At ECU Health, the support team members provide to each other makes a difference – not only to those team members but also to the patients we serve across eastern North Carolina.
Recently, three ECU Health nurses were inducted into the East Carolina University (ECU) College of Nursing Hall of Fame while another earned a scholarship as she pursues her doctorate in nursing. These four ECU Health nurses each said the support of fellow nurses has uplifted them throughout their careers and the scholarship and inductions into the Hall of Fame is a reflection of that support.
Learn more about the honorees below.
Amy Campbell
Amy Campbell, quality nurse specialist at ECU Health, has been with the system for about 18 years over two separate stops.

 Campbell started at ECU Health Medical Center as an associate degree nurse in pediatrics and said she was quickly encouraged and supported by fellow nurses and leaders to join the HomeGrown program, which helps team members go back to school and balance their work and school responsibilities, and she received her bachelor’s degree from ECU in 2001. Campbell left ECU Health to teach at Pitt Community College and ultimately returned to the health system with a master’s degree. During her second stop at ECU Health, she said she was once again supported to further her education and pursue a doctorate degree, which she completed in 2020.
Campbell started at ECU Health Medical Center as an associate degree nurse in pediatrics and said she was quickly encouraged and supported by fellow nurses and leaders to join the HomeGrown program, which helps team members go back to school and balance their work and school responsibilities, and she received her bachelor’s degree from ECU in 2001. Campbell left ECU Health to teach at Pitt Community College and ultimately returned to the health system with a master’s degree. During her second stop at ECU Health, she said she was once again supported to further her education and pursue a doctorate degree, which she completed in 2020.
“A lot of executives were so encouraging for me to get my Ph.D. and I was HomeGrown and I was able to do my research here so they really were supportive all along,” Campbell said. “I also went through the Ph.D. program with a lot of my colleagues here so that was really great, too. I couldn’t have done it if people hadn’t given me time to do my research and to go to school.”
Campbell is a Williamston native and she said the rural aspect of the care ECU Health provides for the region is close to her heart.
The close-knit communities of eastern North Carolina transfer over to the hospital setting where Campbell said it’s a family atmosphere for team members and the patients they serve.
“I believe that at ECU Health we really do rise by lifting others and people really try to make sure others get time in the spotlight, even though, if you ask any of the four of us, we really don’t like this spotlight,” Campbell said. “But for me, I’m able to embrace it because I want all those people who supported me to have their moment with me. I’m a single mom, I’ve been a single mom for 19 years, but I’ve had a wonderful family here. Everyone has always been so good and supportive of school or whatever I was going through to help me be successful.”
Angela Still
 Angela Still, senior administrator of Women’s Services at ECU Health Medical Center, said she was humbled to join her colleagues who have been inducted into the ECU College of Nursing Hall of Fame as part of the Class of 2023.
Angela Still, senior administrator of Women’s Services at ECU Health Medical Center, said she was humbled to join her colleagues who have been inducted into the ECU College of Nursing Hall of Fame as part of the Class of 2023.
Still has been with the health system for 36 years and is a 1986 graduate of ECU. As a Greenville native, Still said the opportunity to care for and support women in eastern North Carolina is special to her.
“The needs of the patients and families in our region, the disparities, and the social determinants of health are so different from what the rest of the state deals with every day,” Still said. “Our 29 counties are comparable to the size of some states but it’s rural. Access to care, access to healthy food, these are unique needs. At this point in my career I am not impacting the individual patient and family, I’m working to impact the region. It’s a population of mothers and babies that we want to be healthier because they are our future in the region.”
Still said that during her time at ECU Health, she’s been the beneficiary of great leadership and mentors and she’s been happy to give that back to the next generation of nurses as they rise through the system and across the state.
She said it’s crucial to invest time and energy into mentorship as it will make a difference for the individual, those they mentor in the future and the patients they serve.
“The opportunity to mentor people through my career has been just really amazing. I have people across the state I mentored that are not with the system anymore and they still call me to ask questions or just look for guidance,” Still said. “So just being able to make an impact on the people that are going to care for others is very special to me. We’re all eventually going to retire, so being able to mentor and guide folks that are going to be here long after I’ve left and are going to continue to carry that torch and make a difference for our communities, it’s a big deal.”
Georgia Perry
 Georgia Perry is the nurse manager on 2 North Medicine and 2 North Progressive Care at ECU Health Medical Center and was also inducted into the ECU College of Nursing Hall of Fame this year.
Georgia Perry is the nurse manager on 2 North Medicine and 2 North Progressive Care at ECU Health Medical Center and was also inducted into the ECU College of Nursing Hall of Fame this year.
Perry said the night of the induction into the Hall of Fame was special for her as she had a chance to look into the crowd gathered and see mentors, some of whom nominated Perry for the recognition.
Perry earned her bachelor’s degree from ECU in 2010 and began working at ECU Health as part of the very first New Grad Nurse Residency Program class. She started working on 2 South, became an assistant nurse manager, and eventually became the nurse manager on her current unit. She received her master’s degree in 2015 and said the backing of fellow nurses and leaders alike made going back to school a manageable task.
“I tell people all the time, if you can dream it, you can do it here,” Perry said. “I truly feel like the support system is really what makes it easy to go back to school to be able to juggle it all. There’s a wealth of mentors here, you can pick up the phone and call anybody and it doesn’t matter if it’s across service lines.”
