While Heather Duncan, the director of ECU Health Medical Center’s laboratory services, knew she wanted to work in health care from an early age, her career plans changed when she learned about the medical technologist program at her school. “I thought I’d be a dermatologist,” she recalled. “But I liked biology and science, and the medical tech program fit my interests. That steered my career, and I’ve never looked back.” The South Carolina native has served in her current role at ECU Health for six years, and she is now wrapping up her four-year term with the Clinical Laboratory Improvement Advisory Committee (CLIAC), which is an appointed position. During her time with CLIAC, Duncan has been instrumental in bringing positive change to her profession.
CLIAC is a federal advisory committee that provides guidance to the Department of Health and Human Services (HHS) and is managed by the Centers for Disease Control and Prevention (CDC). The advice and guidance the committee provides pertains to general issues related to improvement in clinical laboratory quality and laboratory medicine practice.
Duncan said she didn’t even know CLIAC existed until a former co-worker approached her to gauge her interest in being nominated for a position. “They asked me if I would be interested, and it was exciting because CLIAC is so impactful.”
In the past four years, Duncan said she’s been privileged to collaborate with 20 other professionals to develop educational resources for the lab community and update the CLIA regulations. During her tenure, Duncan chaired the CLIAC Certificate of Waiver (CoW) and Provider-performed Microscopy (PPM) Procedures workgroups.

“The work that has come out of those groups has allowed CLIAC to make recommendations to modernize our regulations, which impact the laboratory community at large. We’ll see those impacts here at ECU Health,” Duncan said.
One such regulation restricts who is allowed to train new personnel to perform certain functions in the lab. With Duncan’s work, the regulation has now expanded to allow more people in the lab community to perform that training. “Because there is such a workforce shortage with laboratory technicians, this is impactful by expanding who can provide training, and it improves the overall quality of lab testing,” Duncan said. Caryl Havasy, the system administrator for laboratory services, sees Duncan’s work with CLIAC as instrumental in gaining more lab technicians. “ECU Health, like other health systems, faces an ongoing shortage of laboratory testing personnel. Heather’s experience in laboratory operations and regulatory compliance in our rural-focused health system brings a much-needed perspective to the work of CLIAC, specifically its role in creating the regulatory structure that defines the qualifications for frontline laboratory roles,” Havasy said.
Another exciting recommendation that emerged from the most recent CLIAC meeting would allow for virtual competencies, which would expand training capability and incorporate cutting edge technology into practice. “Because we serve rural communities, having this technology would cover a huge network,” Duncan shared. “We have benefitted from having a direct pipeline to the work CLIAC is doing. For example, our lab was one of the initial beta testers for virtual lab safety training. They sent us four Oculus headsets and they push new training programs to us.”
While this technology isn’t widely used yet, Duncan said being a part of an organization that promotes advancements in technology and makes recommendations on a federal level is gratifying. “This work allows for a forward-thinking process, and it will impact our whole community,” she said. “Our vision is to be the national model for rural health care, so we should use every tool available. Being a part of CLIAC means I’ve been able to make a real difference.”
Havasy highlighted other areas CLIAC and Duncan’s work with the committee makes an impact, including, “a change to rules surrounding histocompatibility testing (performed to match organ donors with recipients, i.e., kidney transplants) that will remove specific requirements for obsolete methods and practices, accept newer testing techniques and eliminate redundant requirements. This will result in a decreased compliance burden on the laboratory and more efficient testing for our eastern NC kidney transplant patients.” Duncan also worked with the CoW workgroup, which addresses regulations as they pertain to labs with a Certificate of Waiver. This waiver is granted to labs that only perform waived tests, which are simple laboratory procedures and examinations with a low risk of an incorrect result (including urine pregnancy tests or blood glucose monitoring). Labs must pay certification fees every two years to acquire and maintain the certificate. Duncan explained that one area her workgroup focused on was an updated fee schedule. “CLIA is a self-funded program, and they haven’t updated their fees in a long time,” Duncan explained. The group also worked on establishing a broader range of sanctions for laboratories that operate under a Certificate of Waiver but are not compliant with the CLIA regulations.
