIPP) at ECU Health Medical Center, is no stranger to winning awards and giving presentations about injury prevention, she was no less thrilled to learn she was named the 2022 Safe Kids Coordinator of the Year.
“You’re nominated by your peers, and it’s a big deal,” she said of the award. “I’m blessed to be recognized.”
Walston has been with ECU Health for 31 years, the first 14 of which she served as an oncology social worker. Although she loved that role, she moved into injury prevention in 2006. ECU Health supports her in this role, but for every project she undertakes, she must seek external funding.
“If I want to do a water safety program, I have to write a grant,” Walston said. But, she added, the effort is worth it. “All of my work is to teach children and their parents about safety and to prevent unintentional injuries. My goal is to keep kids out of the hospital.”
Walston also serves as the Safe Kids Pitt County Coalition Coordinator.
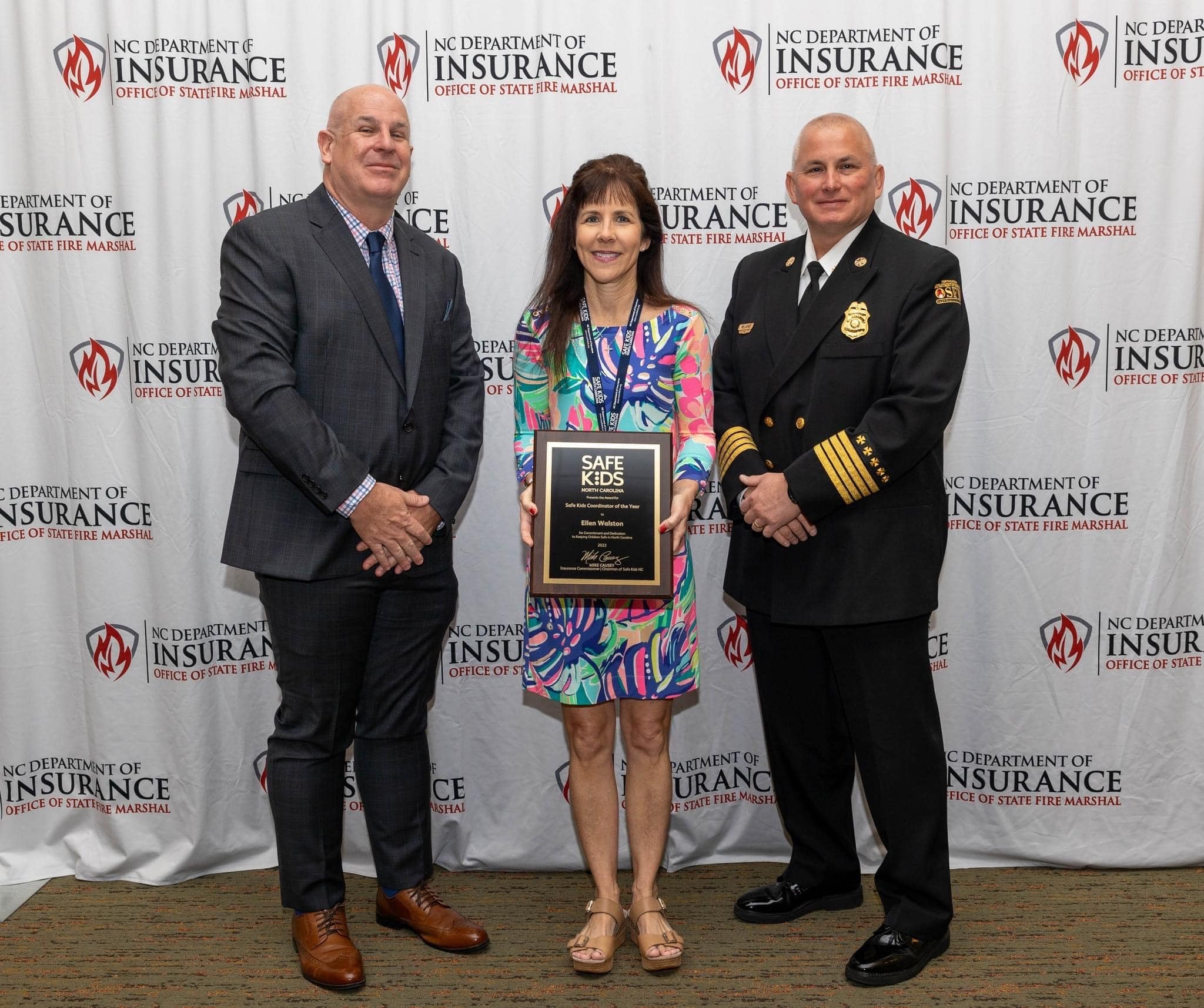
“We have 50 coalitions in North Carolina, and we’re part of a worldwide network of more than 300 coalitions,” Walston explained.