Perry is a Newton Grove native and said working in rural medicine is important to her because she grew up in a rural area.
“I think it’s wonderful that we have such great access to really all specialties right down the road,” Perry said. “My family actually will travel and get to ECU Health Duplin Hospital and then have access to the tertiary center, so we live it. I’m really grateful for what we have here at ECU Health and I’m glad to be a piece of the impact we have on this region.”
She added that the team around her keeps her going while the patients they serve inspire her to bring her best each day.
Lauren Nichols
 Inductees into the Hall of Fame help fund a scholarship for ECU College of Nursing students. Lauren Nichols, a staff nurse on the Cardiac Intermediate Unit at ECU Health Medical Center, earned a scholarship from the fund for this year.
Inductees into the Hall of Fame help fund a scholarship for ECU College of Nursing students. Lauren Nichols, a staff nurse on the Cardiac Intermediate Unit at ECU Health Medical Center, earned a scholarship from the fund for this year.
Nichols, who has been working at ECU Health for seven years, is pursuing a doctorate in nursing with a family nurse practitioner specialty at ECU.
Nichols is from Edgecombe County and said she chose to work at ECU Health and continue her education at ECU because of the health system’s commitment to rural health care and eastern North Carolina.
“ECU Health’s mission really resonates with me,” Nichols said. “Growing up in such a rural community makes me want to do my part to help improve the health of the people of eastern North Carolina.”
She said she never doubted her decision to go back to school because of the support she has received, especially from nursing leadership.
Join the Team
ECU Health nurses make an incredible impact every day across eastern North Carolina. Learn more about opportunities to work alongside these amazing nurses and so many others here.

Trish Baise
Since my arrival to the organization in January, I have enjoyed the privilege of getting to get to know the nurses of ECU Health. I’ve visited our acute care environments and interacted with a number of ambulatory care teams. In every visit, I come away inspired by the level of nursing care that is provided on a daily basis in communities across eastern North Carolina.
This week, May 6-12, is National Nurses Week, and it is my distinct honor to recognize and celebrate the incredible contributions of our ECU Health nurses. They demonstrate the mission, vision and values of ECU Health by providing excellent care in our hospitals and clinics. Nurses also serve in other critical roles across our health system focused on improving well-being, quality, safety, outcomes and access.
All nurses, regardless of their role, have a profound connection to purpose. Our purpose might be to provide hope to the hopeless, administer life-saving care that impacts generations of a family, give the support a colleague needs at just the right time, teach the next generation of nurses or be a part of innovation that fundamentally changes health care. If we pay attention, our careers our filled with daily moments of purpose, some small, some life changing. Our nurses are joined in purpose by 4.2 million nurses nationwide. It is the tie that binds us together. Together we will build upon our shared purpose as ECU Health nurses and become a national model for nursing excellence.
During National Nurses Week and beyond, I encourage our community to take the time to celebrate each and every one of the nurses providing care for our family, friends and neighbors. Nursing is the backbone of health care, and achieving the ECU Health mission would be impossible without them.
Thank you, ECU Health nurses, for your compassion, commitment to excellence and all you do for your patients and their families every day. ECU Health, our patients and our communities all benefit because you choose to serve eastern North Carolina.
For more than 25 years, the Pediatric Asthma Program at the Maynard Children’s Hospital at ECU Health Medical Center has worked to help patients and families living with asthma lead healthy lives.
Jeanine Sharpe, social work care manager for the Pediatric Asthma Program, said the goal of the program has always been to decrease emergency department visits, reduce school absences due to asthma, provide education and improve quality of life for patients and families.
“Currently, there are about 5.1 million children under the age of 18 that have asthma in the U.S. and it’s the leading chronic disease for children,” Sharpe said. “Just for our service area last year, we had 1,687 pediatric asthma patient referrals. It’s the number one reason for school absences and the number two reason for hospital admissions for children. But we know that asthma is a controllable disease. What we find is that a lot of times the missing piece is just education.”
Sharpe said the program has touched many families over the years, whether it’s just one interaction or years of working on a family’s case. One family that has seen the impact of the program recently is the Carr family.
Dalton Carr III was diagnosed with asthma three years ago and struggled with wheezing, coughing and attacks in the years since.

Dalton III’s mother, Shanika said she was scared when her son was first diagnosed and she wasn’t sure how to handle certain situations. This past December, Dalton had an incident and was seen in the emergency department for his asthma.
“That’s when I met Ms. Sharpe,” Shanika said. “I was confused at the time, but ever since I met Ms. Sharpe, it’s been easier to learn things. I was confused with the things different doctors were telling me and I really didn’t understand how serious it was.”
Dalton III’s father, Dalton Jr., said it has been a great experience working with Sharpe and the Pediatric Asthma Program team.
He said the education and support offered have helped their son be confident and join in the everyday activities of other children his age. While he used to struggle, today he does not wheeze, cough or have flare ups from his asthma. Dalton Jr. credited the work with the Pediatric Asthma Program for this turnaround.
“She got us in a good routine for him. Ever since we’ve gotten Dalton on a consistent routine, he hasn’t had any problems,” Dalton Jr. said. “It’s even to the point where he can tell us when he needs his pump. He might say, ‘Mom or dad, I need my pump’ or ‘I’m good.’ He plays football and he’s running and tackling and it’s a lot but with Ms. Sharpe being in our lives these last few months, it’s just helped a lot.”