Because of her work with CLIAC, Duncan said ECU Health has a seat at the table and can provide input for advancements in laboratory operations. “Through these efforts,” Havasy added, “Heather embodies the ECU Health vision of bringing our rural health care system needs and potential solutions to a national stage, impacting not only our own operations but those of every health care system across the country.”
Across the ECU Health system, hospitals recognized Veterans Day with events honoring those who have served our nation and thanking those who have chosen to serve in a new way at ECU Health.
At ECU Health Medical Center in Greenville, team members gathered around the flagpole just after 9 a.m. to come together, connect with other veterans, and appreciate one another’s service to the country and eastern North Carolina.
Dr. Virginia Hardy, vice president and chief inclusion and belonging officer at ECU Health, hosted the event and welcomed in team members.
“Today, we celebrate not only your past service, but also your legacy of courage and honor,” she said. “Our veterans remind us that our freedom is not just a right, it is a responsibility. Freedom today means different perspectives, engaging and constructive dialogue and ensuring that every voice has been heard.”

Cameron Graham, manager of electrical and mechanical systems in Plant Operations at ECU Health, gave a roll call for each branch of the United States military with veterans responding with their branch battle cry.
He shared that his service in the Navy helped shape his perspective as a leader and in his daily work at ECU Health.
“My brother was in the service, also in the Navy, and he was kind of my hero, so I followed his tracks,” Graham said. “When I attained the rank of Chief, we used to do what was called an initiation. You’re taught humility, to never forget from whence you came, and those who made you who you are. That has served me well, not only in the military but at ECU Health as well.”
Wayne Waters, a mechanic with Plant Operations at ECU Health, led the Pledge of Allegiance during the event. He served in the National Guard and said he took lessons from his time in the service that he sees in his work each day at ECU Health.
“A lot of my family in the past had been military, so growing up it was just the right thing to do. I’m just proud to be a part of the service,” Waters said. “Being young and going in, it helped me with structure in my life. It really taught me to be team player, being part of a team and working together.”
Trish Baise, chief nursing executive at ECU Health, said as the daughter of a veteran, she’s proud to participate in these events and recognize others for their service and sacrifice.
She said the sense of service in those who serve in the military does not fade and we see that each day in eastern North Carolina and at ECU Health.
“Our neighbors, friends and family members who have served often return home to continue their legacy of services,” Baise said. “They become teachers, first responders, health care professionals and community leaders. The sense of commitment is part of what makes eastern North Carolina unique – a place where selflessness and service are not just values, but a way of life.”
At ECU Health, we’re grateful today and every day for the service of our veterans. We’re proud of the more than 550 ECU Health team members and 60 medical students, faculty and staff at the Brody School of Medicine who have decided to continue their service to others after their time in the military.