An award-winning career
The work she’s done in these roles hasn’t gone unnoticed. She also received the Safe Kids Coordinator of the Year Award in 2013, and the coalition won Coalition of the Year awards in 2010 and 2021: That’s four awards in 17 years.
These achievements wouldn’t be possible without partnerships, and Walston said she has friends all over the state and country to partner on projects.
“You have to share your successes and what you’ve learned, and give tools to others,” Walston said. “If you have something that works, share it. I never tell anyone no.”
One of those partnerships has been with the Greenville Traffic Safety Taskforce, which was created out of necessity when the then-Greenville police chief approached Walston and her manager, Sue Anne Pilgreen, with concerns about car crashes.
“In 2018, we were number one in the state for crashes in cities our size. The chief wanted a new way to prevent these crashes so we put together the taskforce,” Walston said. “I was thrilled he was so forward thinking.”
From there, Walston helped build a multidisciplinary team of high-level leaders, including the hospital police chief, the ECU Health vice president from design and construction, Greenville traffic safety engineers, the ECU police chief, NCDOT and the Greenville police traffic safety sergeant.
“We then became an official Vision Zero community, one of only 12 in the state,” Walston said.
Vision Zero’s goal is to eliminate all traffic fatalities and severe injuries by improving the roadway environment, policies and related systems. The taskforce quickly began environmental modifications, such as high visibility crosswalks, modular medians and delineator systems in center turn lanes, throughout the city. They are currently seeking federal funding to install a High-Intensity Activated CrossWalk (HAWK) to help pedestrians cross the street more safely.
The outcomes of this taskforce were seen immediately; “In 2020 we went from number one in the state for crashes to number seven, and in 2021 we were number eight,” Walston said. Because of their work, the taskforce won the 2019 North Carolina Governor’s Highway Safety Program Community Collaboration Award. In 2022, they won the Safe States Injury and Violence Prevention Achievement Award, and in 2023 they won the inaugural North Carolina Vision Zero Safety Award. Walston adds that another national award will be announced this year.
Sharing knowledge with others
Walston is eager to share her knowledge with others, and she’s done so through publications and conference presentations. She co-authored articles published in the November 2021 International Association of Chiefs of Police Journal and Exploring Perspectives – ECU Health Medical Center Journal, both addressing the evolution of Greenville’s Traffic Safety Taskforce.
She is also a veteran conference presenter.
“My husband says I go on my rock star tour,” she laughed when talking about her annual conference schedule.
This summer, she presented in Concord and Chapel Hill, North Carolina, and she’s slated to present in Washington, D.C.; New York City; and Denver, Colorado. The Washington, D.C. conference, the Safe Kids Worldwide Conference, is especially significant.
“That’s an international conference and I’m giving three presentations. It’s a big deal to break into that conference,” Walston said.
Walston said she loves to share knowledge to help others.
“It brings me great joy to bring positive attention to our hospital and community,” she said. “I want this work to be replicated everywhere, because we all have a mission to keep people safe.”
She also said what she learns at these conferences, she then applies to her work in here in eastern North Carolina.
“When I see something that works, I’m going to do whatever it takes to bring it to the community,” Walston said.
In addition to her passion for safety, Walston said implementing safety changes is a part of her legacy.
“There are mounted speed boards around school campuses in Greenville, for example,” Walston said. When I drive by one of those, I think I can’t wait to tell my grandchildren that I was instrumental in getting those put in place.”
Ultimately, Walston’s goal is to make Greenville, the surrounding communities and the state safer.
“It hurts my heart when there are preventable injuries, and I don’t want that for families,” she said. “I’ve been touched by severe injuries and deaths and I am always looking for ways to reduce risks.”