Dalton Jr. encouraged families to reach out for help and to learn what might work best for their child’s asthma.
Malorie Whitaker, respiratory care manager at ECU Health Medical Center, said the program is designed to help patients from one to 18 years of age feel more comfortable while they manage their asthma and participate in normal childhood activities.
She also said the program is set up to meet children where they are and eliminate barriers to care.
“Sometimes they’ll come into our office to do different testing or do some education, but usually we meet them,” Whitaker said. “So we’ll get into the homes, we’ll go into the schools, into the clinic, wherever they are. Some of these kids that we see don’t have transportation or transportation is difficult for them, so that’s why we like to go into the school or into the homes to help them.”
To learn more, or to speak with someone close to you, visit the Pediatric Asthma page or call one of the ECU Health locations offering pediatric asthma services.
- ECU Health Bertie Hospital: 252-833-2861
- ECU Health Chowan Hospital: 252-833-2861
- ECU Health Edgecombe Hospital: 252-641-7382
- ECU Health Medical Center: 252-847-6835
- ECU Health Roanoke-Chowan Hospital: 252-209-3117

Brian Floyd
ECU Health Chief Operating Officer and ECU Health Medical Center President Brian Floyd joined other rural health care leaders from across the state for a virtual town hall hosted by the North Carolina Healthcare Association on Tuesday, April 11.
During “Reimagining Rural Health in North Carolina,” Floyd and the 4 other panelists – Jessie Tucker, president and CEO at UNC Health Wayne, Kathy Bailey, president and CEO at UNC Health Blue Ridge, Lynda Stanley, President and CEO at Dosher Memorial Hospital, and Michelle Fortune, CEO at St. Luke’s Hospital – discussed how they are evolving the future of rural health care in the state.
Like many rural regions, 1.4 million people who call eastern North Carolina home face a number of systemic socioeconomic challenges, which have negative impacts on health outcomes. The panelists discussed the unique challenges rural health care faces, how Medicaid expansion will impact rural health care and communities, workforce development, community partnerships and outreach and innovations. Partnerships and collaboration were a key topic and many rural health systems across the state, including ECU Health, continue to identify solutions to improve access to care in rural communities.
“I was honored to discuss rural health care challenges, successes and innovations alongside fellow rural health leaders across North Carolina at today’s town hall,” said Floyd. “ECU Health and the Brody School of Medicine at East Carolina University are uniquely positioned to help train the next generation of physicians and health care workers. Together, we can address the issues that rural communities face like a lack of access to health care resources and disproportionate chronic illness. From community education, to partnerships that make every social system more vital, to caring for people at their worst and sometimes best day, the work we get to do is so fulfilling.”
Wildwood Park in Greenville served as the perfect setting for “Emergency Medicine Wilderness Day” as ECU Health emergency medicine residents practiced assessing and treating a variety of common outdoor ailments including altitude sickness, lightning strikes, falls from trees and more.
On March 29, approximately 20 emergency medicine residents attended training and worked in small groups to run through simulated injury scenarios with real people. From knowing how to stabilize an injured person, to assessing injuries and helping get them to safety, emergency residents worked together to treat the injuries under the watchful eye of experienced faculty members from the Brody School of Medicine at East Carolina University. Residents received real-time instruction and feedback from faculty as they worked through their training.
Standardized patients from Brody’s Office of Clinical Skills Assessment and Education acted as the patients in each scenario. Standardized patients are trained to mimic real patients so that students can learn. Their role is to help prepare future health care professionals for a variety of patient interfaces.

“There are a number of practical applications for this type of training, especially for our medical residents who get to test their knowledge in the field,” said Dr. Jennifer Bennett, an emergency medicine physician at ECU Health and clinical assistant professor of emergency medicine at Brody. “These scenarios are the types of things that we, as emergency medicine physicians, address somewhat commonly. We can apply the knowledge and skills learned out here to patient care.”
The day was a success, according to Dr. Bennett, who helped create the simulation Emergency Medicine Wilderness Day training event last year alongside Dr. Jennifer Parker-Cote, assistant professor of emergency medicine at Brody. Both doctors helped organize the Wilderness Day, coming up with unique patient scenarios, including the altitude sickness training station which featured a standardized patient acting as a distressed hiker. The residents removed a fake snake from the area, asked the patient questions about their medications and medical history, moved the patient to a lower area and helped get them to further medical care.
“It’s always nice to get outdoors instead of sitting in a lecture hall,” said emergency medicine resident Tyler Ruchti, DO. “When you’re in the hospital, you have all of your tools and all of your equipment and know where it is, and when we come out here and do things like this it’s a change of scenery. You have to think outside the box.”
The training is another example of the valued partnership between ECU Health and Brody. Residents at an academic health system like ECU Health have support and resources for continued education from faculty and the Interprofessional Clinical Simulation Program at Brody, enriching their clinical training experience. Residents are able to participate in trainings like this to prepare for real situations with real patients both behind the walls of the hospital and out in the community.
“This training was partially about simulating complex medical issues that you may encounter in the wilderness as well as providing a little wellness for our residents,” said Dr. Parker-Cote. “This is a fun way to test knowledge and work together as a team. When it comes to education, there are different modalities for teaching. Learning in this type of environment provides us another way of reinforcing the knowledge they have learned throughout their residency, and it prepares them to help their fellow community members no matter the situation.”