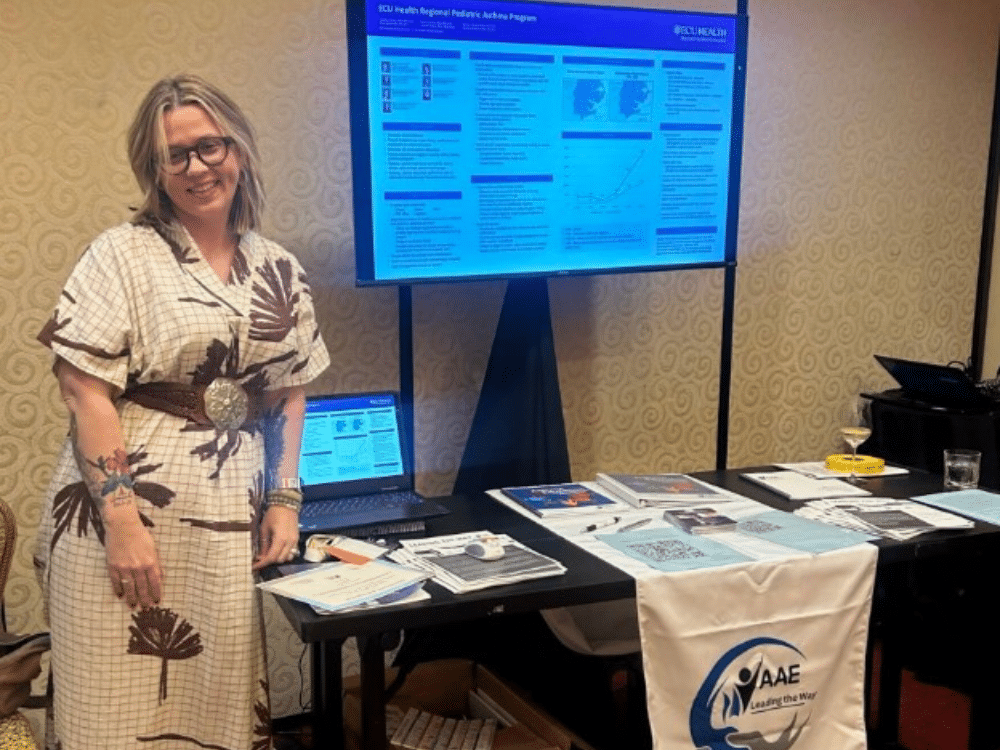
Candace Cahoon, the respiratory care manager for the Pediatric Asthma Program, presented in July at the National Association of Asthma Educators (AAE) annual conference in Charlotte, North Carolina. The AAE is dedicated to providing quality education to a multidisciplinary group of asthma educators, and members include respiratory therapists, nurses, pharmacists, physicians, social workers, nurse practitioners and others. Cahoon’s presentation is one way the Pediatric Asthma Program at Maynard Children’s Hospital strives to share its research, lessons learned and processes for establishing a national model for a pediatric asthma program in the United States.
Cahoon has worked with ECU Health for 10 years, and during that time she has continued her education from a bachelor’s degree in sociology and an associate’s degree in respiratory therapy, to a master’s in health education and several certifications.
The Pediatric Asthma Program, which has grown from serving two counties in 1995 to 29 counties today, aims to reduce emergency department and inpatient admissions for children with asthma, decrease school absenteeism and increase the quality of life for children with asthma in eastern North Carolina. It does this by offering asthma testing, asthma education, tools to manage asthma, access to community resources and medication assistance. Their work with eastern North Carolina public schools has been a particularly effective way to reach children in rural North Carolina communities.
The poster Cahoon presented was the collaborative work of the Pediatric Asthma Program’s entire team, and the goal was to educate others on how to establish and support a pediatric asthma program. “We’re one of the best programs in the nation,” Cahoon said. “We are ahead of the game in terms of what we address for our patients with asthma. I go to conferences and say, ‘we know this; we do this,’ so we are well-known in the state and nationally.” Sue Anne Pilgreen, the manager of the Pediatric Asthma Program, said Cahoon is the “teacher” of their team. “She is a lifelong learner,” she said. “While the content development was a team effort, Candace pulled it all together, submitted the abstract and ultimately showcased our great work.”
Cahoon shared that the Pediatric Asthma Program is now establishing its own professional conference: Pediatric Asthma Management: Providing Holistic Care to Rural Communities. The conference is scheduled for February 28, 2025 and will be held at the Eastern Area Health Education Center, with virtual and in-person capability. Cahoon leads the committee responsible for making the conference a reality. “We want to show how we are touching every single aspect of an asthmatic patient’s life,” Cahoon said. “We have worked to expand and grow our program over the past few years, and we’ve had countless people ask us how we ‘found’ our success, especially in such a rural area,” Pilgreen added. In answer to that, the conference will address key components involved in implementing a comprehensive asthma program, while also discussing the clinical components of how the asthma team treats patients with asthma and helps them transition to home. “We’ll have a case study that goes through the hospital or clinic and has a breakdown of testing, education, home visits and environmental assessments for the patients,” Cahoon shared. The team will also talk about Single Maintenance and Reliever Therapy (SMART) as a new treatment option for patients with asthma that combines in a single inhaler both a corticosteroid and a long-acting beta-agonist so it can be used as a daily maintenance and as-needed relief of asthma symptoms. “The overarching objective for the conference is to help participants to utilize clinical knowledge, skills and expertise to provide holistic pediatric asthma care in the community,” Pilgreen said. “We know this starts in multiple places, including the hospital bedside, schools, and primary care provider offices.”