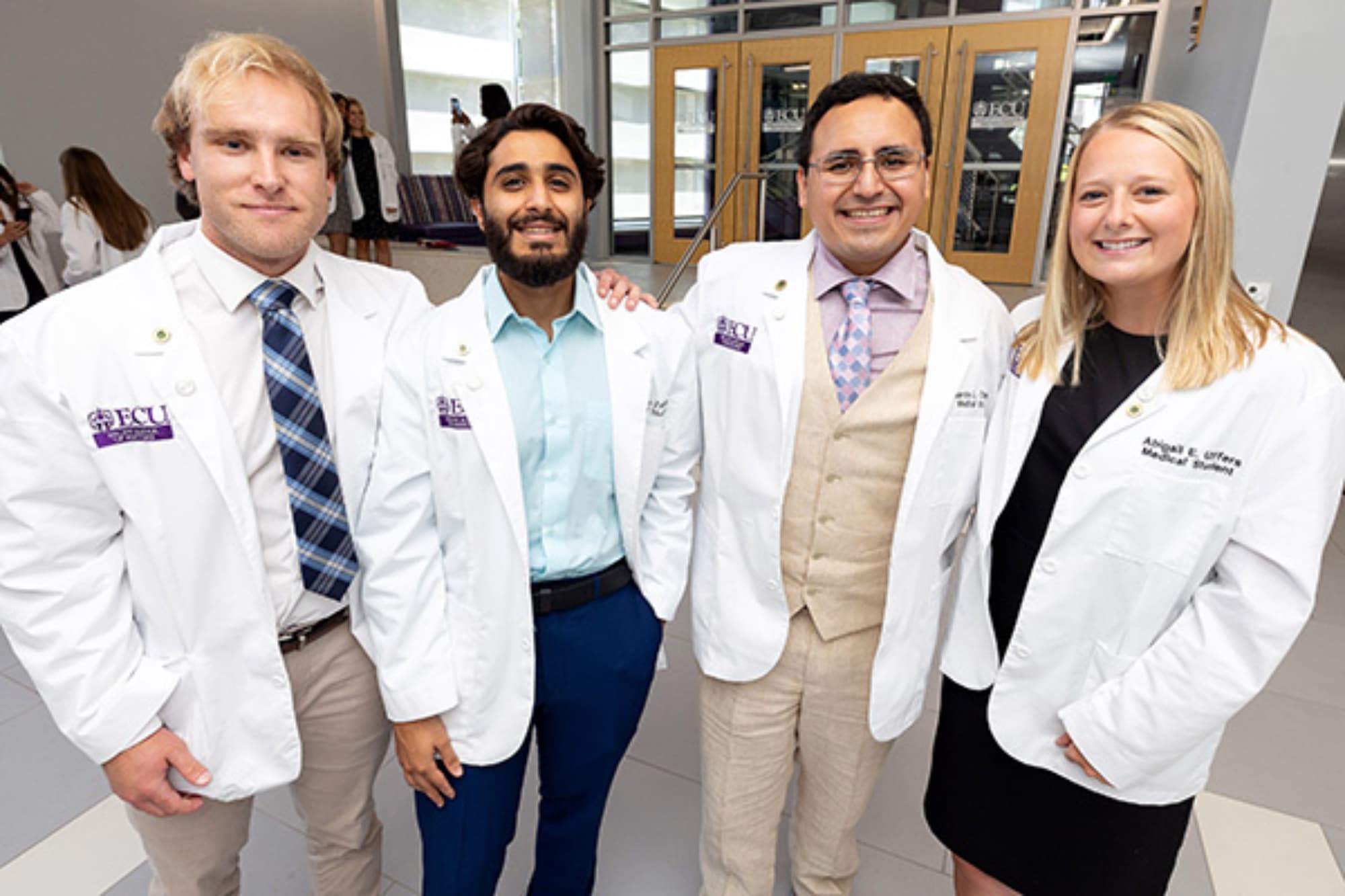
Lifelong dreams came one step closer to reality for the newest class of students in the Brody School of Medicine at East Carolina University as they were officially welcomed during the school’s annual White Coat Ceremony on Friday.
The 90 members of the Class of 2027 — all North Carolina residents — were helped into their white coats during the traditional celebration at the Health Sciences Student Center and regaled with messages and well wishes from Brody faculty and leadership.
Kristel McLawhorn, transplant nephrologist and 2005 Brody alumna, gave the keynote address, urging the Class of 2027 to stop, listen and absorb the knowledge and experiences they gain in the coming years.