Resources

Patient-centered care is a term often used in health care to describe a collaborative relationship between care teams, patients and families. It is the goal of many health care providers, the type of relationship that occurs only when trust is fully developed.
For medical students learning the trade, there are right and wrong answers to most of the questions they encounter. These symptoms match that disorder, or this medication cannot be given to that type of patient. While there is much to learn about the science of medicine from the pages of a textbook or within the walls of the classroom, it is hard to replicate the hands-on experience gained during direct patient care. Often times, the best lessons come from long days and nights spent compassionately caring for patients, listening to feedback, patiently answering questions and validating the feelings of those they care for.
“It’s one of those things that you’re taught in medical school to listen to patients and their families because it really is shared decision making,” said third-year Brody School of Medicine at East Carolina University student Jennifer McMains. “But then when you get in the moment, there’s so much going on and it’s very easy to think that you know medically what’s best. But that’s not the way we practice medicine. If the family feels strongly, then listen because they’re with their loved one every single day, every minute.”
McMains learned firsthand the importance of patient-centered care when she met Carnie and Melody Hedgepeth in June 2022 during one of the most difficult periods of their lives.
Carnie, who serves as the director of emergency services for Beaufort County and as a pastor at Arthur Christian Church, was out for a summer ride on his motorcycle when he was involved in a serious accident. He was hit by an oncoming driver and thrown from his bike, eventually landing on the roof of the car. Despite wearing a helmet, the accident left him with multiple facial injuries and a brain bleed that resulted in a traumatic brain injury. With Melody by his side, Carnie spent more than a month in ECU Health Medical Center where they quickly found an expansive support system.
“A lot of people in the (emergency room) know him and people surrounded us with love and prayers,” said Melody. “We got through that first night thanks to everyone in the ER.”
It was in the ER during her surgery rotation where McMains would first meet the Hedgepeths.
“We would go in as a team of doctors to check and provide updates on the plan,” McMains recalled. “Melody was constantly asking ‘Can we be doing anything more?’ or ‘Are there better ways for us to position his feet?’ Things like that seem small but she was always looking at the six-months, one-year outcome and always believing that he would recover. That showed me a lot because I would go into the next person’s room and there wouldn’t be a person to advocate.”
For the Hedgepeths, the attention and care they received left a lasting impression.
“From my standpoint, that’s the most important thing, knowing that the person who is calling the shots cares,” said Carnie. “It means so much when you know that the person cares.”
Carnie, Melody and McMains were reunited April 6 at the Hilton in Greenville during the Legacy Teachers Celebration, a tradition presented by Brody and ECU Health that gives students a chance to honor a patient they met during third-year rotations who taught lessons about care, compassion and communication they will take with them into their careers as physicians.

In total, 20 third-year medical students shared their stories at the luncheon, which featured gift baskets, a photo station and remarks from ECU Health and Brody leaders. At the end, legacy teachers placed custom pins on the students’ white coats to commemorate the significance of the occasion and serve as a reminder of the lessons learned – lessons that they will carry with them through their medical careers.
“As physicians, these stories fuel our hearts and purpose for servant leadership in our pursuit of medicine,” said Dr. Christina Bowen, ECU Health chief well-being officer. “The connections we make with patients help us learn the art of practicing medicine. We’re here to honor these sacred relationships and celebrate our legacy teachers.”
Third-year Brody student Karen Semaan shared her experience with former patient Aidan Mummert and his grandparents. Semaan got to know them well while on the pediatric hematology-oncology rotation. At first, the care team was unsure of the cause of Mummert’s illness. They visited Mummert and his family often to ask more questions and run more tests. Despite the uncertainty, the family and care team developed a light-hearted and fun relationship. When doctors finally determined the cause of the infection, the care team celebrated with joy alongside the family during Mummert’s discharge.
Semaan said the relationship she developed with Mummert and his family was a reminder of her “why” as a future physician.
“Talking with Aidan and his grandmother reminded me, even though medicine and medical school is hard, even though you’re tired and your emotional reserves are low, you can get energy from people,” Semaan said. “You can get love and compassion from them that you can then give back and share with other patients that you see that day.”
The Legacy Teachers Celebration is an important partnership between ECU Health and Brody. The education that medical students receive at Brody, combined with the experiences gained within the ECU Health clinical setting, provides a full spectrum of knowledge that prepares them to deliver compassionate care to the patients they will serve.
“Today is one of the greatest days because we get to celebrate the relationship between our student doctors and their patients,” said Dr. Amanda Higginson, associate dean for student affairs at Brody. “Together, Brody and ECU Health have a shared responsibility to provide both healing and learning. Our legacy teachers help us do that in ways that go beyond just the classroom setting.”
Dr. David Eldridge, senior associate dean for academic affairs at Brody and Brian Floyd, chief operating office at ECU Health and president of ECU Health Medical Center, provided remarks at the event. Like the students, they shared their deeply personal stories of important lessons they learned as students. The speakers shared common themes, especially around the importance of positive, trusting relationships between patients and care teams.
“All across health care, and especially here at ECU Health, there incredible people gathered around others who are in-need of care,” said Floyd. “We’ve chosen this work because it is so meaningful. We are able to make a difference in the lives of so many because of the beautiful relationship between these students and these patients. Today is a reminder of why we do what we do.”