Ultimately, attending conferences, as well as establishing a conference of their own, highlights and shares the innovative work of the Pediatric Asthma Program at Maynard Children’s Hospital. “It shows that we’re here and we can do this together,” Cahoon said. “We are more than willing to show how over the last 20 years we have put this program in place.” Pilgreen agreed: “The design of our program is unique. Having the opportunity to present our program model and outcomes at a national conference not only elevates our work, but it also gives others the tools to replicate our model in their area. Our goal is to increase the quality of life for children with asthma, regardless of where they live.”
In celebration of the season, Maynard Children’s Hospital patients, families and team members had a chance to recognize Halloween and bring a sense of normalcy around the day.
Team members from across ECU Health and some community groups came together inside the children’s hospital to dress up and let the children see some of their favorite characters, like Mario, Woody and Buzz from Toy Story, and everyone from Inside Out.
Some tables set up inside Maynard Children’s Hospital even offered interactive games for the kids to play while they were picking up goodies from each team. Those involved said this is one of the most special events of the year, where teams can share a bit of normalcy with the youngest patients at ECU Health Medical Center.
Amanda Jones, a child life specialist at Maynard Children’s Hospital, said she’s grateful to work with a team whose role is to put a smile on children’s faces.
“That’s part of our role here, we try to bring some fun to Maynard Children’s Hospital,” Jones said. “Kids and their families have to be here, so we just try to celebrate holidays, celebrate milestones and bring some of their home to them while they’re in the hospital.”
Jones said while the event takes a lot of planning and organizing, the team member engagement makes it easy to pull together and generate excitement. After four years of hosting a parade outside of Maynard Children’s Hospital, the event moved back indoors this year for a more interactive experience for patients and families.

One of those patients was Aleksandra, who was dressed as Belle from Beauty and the Beast during the event. She said it made her day to see the Minecraft booth set up from one of the teams.
“It was fun to go trick-or-treating and see all the booths. There were so many different booths, it was just really fun,” she said. “Being able to do this with other people, who some of them might have the same condition as me, that was a good memory.”

Her mother, Lydia, said she was grateful for her daughter to have something to look forward to for Halloween while she’s in the hospital. For herself, Lydia said it was nice to see Aleksandra and so many other children light up as they went through the different booths.
“It’s wonderful that they put on an event like this so that all of the children who are missing out on Halloween get this experience,” Lydia said. “I love seeing them have the moment of just being a kid, wearing a costume and forgetting for a day that they’re in the hospital.”
Lydia said she had a great time watching her daughter, other patients and even parents interacting with an Inside Out booth, complete with a replica console from the movie.
Tara Stroud, vice president of Women’s and Children Services, said team members step up in many ways to be there for the patients and families served at Maynard Children’s Hospital and this event is a true example of that commitment.
“There’s something about being able to work in a children’s hospital and really give the child the experience of being a child, whether they’re sick or not,” she said. “It gives a heartwarming feeling to the team to know that we’re going to make a difference – whether it’s caring for them medically or it’s just putting a smile on their face.”



There were plenty of smiles and handshakes at the Teachers of Quality Academy (TQA) 7.0 Recognition Ceremony on Sept. 30, as 37 graduates from the most recent TQA cohort celebrated successful completion of the program alongside ECU Health and Brody School of Medicine leaders.