“You have earned this opportunity,” McLawhorn said. “My charge to you is this: Be prepared for anything: to be challenged, to be afraid, to be humbled, to serve and to change. Know where your support is and know what is mission-critical in the big picture. Have the grace and wisdom to know when you don’t know, and the drive to do something about it.”
McLawhorn told the students that during her intern year at Brown University after she graduated from Brody, she got an early-morning phone call that her father was gravely ill. Knowing what she did about medicine, she jumped in her car and drove 700 miles south, knowing the odds were stacked against her father. But with her medical knowledge, she held out hope.
“My dad survived that event,” she shared, “and is actually sitting here with us today. Can you stand up?”
The crowd cheered and applauded as McLawhorn’s father, John Jernigan, stood and waved from the first row.
“I was clinically sound before; I left ECU with a strong base of medical knowledge, and I was working hard to hone and craft my skill at Brown,” she said. “But his illness taught me a great deal about life and even more about doctoring that no institution can teach you,” including empathy, ability to listen, sharpened knowledge and agile teamwork.
“My dad taught me that every day is a good day, and some days are better days,” McLawhorn said. “Today is one of the better days. It’s a marker in your life and education, a point at which you are living the consequences of your previous choices. You’ve worked hard for the opportunity.”
The Class of 2027, the largest class in Brody history, hails from 36 North Carolina counties and 26 undergraduate institutions; 61% of the class is female, 16% are first-generation college students, and 21% are from minority groups — Black, Native American and Hispanic or Latino — that the Association of American Medical Colleges considers “underrepresented in medicine.” Four are veterans, and four were collegiate student athletes. The class speaks a total of 23 languages.
Jason Higginson, executive dean of Brody, formally welcomed the class and voiced confidence in the students’ future contributions to medicine.
“Today we welcome you to the study and art of medicine, a profession symbolized by the white coat,” he said. “We know you will do great things.”
Onolunosen Abhulimen
Onolunosen Abhulimen — her family and friends call her Ono — doesn’t have time to wait for things to happen.
The Brinkley-Lane and early assurance student, the daughter of Nigerian immigrants, graduated from high school in Winston-Salem with an associate’s degree under her belt — the first in her school to do so. Since she pioneered the path, other family members have followed in her wake, including her two younger brothers, who are also Brody Early Assurance students — one a sophomore and the other a junior. Her youngest brother will start fourth grade in the fall of 2023.
Abhulimen played basketball on her school team and a travel team. She did the same with track, where she ran the short distances. That wasn’t enough, though. She picked up the shot put and then the discus, which she fell in love with and would have broken the school record had the COVID-19 pandemic not shut sports down.
She excelled in the classroom as well. Having to navigate traditional high school classes, driving to the community college, and juggling sports and clubs taught her life lessons that would set her up for success in college: discipline, organization and commitment.
“It was hard for me to seek help, to ask for advice. There were some barriers that had to overcome,” Abhulimen said. “I definitely had to learn time management.”

During high school she knew she wanted to pursue some kind of medical career. She attended a medical student symposium at Wake Forest University and heard a presenter talk about health care disparities, which was a new concept for her. Investigation and research solidified her plans — she wanted to be a doctor, enough so that during her undergrad years at ECU she founded a Students for Equitable Health Outcomes organization.
“I want a leadership role, to use my experience in helping those in rural communities get better health outcomes,” Abhulimen said.
Because she graduated high school with a pocketful of college credits, she was able to graduate from ECU summa cum laude in December 2022 with a degree in biology with honors in five semesters. She’ll start her first year of medical school at 21— most of her peers who will be a few years older — and after a semester’s break that she used to get her head in the game.
“I wanted to make sure I was really prepared and I was familiar with people that I could seek help and advice from. Brody is a very welcoming environment where it’s easy to ask for help or advice from other students,” Abhulimen said.
When she donned the white coat for the first time it was with pride and a sense of accomplishment. And her family beamed from the audience — her parents, all three brothers and a slew of aunts, uncles and cousins.
“It’s a representation of everything I’ve had to do to get to this point, even before high school. All the sacrifices that I made, being able to really study for those hard classes, some of the all-nighters I had to pull — I’m finally here,” Abhulimen said. “It’s like a breath of fresh air. I’m starting a new journey.”