On Wednesday, ECU Health Medical Center partnered with Honorbridge to celebrate National Donate Life Month and recognize organ and tissue donors, their families, those who are waiting for life-saving and life-changing donations, and recipients of organ and tissue donations.
The occasion was marked at 10:08 a.m. as the Donate Life flag was raised in front of ECU Health Medical Center, followed by a 30-second moment of silence. These two numbers are significant as the time symbolizes that one donor can save eight lives while the moment of silence recognizes the 3,000 North Carolinians waiting for an organ donation.
Dr. Walter Pofahl, chief medical officer for ECU Health Medical Center, said eastern North Carolina is home to a disproportionately high number of those 3,000 in North Carolina. Dr. Pofahl shared that last year ECU Health Medical Center had 31 organ donors, transplanted 90 organs while 18 were sent out for research. It also had 56 tissue donors with 141 tissues recovered and 90 eye donors with 84 corneas transplanted and 21 placed for research.
A daughter’s gift

During Wednesday’s event, Darice Fonville shared her inspiring story of donating her kidney to her mother in February.
Fonville said her mother had suffered from chronic kidney disease for about 20 years and as she began to struggle more, they learned she would need to find a donor or start dialysis. She knew that dialysis can be very difficult for patients, and she wanted to help her mother any way she could. So Darice decided to get tested to see if she would be a match.
“I was actually at work when I got the call, and they let me know we were a match,” Fonville said. “As soon as I got that call, everybody in the office already knew how excited I was. I put work on pause to go call my mom. She already knew, and she was nervous. I was excited. I knew it was a done deal. We were just going to go through with it.”

She said she never had any hesitation when she knew she could give something back to her mother and improve her life. She said the transplant team at ECU Health Medical Center put everyone at ease and allowed Fonville and her mother to be together shortly before surgery to spend time with one another.
How to give
Dr. Pofahl said while it is important to identify as an organ donor when you receive your driver’s license or state identification card, it’s just as important to share your wishes with those close to you.
“It’s not always easy, but having that discussion is important,” Dr. Pofahl said. “In that critical time when decisions are being made around donation, if your loved ones understand what your wishes are upfront and ahead of time, that makes the process a lot easier.”
While only about 50 percent of adults in North Carolina are registered organ donors, there are 3,000 people waiting for organ and tissue donations in North Carolina and more than 100,000 waiting for a donation across the country.
Learn more about how to become an organ donor and the impact you can make as a donor on Donate Life’s website.
Resources
Survivors of stroke and brain injury had an opportunity to artistically express their journey during a recent Unmasking Brain Injury event at ECU Health Medical Center.
The Brain Injury Association of North Carolina sponsored the Unmasking Brain Injury workshop. This event provides blank face masks and supplies to decorate the masks. Unmasking Brain Injury is an organization that aims to bring awareness to the prevalence of brain injuries and give survivors a voice and the means to educate others of what it’s like to live and recover with a brain injury. The event was the first of its kind in the ECU Health system.
Michele Horvath, stroke navigator at ECU Health Medical Center, helped run the event and said it was a wonderful moment to share with survivors.
“Everybody was really engaged and it was an emotional time for survivors because it made them artistically express their stroke or their traumatic brain injury and some of them are still in recovery,” Horvath said. “They’re really excited to share their story and it was really heartfelt. We’re hoping to bring community awareness to some of these brain injuries.”

Along with a support person, each attendee, many of them members of ECU Health’s Stroke Support Network, decorated a mask to represent their journey and recovery process from their stroke or brain injury.
Molly Twiss, marketing coordinator at the Brain Injury Association of North Carolina, said it was the first Unmasking Brain Injury event she’d helped coordinate and she felt inspired after the event. She explained that the masks could be anything attendees wanted, not just their brain injury or stroke, but about themselves as a whole.
“The masks are a look inside of them, what they’re feeling, what they’ve gone through, what they hope for the future,” Twiss said. “Some can be as small as their favorite TV show, their favorite color or something about what their life was like before their injury. So if they were a skier beforehand and their accident was a ski accident, they can have it ski related. The mask could represent just something to get their mind off of having this invisible injury.”
Discovering New Passions
Wendy Gardner had her first child in 2000. Ten days after her son was born in Wilson, she suffered a hemorrhagic stroke, which has affected the left side of her body.
About a year ago, Gardner joined the Stroke Support Network at ECU Health and she said she’s enjoyed connecting with people in eastern North Carolina who have had similar experiences. She said the Unmasking Brain Injury event was a positive experience for everyone and she hopes for similar events through the support group in the future.
Gardner’s mask was painted red white and blue and adorned with a gold medal, representative of her new found passion — and talent — for archery.
About three years ago, Gardner stumbled upon archery as a sport she could participate in. Today, Gardner is a member of the USA Para Archery World team.

“I hadn’t been able to find a sport that I can do because my whole left side of my body is affected,” Gardner said. “So I can’t run and I really can’t swim and do the usual activities. So I’d kind of given up actually finding something that I could do. We happened to go to a big archery competition because our daughter was interested in it. I saw a guy who has no arms and shoots with his feet and his name is Matt Stutzman. He’s on our team. That is what got me inspired. I thought, if he can do it with no arms and I have one arm I could use, we could find some way for me to do this.”