TQA is a professional development program for health care leaders designed to fundamentally change care delivery through a curriculum focused on building knowledge and skills in Health Systems Science which comprehensively explores how health care is delivered. Participants engage in advanced learning in quality improvement, patient safety and team leadership, develop improvement projects to apply these skills across the health system, teach others in their environment about these concepts and evaluate the outcomes of improvement interventions. Leading by example, TQA participants promote a culture of quality and safety across the enterprise.

This year’s program graduates came from multiple areas of expertise and locations, including ECU Health Physicians, ECU Health Medical Center, ECU Health North Hospital, ECU Health Chowan Hospital and Contentnea Health. Additionally, the cohort includes participants from ECU Health’s Rural Family Medicine Residency Program, ECU Health’s Administrative Fellowship Program and the MedServ Fellowship Program.
“As an academic health care organization, it’s incredibly gratifying to see educational programming like TQA woven into ECU Health and Brody’s culture of quality improvement,” said Dr. Michael Waldrum, ECU Health CEO and dean of Brody. “You can see and feel the pride that people take in improving quality, and that has real tangible impacts on patients who can experience better health and wellness as a result. This cohort and these graduates are an example of our quality improvement culture which TQA has helped build.”
According to Dr. Jennifer Sutter, TQA physician director, the diverse, multidisciplinary class represented the ultimate goal of the program: to further knowledge and instill principles that help health care professionals across eastern North Carolina improve quality on behalf of the patients they serve.

“It is exciting for us as program leaders recognize and celebrate these dedicated health care professionals for successfully completing TQA,” Sutter said. “Those of us involved in the program have been fortunate to witness incredible growth from our 7.0 cohort. We could not be more proud of what they’ve accomplished and how they will use their knowledge and skills to help further high-quality care in their individual clinical setting through out eastern North Carolina.”
The seventh iteration of the program was comprised of 12 half-day sessions alternating concepts of leadership development and new competencies of Health Systems Science, including patient safety, quality improvement, systems thinking, population health and team-based care. Each learning session also emphasized wellness topics enabling participants to engage in supplemental activities to further enhance the experience of life while at work. The year-long program culminated in each participant completing a comprehensive quality improvement project in their area of focus.
“As part of TQA, I had the honor of partnering with leaders from our community hospitals—North, Chowan, and the Medical Center—all of whom shared a commitment to serving our community,” said ECU Health administrative fellow Madison Stevens, a member of the 7.0 cohort. “The sessions empowered us to explore and refine our leadership philosophies, building a strong foundation rooted in quality improvement, professional growth, and innovation. The program has equipped me with the tools to become an effective and open-minded leader. In our project, my team focused on post-event debriefing in the emergency department, prioritizing the well-being of our team members alongside clinical learning to help teams navigate high-stress situations and improve patient care outcomes. We look forward to sharing our results and broadening our focus on quality improvement to provide exceptional patient care.”
The TQA curriculum is also designed around experiences that span the continuum of care in multiple areas of clinical focus which enables participants to be better prepared to meet real-world challenges. This intentional design, according to ECU Health Chief Quality Officer and Chief Clinical Officer Dr. Niti Armistead, enables TQA graduates to immediately help drive quality improvements in the clinical environment.
“TQA is so important because it creates a community of interdisciplinary professionals committed to improving quality both here at ECU Health and beyond,” Dr. Armistead said. “Quality is a critical component of our quintuple aim and the work being done by TQA program leaders and participants directly ties to our ability to improve the health and well-being of the region. Through TQA, participants learn by doing and acquire collaborative problem resolution skills to drive continuous improvement.”
As recovery efforts continue following Hurricane Helene’s devastating impact in western North Carolina, team members from the east continue to do their part in support of those impacted.
The local efforts, led by the Eastern Healthcare Preparedness Coalition (EHPC) at ECU Health, include boots-on-the-ground contributions that started immediately after the storm hit the state and continue today in various capacities.