Jose Robles Arvizu
Learning to navigate opportunity has given one first-year medical student a layered perspective from which to change the lives of his future patients.
Jose Robles Arvizu was born in Rio Verde San Luis Potosi, Mexico, and moved to Hendersonville when he was 2 years old. Over the years, he observed the challenges facing those around him and started formulating plans to make improvements in his community.

“Growing up, I saw how people in my marginalized communities, particularly farm workers and migrant farm workers, were often spectators in their health needs as a result of their lifestyle and barriers to accessing health care,” Robles Arvizu said. “I knew there had to be something I could do to bridge this gap and empower these communities to become stake holders in their health and make it a priority. This fueled my desire to become a physician with the goal of returning to western North Carolina to make a positive impact in the communities in the place I call home.”
He later attended UNC–Chapel Hill as a first-generation undergraduate, then went to Wake Forest to get his master’s in biomedical sciences, research track.
“One of the things that I am most excited about is being part of the incoming Brody class is becoming a member of a larger family that has a common goal of improving the health of communities across North Carolina,” he said. “Even within the last few days getting to know more people, it is more evident that we all have a ton in common, and I’m excited to embark on this journey with the rest of my classmates.”
Robles Arvizu has come to view education as a lifelong opportunity that can benefit those around him, making health care — and education — more accessible.
“Being a first-generation college and medical student brings both challenges and opportunities,” he said. “I would aim to use my experience as a first-generation student to advocate for others in similar situations. Understanding the unique challenges faced by first-generation students, I could contribute to making the education system more inclusive and accessible.”
Because of his motivation and perseverance, Robles Arvizu was named a Gates Millennium Scholar. The program, funded by the Bill and Melinda Gates Foundation, provides a full scholarship to any undergraduate institution to students from underrepresented groups. The scholarship also covers master’s and doctoral studies in the disciplines of computer science, education, engineering, library science, mathematics public health, and the sciences, where these groups are severely underrepresented.
“Being named a recipient of the Gates Millennium Scholarship one of the largest blessings that allowed me to peruse my dream of becoming a physician without the immense financial barrier that many first-gen students encounter,” he said.
As he begins medical school, Robles Arvizu plans to use his life experiences to be empathetic to his future patients’ barriers and circumstances.
“Having faced my own challenges and adversities, I would use these experiences to relate to my patients and their struggles,” he said. “This empathy would help me provide better care and make a positive impact on my patients’ lives.”
Grant Irons
The Class of 2027 includes a student whose family has already built a legacy in eastern North Carolina health care.
Grant Irons is the great-grandson of regional health care pioneers Fred and Malene Irons and the grandson of Tom Irons, professor emeritus of pediatrics at Brody, medical director of Access East and the N.C. Agromedicine Institute, and interim medical director of physician assistant studies.
Grant Irons was born and raised in Greenville and attended UNC–Chapel Hill, where he earned a degree in biology with minors in chemistry and health and society.
“It is truly humbling to carry on my family’s legacy here in eastern North Carolina,” he said. “I was lucky enough to spend time with my great-grandparents, Drs. Fred and Malene Irons. As I’ve grown up, I continue to learn more about their work and the impact they had on health infrastructure in eastern North Carolina. Their legacy demonstrates the impact of servant leadership. My late grandmother and grandfather, better known as Carol Irons and Dr. Tom Irons, continued this tradition of selfless service. I would not be the man I am today without their guidance as I aim to hold myself to their standard; a life lived with compassion, and humility.”

Tom Irons said he could not be prouder of his grandson’s desire to serve as a physician.
“I’m Grant’s only living grandparent, but I like to believe that today the other three are wearing smiles as big as mine,” he said. “His parents and I could not be more grateful that he has been given this opportunity, or prouder that he has chosen to come to Brody and eastern North Carolina.”
He added that he encourages his grandson and Grant’s classmates to follow their hearts.
“There is nothing easy about this journey you have undertaken, but if you put your heart into it, the rewards will be immeasurable,” he said. “Keep your head down these first two years, lean on each other, ask for help when you need it and never forget that there is no life more noble than a life of service.”
Grant is eager to live out a legacy and mirror his grandfather’s ideals and impact in medicine — but he is also ready to make his own name through the medical school that represents a life goal.
“The opportunity to be a student at Brody means the world to me; it has been a dream of mine for some time,” he said.