Wendy and her husband went to work on figuring out some adaptive equipment to help her hone her new craft. She said there are not many resources available to help people with making adaptive archery equipment so they went through a “trial and error” process.
Once the Gardner family got a handle on making adaptive equipment and realized how expensive it could be for others to create their own equipment, they started a nonprofit called GX4 Adaptive Archery.
Her attitude since first suffering her stroke has made all the difference. She said she never expected to be involved in something like the USA Archery Team, and through her determination to try new things—coupled with her relentless effort—Gardner now travels the world doing something she loves.
This includes trips to the United Arab Emirates, Chile and Czech Republic with the team, and she hopes to be in France next summer for the 2024 Paralympic Games.
“I’m always like, ‘Why not me?’ And I would never have done anything like this if this had not happened to me,” Gardner said. “So I always tell people, go try something new. The main thing is show up, you’ve got to show up and don’t be afraid to look foolish doing it. Because sometimes, as someone with a physical disability, you will. But just show up and try and do your best.”
Resources
Stroke Support Network – Upcoming Events
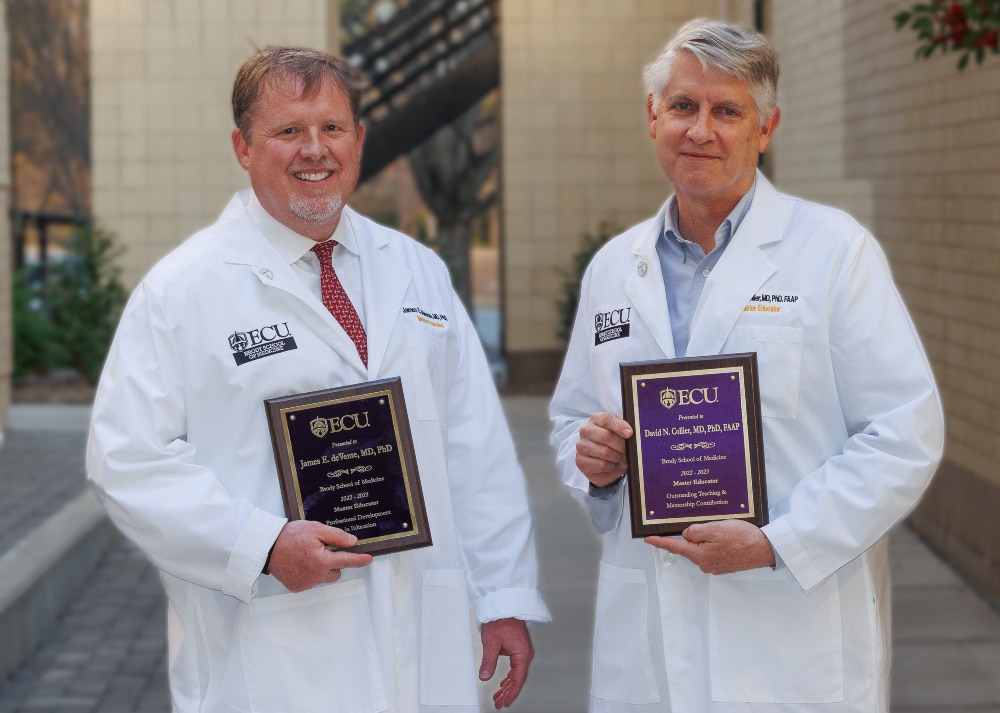
Three physicians – Drs. David Collier, James deVente and Ricky Watson – were recently named master educators by the Brody School of Medicine at East Carolina University. All three are Brody alumni.
The school’s master educator program recognizes excellence in leadership and administration, teaching contribution or mentorship, innovation and curriculum development, evaluation and research, professional development in education and educational contributions by community physicians.
The winners were announced during a Brody faculty meeting on Feb. 16, during which each winner received a white coat featuring a master educator designation, a plaque and master educator pin.
Faculty members and students may nominate faculty members to receive the award, and a committee of faculty members and students decides on the recipients.
Since the program began in 2002, close to 80 Brody faculty members have received the master educator recognition. The awards can be given in the areas of educational leadership and administration, outstanding teaching or mentorship contribution, educational innovation and curriculum development, educational evaluation and research, professional development in education and outstanding educational contribution by a community physician.
“The bestowing of the Master Educator Award allows us to honor faculty who have a sustained record of excellence in education and are who are recognized by their peers and learners as exemplifying leadership in education,” said Allison Flowers, director of Brody’s Office of Faculty Affairs and Leadership Development. “These master educators highlight how the Brody School of Medicine attracts and retains high-quality faculty who are driven by and demonstrate our mission.”
Dr. David Collier
Master Educator in Teaching and Mentorship
Dr. David Collier is a professor of pediatrics and health disparities and director of the Pediatric Healthy Weight Research and Treatment Center. He is associate director of the Integrative Health Sciences Facility Core in the NCSU Center for Human Health and the Environment.
Collier is a graduate of the Brody School of Medicine and completed his residency at Pitt County Memorial Hospital, now ECU Health Medical Center. His research interests include the prevention and treatment of childhood obesity.
Collier’s nominator highlighted his ability to share his knowledge in ways that benefit both his students and colleagues.
“David was a creative interprofessional educator before interprofessional education was a goal or mandate,” according to the nomination letter. “Dr. Collier is shown at his best — not in a classroom, not scripted — but in clinic teaching interprofessionally.”