Chris Cieszko, Disaster Services Specialist with EHPC, was among the first group of team members to travel to western North Carolina in the Medical Ambulance Bus the day after Helene hit the western part of the state. Along with other members of EHPC, Cieszko said they helped with the immediate response which included logistical support during the staging period such as changing batteries, loading trailers and “a little bit of everything” to help manage supplies.

Using the medical bus, the team partnered with Lumberton Rescue Squad and assisted with the local EMS response from Linville-Central Rescue Squad to help evacuate 23 patients from a damaged assisted living facility in Grandfather Mountain to a safer location away from the impacted area.
“It was obviously a difficult situation given the conditions and circumstances,” Cieszko said. “No one wants to leave the comfort of their own living space. We were able to talk to them, take care of them and ultimately get them to a safe location. The entire response was a true testament to the teamwork between EHPC, Linville-Central Rescue Squad and of course our sister agencies in the North Carolina Healthcare Preparedness.”
The EHPC team also helped with technology and communication needs in the immediate aftermath of the storm, which is a vital asset to disaster response. Matthew McMahon, disaster services specialist with EHPC, helped connect a Starlink to the medical bus ensuring it had internet, and programmed helicopters to provide connectivity with ground support.
Recovery efforts have not stopped since Helene’s arrival, and neither has EHPC. Chris Starbuck, Healthcare Preparedness Coordinator with EHPC has been stationed in Raleigh at the North Carolina Department of Public Safety Emergency Operations Center. His role includes supporting health care staffing needs at all several operational sites managed by the state.
These needs, along with EHPC support, represent the importance readiness to respond to disasters immediately, while also being prepared to provide long-term help as recovery efforts continue.
“A huge outpouring of medical personnel from all over NC have volunteered to assist with the response efforts in the west,” Starbuck said. “Many are wondering ‘when’ they are going to get a chance to help. We can be ready for when the call comes. Have plans for your family, kids, and pets along with working with your employer so they can plan schedules.”
In March of 2021, Jalen Hill, MLT (ASCP)CM, joined ECU Health Beaufort Hospital as a cook in the Food and Nutrition Services department. “I wanted to go to culinary school,” he said. “But once I was at the hospital, I found out about a whole other world of opportunities.”
Those opportunities began with one conversation with Human Resources (HR). “Someone in HR heard me talk about wanting to do something different,” Jalen shared. “I wanted to be more involved and out in the field, doing patient care. I was considering going into radiology, and I thought I could train in phlebotomy and then transfer into a radiology program; but then the person in HR talked to me about the medical laboratory technician (MLT) role, which I had never even heard about. She was the one who set me up with the lab to do some job shadowing, and that was the spark.”
From there, Jalen entered the medical laboratory technician program at Beaufort County Community College in August of 2021, and at the same time, he also trained as a phlebotomist. In July 2023 he completed his phlebotomy training, and in May of 2024 he graduated with an associate degree in medical laboratory technology. That following June he began working at the hospital as an MLT.
Now Jalen truly enjoys his work and the chance to meet different people every day. “You are talking to people and hearing their stories every day. I’m drawing blood to help doctors, and I’m in the lab running tests to help get a diagnosis. That means a lot,” he said. He also values his co-workers, without whom he might not have found his true calling. “In this job, I’ve gained friendships and I’ve learned a lot. Andrea Latham and Sherry Langely were the ones who encouraged me to train as a phlebotomist and let me shadow in the lab. When I was in school, I still worked in the cafeteria, and they’d come by and ask how classes were going. They offered to help if I had any questions. I appreciated them checking up on me.”
The Washington, North Carolina native is now pursuing a bachelor’s degree in medical laboratory science at Winston-Salem State University, and he is already considering his future education and career options. “I’ve researched forensic science, but I’ve also looked into a master’s in business administration or a master’s in public health, where I could be an epidemiologist or toxicologist. It feels good to have these opportunities ahead of me,” he said.