Grant Irons sees the bigger picture of eastern North Carolina’s health care landscape and also plans to make a difference through policy.
“Regardless of my career path, I have long been interested in health policy,” he said. “Initially, I was exposed to the importance of institutions through my family. Since I was old enough to understand, I have been fortunate enough to learn about care disparities and their impact on health outcomes.”
As a student at UNC-Chapel Hill, Irons explored the relationship between power, policy and differential health outcomes. He helped lead a chapter of PIH-Engage, a global health organization dedicated to building sustainable health infrastructure. That experience has led him to lead on a variety of fronts.
“As a physician I want to be more than a care provider; I hope to be a leader in my community,” he said. “While significant progress has and continues to be made, care expansion efforts are far from over. There are far too many people still in need.”
Lachlan Younce
Something about home — both places and people — helps to decide our futures for us.
Lachlan Younce is about as eastern North Carolina as a guy could get. His father’s family is from Belhaven and his mother’s is from Vanceboro. He played football and lacrosse at J.H. Rose high school in Greenville. He was a sailing counselor at a YMCA camp in Arapahoe, on the Neuse River, which will become important to his story.
At the camp he made friends with another counselor, a young man who ran a lot and worked out. Younce asked his friend why he was so fanatical. The answer — he was getting ready for the U.S. Naval Academy. Younce isn’t from a military family and had no idea what that meant but got very interested.
Younce applied for an appointment to the Academy and received one from the late Representative Walter B. Jones, who Younce recalls fondly. His initial attempt to get into Annapolis didn’t work out, so after graduation he headed west to Raleigh where he was part of the ROTC program at N.C. State, which he said was a blessing because he learned about military culture, which was completely foreign.
The next year his fortune changed and the Navy accepted him as a Midshipman.
Like many young men entering the academy, Younce wanted to be a pilot. He had his mind on studying political science; instead he took his first physics class, majored in chemistry and applied to the medical corps track.
He graduated in May 2023 as an ensign, and the Navy told him he could apply to any medical school in the country. He applied to three, but there was only one he really wanted to receive an acceptance letter from.
“I had the best interview experience here at Brody, I just felt like I was at home. This community raised me, built me and I think that learning medicine here is going to be extremely rewarding,” Younce said.
He’s not completely sure about what specialization he might pursue after graduation, but Brody’s mission of educating the next generations of primary care physicians impresses him.
“I think it’s great that a school so oriented towards primary care can train a physician to go into the military and provide care that service members need,” Younce said.
The winding route that brought him home means more than just place. Health care is a thread that is beginning to be woven into the fabric of his family. His mother is a registered nurse with ECU Health and a proud Pirate Nurse. His sister, Fallon Younce, has a year and a half until she graduates from the College of Nursing as a Pirate nurse herself.
“We’re going to be able to overlap these two years, and one thing I’ve learned is that nurses know what’s going on, so I’m going to use nurses’ knowledge to be successful,” Younce said.
After graduation, he’ll owe the Navy a number of years as an active-duty Navy doctor, which he is excited for, but is ultimately unsure about a career in uniform. Regardless of when is his time in uniform ends, he’s sure he’ll return to eastern North Carolina to use his Brody training to improve access to health care in underserved areas.
Family, service, and leadership were key themes of Dr. Jason Higginson’s presentation to nearly 100 first year ECU Brody School of Medicine students at the 15th Annual José G. Albernaz Golden Apple Distinguished Lecture Thursday, July 27 at the East Carolina Heart Institute at ECU.
Funded by the Albernaz family in partnership with the ECU Health Foundation, this lecture was established in 2006 with the goal of providing support for physicians to share their expertise with the medical education community. In a presentation titled “Learning to Lead: Lessons from My Military Life and Beyond,” Dr. Higginson, executive dean of Brody and chief health officer at ECU Health, outlined how his experience in the U.S. Navy, alongside the lessons he learned from his family, mentors and patients, has shaped his journey as a leader and medical doctor.
“Leadership is about finding what you do best and using that to help the people around you,” Dr. Higginson said. “You cannot achieve anything in life without the people around you. A good leader finds a way to use their knowledge and skills to solve problems for others.”