Dr. James deVente
Master Educator in Education
Dr. James deVente is an associate professor in Brody’s Department of Obstetrics and Gynecology and is director of obstetrics at ECU Health Medical Center. At ECU since 2005, deVente graduated from the Brody School of Medicine in 2001 and completed a residency in obstetrics and gynecology in Greenville as well.
deVente has also served as the medical director for women’s services at ECU Health Medical Center since 2007 and is a trailblazer for innovation in the profession.
“In keeping with Jim’s passionate and tireless work as an educator, he has capitalized on his role to improve our entire health system through an ongoing series of faculty development opportunities,” according to the letter of nomination written for deVente. “Every obstetrical provider in our hospital system, across our portion of the state, has met with Jim for safety drills, new equipment training, fetal heart rate monitoring classes, and systemwide implementation of safety and quality initiatives – many of which he also helped to develop.”
Dr. Ricky Watson
Master Educator in Teaching and Mentorship
Dr. Ricky Watson is a clinical assistant professor and assistant residency director in the Department of Family Medicine. He is a Brody graduate and completed his residency at Pitt County Memorial Hospital, now ECU Health Medical Center. His areas of interest include women’s health, infectious diseases, travel and wilderness medicine and health care delivery systems.
Watson has earned a variety of teaching awards over the years including a Faculty Excellence Award for Excellence in Teaching and Compassion from family medicine residents. He has also received a teaching award from the American Academy of Family Physicians. He joined the ECU family medicine faculty in 2001.
“I know Ricky has delighted in helping other faculty, residents and students, new to our area, understand the needs of our patients,” reads his nominator’s letter. “He has been a steady source of education and inspiration for medical students and residents, fellows and junior faculty. He has been our go-to person for cultural competence and humility training for residents.”
Read more from ECU News Services
![Ricky Watson1[53] Dr. Ricky Watson poses for a photo after he was recently named a master educator by the Brody School of Medicine at East Carolina University.](https://www.ecuhealth.org/wp-content/uploads/2023/03/Ricky-Watson153-scaled.jpg)
By ECU News Services and ECU Health News
Getting through medical school can be tough – long hours, books and tests, and more books. However, in between classes and all-nighters, two students from the Brody School of Medicine have established a flourishing volunteer program to bring doula-like services to a region of North Carolina starved for birthing support.
The birthing companion program was started in October 2022 by Uma Gaddamanugu and Shantell McLaggan, both second-year Brody students and Schweitzer fellows. The Albert Schweitzer Fellowship supports graduate health professionals drawn from across the state who learn and work to address unmet health care needs in North Carolina.
Gaddamanugu’s and McLaggan’s fellowship project is focused on improving birth experiences of high-risk pregnant mothers in eastern North Carolina through the free birth support program to add an extra layer of support for women in the birthing process.

Patient populations in rural parts of eastern North Carolina simply need more help, Winston-Salem native Gaddamanugu said, from prenatal care through the laboring process, and certified doulas are an expensive out-of-pocket resource for which most North Carolinians must pay out of pocket because health insurance often doesn’t cover the cost.
“We are the only hospital with a high-risk labor and delivery unit for half the state. You think about how far some of these people have to travel, which makes it way harder for their support people to come with them,” Gaddamanugu said.
In February 2022, the North Carolina Institute of Medicine reported that the state’s maternal mortality rate was 27.6 per 100,000 births, which is slightly lower than the national average, but more than double the previous year’s rate of 12.1 per 100,000 births.
A 2021 study by the North Carolina Maternal Mortality Review Committee reported that 60 women died from pregnancy related causes from 2014-2016. Of those, nearly 60% were from minority racial categories and more than one in three were from rural areas. What’s more troubling – the study determined that 70% of maternal deaths could have been prevented by changing “patient, family, provider, facility, system and/or community factors.”
The program
At first, the program had 18 volunteers, but since its inception in October 2022 the ranks of birthing support volunteers have doubled to 37. At the beginning of February, the volunteers had assisted with more than 70 births, which is “way past our goal that we had initially set,” Gaddamanugu said.
Volunteers from the program come from a wide range of backgrounds, though most are medical or nursing students. Some are undergraduate students from main campus who want to be part of a program that serves the community. For now, the program is staffed almost completely by ECU students, though Gaddamanugu and McLaggan will soon hand the program’s day-to-day management off to first-year medical students who aim to open the program up to the public.
“Our program is very much modeled off a program at UNC. They’ve been doing that for about 20 years,” Gaddamanugu said. “A Wake Forest medical student started a similar volunteer doula program two years ago through the Schwitzer Fellowship. It’s just neat to see that it was possible with the structure of the organization to bring that program here, because there’s a whole different need in eastern North Carolina.”
Gaddamanugu stressed that the volunteers in the program, who support the labor and delivery services at ECU Health, aren’t certified doulas but rather are there to help during the immediate labor process. For one delivery, that might be a non-clinical, non-medical role – a friendly face and a hand to hold – and in other cases it might be running through the hospital to find a phone charging cable so a mother can stay in contact with her other children at home.
Leslie Coggins, a charge nurse on the labor and delivery unit at ECU Health Medical Center in Greenville, said the volunteer program has been a great success, both for the mothers in the delivery process as well as for students on track to become the next generation of health care providers.