To anyone considering making a career shift to health care, Jalen said go for it. “It’s a great decision. You have a direct influence on people’s lives every day. Every time you clock in, you are doing something that’s meaningful to someone, whether it’s a simple blood draw or talking to a nurse about lab test results. It’s a rewarding career.”
The Teachers of Quality Academy (TQA) at the Brody School of Medicine at East Carolina University and ECU Health officially welcomed its 8.0 cohort, comprised of a group of multidisciplinary health care professionals committed to quality improvement, leadership development and improved patient outcomes, at its first learning session on Sept. 19.
TQA 8.0 is a professional development program for health care leaders designed to fundamentally change care delivery through a curriculum focused on building knowledge and skills in Health Systems Science which comprehensively explores how health care is delivered. Participants engage in advanced learning in quality improvement, patient safety and team leadership, develop improvement projects to apply these skills across the health system, teach others in their environment about these concepts and evaluate the outcomes of improvement interventions. Leading by example, TQA participants promote a culture of quality and safety across the enterprise.

“Our goal is to help participants take the lessons they learn in TQA back to their clinical areas,” said Dr. Jennifer Sutter, TQA physician director. “It is important that we use this opportunity to equip and empower our leaders to be quality teachers for their colleagues and teammates in order to improve patient care across the system.”
With 36 learners in TQA 8.0, participants spent their first learning session gaining invaluable knowledge about quality, the role it plays in high quality care and the impact it has on ECU Health’s mission to improve the health and well-being of eastern North Carolina. The newest cohort includes health care professionals from clinical, administrative, leadership and educational backgrounds, all of whom were selected from a highly-competitive pool of applicants. The cohort is comprised primarily of ECU Health team members but also features, for the second time, participants from outside the health system.

In one of the main team-building activities during the first learning session, groups of participants worked together to build paper airplanes. The catch? The airplanes had to be built quickly and to exact specifications. The activity helped reinforce key themes that will be instrumental to the year-long TQA experience: communication, teamwork and focus on details. The lessons are all designed to help participants create a Quality Improvement Project at the end of the program.
“Their growth throughout the program is going to be tremendous,” said Dr. Amy Campbell, quality nurse specialist at ECU Health and one of the quality coaches. “The airplane project is a great example of what they’ll experience in TQA. At first it can be overwhelming, but it helps them problem solve and then apply those lessons to their quality projects. Learning that connection between quality and patient experience can help us all provide better care and reach for better outcomes.”
Eastern North Carolinians know all too well the devastation that accompanies major hurricanes. When Hurricane Helene hit our neighbors to the west, ECU Health and Eastern Healthcare Preparedness Coalition (EHPC) team members did not hesitate to answer the call. Since Friday, these specialized team members have been providing ongoing support to hospitals and health care facilities as they work to ensure patients can be safely cared for in the fallout of the catastrophic storm.
“Our folks are great. As soon as this happened, our disaster preparedness group started putting together what we have, how can we help and how we can get there,” said ECU Health Chief Operating Officer Brian Floyd. “One of the things I love about ECU Health is we are filled with people who just care. I could not be more proud of the collective response from our team members, including those who went as part of our organizational response, and those who are helping donate to recovery efforts.”
Across western North Carolina, more than 20 hospitals were impacted by the storm and thousands of people left devastated. Some are without water and power and others are in various phases of assessment and stabilizing operations. Beyond facility issues, hazards rendered the roads dangerous and, in some cases, unable to be used at all.

Through our EHPC, ECU Health is closely aligned with NC Emergency Management for daily coordination of hospital and patient care needs. In one example, the team directly supported the evacuation of 23 residents in a care facility and help relocated the individuals to a safer location using the Medical Ambulance Bus.
Stephanie Seals, disaster services specialist with EHPC, was among the first group of team members to deploy to western North Carolina. Within 24 hours, the team “pre-deployed” to the area carrying supplies, the ambulance bus and experts to help. The ECU Health team was among the first to arrive in the region in the early hours after the storm moved through.