Dr. Higginson has been at Brody since 2012, following 13 years of active duty in the U.S. Navy, where he now continues to serve in the U.S. Navy Reserve holding the rank of captain. His previous roles include chair of Brody’s Department of Pediatrics, Pediatrician-in-Chief of Maynard Children’s Hospital, chief of neonatology and medical director for the Neonatal Intensive Care Unit and Newborn Medicine.
“Being a medical doctor is not about self, it’s about a calling to serve a higher need,” ECU Health CEO and Brody Dean Dr. Michael Waldrum said in his introduction at the lecture, “Dr. Higginson is a shining example of that. He is a highly engaged and highly purposeful leader who is helping us build something special at ECU Health. We’re excited that you, our students, have an opportunity to learn from him today.”
Despite his prestigious rank in both the military and the clinical field, Dr. Higginson said the lessons learned early on taught him the skills he needed to successfully lead others. He recalled joining the Navy shortly after getting his medical degree and being told to master the skills of a broom as he swept floors during his first week. That experience taught him that everything, even the simplest tasks, matters in the organization.
Those lessons, Dr. Higginson said, will serve Brody’s newest cohort of students as they embark on their own personal journeys through medical school.
“All of you are going to stand up and take the oath to be a doctor,” Dr. Higginson said. “As you are reading the words for the first time in front of those you love, I encourage you to pause and reflect on the words and what they mean to you. If you take that oath seriously, you will succeed.”

ECU Health Chief Executive Officer and Brody School of Medicine at East Carolina University Dean Dr. Michael Waldrum recently joined the Raise the Line Podcast to discuss rural health care, his personal journey in medicine and how ECU Health and Brody are advancing the shared mission of improving the health and well-being of eastern North Carolina. Hosted by Osmosis from Elsevier, Raise the Line is a podcast about strengthening global health care systems through education, training and optimizing the workforce to support health care workers.
A passion for rural communities
During his time on the podcast, Dr. Waldrum talked about his background in medicine, from his decision to pursue a medical degree, to his clinical career as an intensivist in critical care medicine, and his robust experience in health system leadership roles. He credits his time growing up in Minnesota near the Mayo Clinic for his rural health care passion.

“As a young person being surrounded by physicians and other health care professionals in a rural community, it was just transformative for me. It was unbelievable,” said Dr. Waldrum. “I lived on Mayo Wood Road. I knew a number of the Mayo family, and to see what that organization did in this rural northern community in Minnesota was incredible. So, it just was something as a young person that I became very interested in because I could make a living taking care of people, which was just an unbelievable opportunity that I still have so much respect for and love for.”
Health care delivery through education
Dr. Waldrum said delivering health care in rural areas is a challenge ECU Health is uniquely positioned to solve, thanks in large part to the Brody School of Medicine, which is a leader in training primary care providers for the state. By training the next generation of providers, many of whom go on to practice in rural communities, the educational component is as important as the health care delivery component.
“I like complex problems,” Dr. Waldrum said. “I like working on these systemic complex issues and so that’s what led me to come to eastern North Carolina. We cover a geographic area the size of Maryland. People aren’t really familiar with the coastal plains of North Carolina, but it’s a huge geography and our organization serves this large geography and is really the safety net anchor institution across this region. Part of that is the academic component, which is the Brody School of Medicine, a great organization whose mission was created to primarily educate primary care physicians to take care of North Carolinians, to improve the health and well-being of this region, and to offer medical education to diverse populations.”
The Brody class of 2023 is a snapshot of Brody’s mission to serve North Carolina by increasing the number of primary care physicians who serve the state. Fifty-two% of the 2023 Brody class matched into primary care residencies — including obstetrics and gynecology — and 44% matched to residency programs in North Carolina. What’s more, Brody’s most recent class features the most medical students who will begin their residency at ECU Health Medical Center in July, which is no coincidence, according to Dr. Waldrum.
“As for ECU Health and Brody School of Medicine, we are creating the model for rural health care by creating a trusted premier education and health care organization that’s a regional-based delivery system and education system,” said Dr. Waldrum. “We have a great team of professionals doing that — multidisciplinary teams. Anybody that wants to join us — that wants to be creating a future for a great region that’s beautiful in eastern North Carolina — if you can get behind that mission, we welcome you because we are in the process of transforming health care for rural America to become that model.”
Looking for more?
Find and listen to the Raise the Line Podcast, Episode 398 – Creating a Model for Healthcare in Rural America wherever you get your podcasts.