“We’ve always had a great relationship with our residents, but now we have almost a pipeline — doctors, potential doctors, nurses, someone interested in birth and supporting birth in its natural function,” Coggins said. “To share that experience with up-and-coming providers and nurses who will be taking our places someday is huge.”
While the volunteer program is currently staffed by students, the student organizers and Coggins as the nurse manager of the labor and delivery unit hope to soon include members of the public. Those interested in volunteering should contact the program by emailing [email protected].
Training medical professionals

The ECU version of a volunteer birth companion program is rooted in experiences both medical students had working as volunteers in hospitals in doula-like roles. Gaddamanugu volunteered during her time as an undergraduate at UNC; McLaggan, who is from Thomasville, spent several years after her undergraduate education working at the Cherokee Indian Hospital in western North Carolina and helped establish a volunteer doula program there.
Both students are interested in pursuing a career in obstetrics.
McLaggan’s mother told her from an early age that she was smart enough to be a doctor. After researching the requirements and being captivated by the science of medicine, she fell in love with the idea.
“I feel like I have the mental, emotional and the physical capacity to do something as strenuous as being a doctor,” McLaggan said. “Because I have those qualities, I feel like it’s my obligation to become a doctor and serve people to the maximum of my abilities.”
Medicine was also a calling for Gaddamanugu, who said that the challenge is humbling but she sees a future where she can make a difference by “maternal and child health disparities in our community” which fit the impact that she hopes to make in the world.
She said that the experiences at the bedside have colored the conversations that she has with her medical school peers about the experience of medicine from the patient’s perspective.
“We know birth is hard, but here is what it really can look like,” Gaddamanugu said. “The U.S. has an awful maternal mortality crisis, and we can hear those numbers all day long in school, but the numbers don’t mean anything until you see it in person, and you realize some of these patients are extremely sick.”
For Dr. Kerianne Crockett, ECU Health OB/GYN and Brody clinical assistant professor, the program has clear benefits for the patients she serves. She has heard from patients who appreciated having another source of support during their delivery.
“Delivering a baby is one of the most exhausting, exhilarating, sometimes scary experiences of a patient’s life,” Crockett said. “There is good evidence that patients with a continuous support person present throughout labor — whether that person is a family member, a spouse or a doula — have better birth outcomes, including lower rates of cesarean delivery. I am so proud that our bright, compassionate, empathetic medical students are now able to be that continuous support person for all kinds of patients, including those who otherwise would not have had anyone besides the medical team there for their delivery.”
Student involvement in health care delivery, and the unique perspectives students offer patients, is a hallmark of a large academic health system like ECU Health. As students learn from the clinical experience of providers at ECU Health, they are empowered to innovate and bring ideas to the table that lead to better patient experiences and brighter outcomes.
“As an academic health system, our medical students help to enrich the patient experience with their energy and ideas,” said Angela Still, senior administrator of women’s services at ECU Health Medical Center. “The birthing support volunteer initiative is a great example of how Brody students go beyond the walls of the classroom and make a direct impact on the patients we’re proud to serve.”
Serving eastern North Carolina
Sometimes the most important support that a birthing companion can provide comes from skills that can’t be taught in a formal doula class.
McLaggan remembers one time she volunteered with a woman who had a number of kids already — the most recent born by C-section. The medical staff recommended another C-section, which the woman was reluctant to agree to due to the complications she had with the previous birth. The challenge that McLaggan was able to help resolve wasn’t convincing the woman to have a C-section, but rather just communicating with her at all. The woman was Haitian and spoke Haitian Creole and little English.
“I happened to speak French, which is very similar to Haitian Creole, so she was able to communicate to me, where she was coming from and what her needs were,” McLaggan remembered. “I was able to bridge that gap and she ended up delivering naturally. I felt so honored and privileged to have been in the room.”
Another of the volunteers in the program has similar experiences with language gaps being a hindrance to quality health care. An undergraduate student recounted to Gaddamanugu how, growing up in eastern North Carolina, she was always saddled with translating for her mother and siblings during medical appointments — a task that shouldn’t really be shouldered by a young person. The student volunteer said, though tears, that she was so grateful to be able to translate for delivering mothers because she knew first-hand the constricting fear and anxiety of being language-locked in a stressful medical situation.
While the language capabilities that some students bring to the hospital bedside are important, Coggins said, patient populations in eastern North Carolina are getting sicker, which often requires the health care team members to devote their attention to the physiological status of the patient.
“We try to promote natural delivery as much as we can,” Coggins said, but sometimes the medical conditions of the mother and baby require doctors and nurses to focus on the immediate illness. “One-on-one support is essential with our patients. A lot of times our sick population are not from around here and don’t have the support system in place, so this is an added benefit so our nurses can focus on what is medically happening and where we need intervene.”
Gaddamaugu is awed at the privilege of being present at a birth.
“I’ve cried every single time; it’s one or two single tears, but they were C-section babies and you could sense the relief in the OR the moment the baby comes out safe and healthy,” Gaddamaugu said.
McLaggan has known that being in the room during the birthing process is what she has wanted to do since before kindergarten. She’s seen a handful of births as a volunteer and continues to be amazed by each one.
“Words don’t describe how amazing childbirth really is. I get so overwhelmed with emotion when I see 37 to 40 weeks of work and love going into this child that is coming into the world,” McLaggan said.