Shortly after she arrived on-site in western North Carolina, Seals was tasked with an important job by the state: directing the Statewide Patient Coordination Team support cell. This support cell – which is vitally important given the outages impacting connectivity at hospitals and health care facilities – brings all transfer centers together to help expedite critical care transports out of the western part of the state and to safer locations.
Many transfers from impacted hospitals to new locations have required assistance from the Statewide Patient Coordination Team support cell. This process involves assessing patient needs, working to find capacity at a new facility and helping to arrange critical care transport.
“It’s hard to overstate the importance of this work, especially during a disaster that impacts critical communication services that care teams and patients rely on,” said Seals. “It takes tremendous coordination to ensure we can get patients safely transferred to a facility that has availability to care for them. In some cases, we’re receiving phone calls from people huddled in the corner of the hospitals because that’s the only place they can get service for a few moments. From there, we take that information to help arrange the necessary transport services.”
Should patients need to be transferred as far east as ECU Health, the system stands ready to serve patients and families from western North Carolina. In the meantime, as recovery efforts continue, ECU Health and EHPC are continuing to do their part to support those impacted by the devastation of the storm in whatever way they can.
“ECU Health is deeply involved and fully aware of what’s going on and is staying connected in the work, and we need to remember this is not a short-term turnaround,” said Floyd. “This issue is going to take a long time for them to get to some form of stability. But we’re here to help and committed to doing what we can to support those impacted.”
Healthy snacks, well-being resources, a mindful walking trail and more were all on display at ECU Health Medical Center’s new Resident Well-Being Zone as part of a recent pop-up event hosted by ECU Health’s Well-Being team.
Resident physicians from across the Medical Center were invited to the pop-up event as a way of showcasing the new space, intentionally designed to support their well-being as they continue in their journey in medical education.
The pop-up event, according to Dr. Christina Bowen, ECU Health’s chief well-being officer, is an important way of ensuring residents are aware of the resources available to them at ECU Health.

“We are thrilled to have a resident well-being zone and to be able to offer something unique and purposeful to our resident physicians, who play such an important role here at ECU Health Medical Center,” said Dr. Christina Bowen, Chief Well-being officer at ECU Health. “The pop-up events are a fun way to get our resident physicians engaged in well-being and mindfulness which we know will benefit them during their time here at ECU Health. Our team is excited to be able to host well-being events throughout the year.”
Located on the sixth floor of the Eddie and Jo Allison Smith Cancer Center at ECU Health Medical Center, the Resident Well-Being Zone officially opened in August after years of thoughtful design and funding provided by the ECU Health Foundation. The space is filled with all the essentials a resident may need: exercise equipment, charting space, healthy snacks, coffee, even a ping-pong table and more.
Dr. Cole Carter, a fourth-year physical medicine and rehabilitation resident, said the pop-up event and the space itself have proven to be a welcome asset in the resident experience at ECU Health.
“I think it’s great,” Dr. Carter said, noting that his favorite part of the space is the ping-pong table. “It’s a great place to check out when you need a break from the busy schedule. You can get a great view of Greenville and just take time to relax. I try to come up here once a month or so. This is a great asset for our residents and for those who may be looking for a residency program.”
Dr. Mary Catherine Turner, interim associate dean of Graduate Medical Education, understands first-hand the value of a Resident Well-Being Zone. She said she was fortunate to have one during her time as a resident physician, and it helped her take a break, refresh her mind and get re-engaged in the mission-driven work of providing high-quality health care. Now, she is excited that current and future resident physicians get to experience a similar benefit as they care for patients and continue to learn at one of the busiest academic medical centers in the nation.
“A space like this is important for residents,” Dr. Turner said. “Residents need a place where they can go and disconnect from their work for a little bit and reconnect with themselves. And importantly this is a place where residents can congregate together. I think there’s a lot that can be said for building a community, and this allows them the space to do that.”







