Patient-centered care is a term often used in health care to describe a collaborative relationship between care teams, patients and families. It is the goal of many health care providers, the type of relationship that occurs only when trust is fully developed.
For medical students learning the trade, there are right and wrong answers to most of the questions they encounter. These symptoms match that disorder, or this medication cannot be given to that type of patient. While there is much to learn about the science of medicine from the pages of a textbook or within the walls of the classroom, it is hard to replicate the hands-on experience gained during direct patient care. Often times, the best lessons come from long days and nights spent compassionately caring for patients, listening to feedback, patiently answering questions and validating the feelings of those they care for.
“It’s one of those things that you’re taught in medical school to listen to patients and their families because it really is shared decision making,” said third-year Brody School of Medicine at East Carolina University student Jennifer McMains. “But then when you get in the moment, there’s so much going on and it’s very easy to think that you know medically what’s best. But that’s not the way we practice medicine. If the family feels strongly, then listen because they’re with their loved one every single day, every minute.”
McMains learned firsthand the importance of patient-centered care when she met Carnie and Melody Hedgepeth in June 2022 during one of the most difficult periods of their lives.
Carnie, who serves as the director of emergency services for Beaufort County and as a pastor at Arthur Christian Church, was out for a summer ride on his motorcycle when he was involved in a serious accident. He was hit by an oncoming driver and thrown from his bike, eventually landing on the roof of the car. Despite wearing a helmet, the accident left him with multiple facial injuries and a brain bleed that resulted in a traumatic brain injury. With Melody by his side, Carnie spent more than a month in ECU Health Medical Center where they quickly found an expansive support system.
“A lot of people in the (emergency room) know him and people surrounded us with love and prayers,” said Melody. “We got through that first night thanks to everyone in the ER.”
It was in the ER during her surgery rotation where McMains would first meet the Hedgepeths.
“We would go in as a team of doctors to check and provide updates on the plan,” McMains recalled. “Melody was constantly asking ‘Can we be doing anything more?’ or ‘Are there better ways for us to position his feet?’ Things like that seem small but she was always looking at the six-months, one-year outcome and always believing that he would recover. That showed me a lot because I would go into the next person’s room and there wouldn’t be a person to advocate.”
For the Hedgepeths, the attention and care they received left a lasting impression.
“From my standpoint, that’s the most important thing, knowing that the person who is calling the shots cares,” said Carnie. “It means so much when you know that the person cares.”
Carnie, Melody and McMains were reunited April 6 at the Hilton in Greenville during the Legacy Teachers Celebration, a tradition presented by Brody and ECU Health that gives students a chance to honor a patient they met during third-year rotations who taught lessons about care, compassion and communication they will take with them into their careers as physicians.

In total, 20 third-year medical students shared their stories at the luncheon, which featured gift baskets, a photo station and remarks from ECU Health and Brody leaders. At the end, legacy teachers placed custom pins on the students’ white coats to commemorate the significance of the occasion and serve as a reminder of the lessons learned – lessons that they will carry with them through their medical careers.
“As physicians, these stories fuel our hearts and purpose for servant leadership in our pursuit of medicine,” said Dr. Christina Bowen, ECU Health chief well-being officer. “The connections we make with patients help us learn the art of practicing medicine. We’re here to honor these sacred relationships and celebrate our legacy teachers.”
Third-year Brody student Karen Semaan shared her experience with former patient Aidan Mummert and his grandparents. Semaan got to know them well while on the pediatric hematology-oncology rotation. At first, the care team was unsure of the cause of Mummert’s illness. They visited Mummert and his family often to ask more questions and run more tests. Despite the uncertainty, the family and care team developed a light-hearted and fun relationship. When doctors finally determined the cause of the infection, the care team celebrated with joy alongside the family during Mummert’s discharge.
Semaan said the relationship she developed with Mummert and his family was a reminder of her “why” as a future physician.
“Talking with Aidan and his grandmother reminded me, even though medicine and medical school is hard, even though you’re tired and your emotional reserves are low, you can get energy from people,” Semaan said. “You can get love and compassion from them that you can then give back and share with other patients that you see that day.”
The Legacy Teachers Celebration is an important partnership between ECU Health and Brody. The education that medical students receive at Brody, combined with the experiences gained within the ECU Health clinical setting, provides a full spectrum of knowledge that prepares them to deliver compassionate care to the patients they will serve.
“Today is one of the greatest days because we get to celebrate the relationship between our student doctors and their patients,” said Dr. Amanda Higginson, associate dean for student affairs at Brody. “Together, Brody and ECU Health have a shared responsibility to provide both healing and learning. Our legacy teachers help us do that in ways that go beyond just the classroom setting.”
Dr. David Eldridge, senior associate dean for academic affairs at Brody and Brian Floyd, chief operating office at ECU Health and president of ECU Health Medical Center, provided remarks at the event. Like the students, they shared their deeply personal stories of important lessons they learned as students. The speakers shared common themes, especially around the importance of positive, trusting relationships between patients and care teams.
“All across health care, and especially here at ECU Health, there incredible people gathered around others who are in-need of care,” said Floyd. “We’ve chosen this work because it is so meaningful. We are able to make a difference in the lives of so many because of the beautiful relationship between these students and these patients. Today is a reminder of why we do what we do.”
On Wednesday, ECU Health Medical Center partnered with Honorbridge to celebrate National Donate Life Month and recognize organ and tissue donors, their families, those who are waiting for life-saving and life-changing donations, and recipients of organ and tissue donations.
The occasion was marked at 10:08 a.m. as the Donate Life flag was raised in front of ECU Health Medical Center, followed by a 30-second moment of silence. These two numbers are significant as the time symbolizes that one donor can save eight lives while the moment of silence recognizes the 3,000 North Carolinians waiting for an organ donation.
Dr. Walter Pofahl, chief medical officer for ECU Health Medical Center, said eastern North Carolina is home to a disproportionately high number of those 3,000 in North Carolina. Dr. Pofahl shared that last year ECU Health Medical Center had 31 organ donors, transplanted 90 organs while 18 were sent out for research. It also had 56 tissue donors with 141 tissues recovered and 90 eye donors with 84 corneas transplanted and 21 placed for research.
A daughter’s gift

During Wednesday’s event, Darice Fonville shared her inspiring story of donating her kidney to her mother in February.
Fonville said her mother had suffered from chronic kidney disease for about 20 years and as she began to struggle more, they learned she would need to find a donor or start dialysis. She knew that dialysis can be very difficult for patients, and she wanted to help her mother any way she could. So Darice decided to get tested to see if she would be a match.
“I was actually at work when I got the call, and they let me know we were a match,” Fonville said. “As soon as I got that call, everybody in the office already knew how excited I was. I put work on pause to go call my mom. She already knew, and she was nervous. I was excited. I knew it was a done deal. We were just going to go through with it.”

She said she never had any hesitation when she knew she could give something back to her mother and improve her life. She said the transplant team at ECU Health Medical Center put everyone at ease and allowed Fonville and her mother to be together shortly before surgery to spend time with one another.
How to give
Dr. Pofahl said while it is important to identify as an organ donor when you receive your driver’s license or state identification card, it’s just as important to share your wishes with those close to you.
“It’s not always easy, but having that discussion is important,” Dr. Pofahl said. “In that critical time when decisions are being made around donation, if your loved ones understand what your wishes are upfront and ahead of time, that makes the process a lot easier.”
While only about 50 percent of adults in North Carolina are registered organ donors, there are 3,000 people waiting for organ and tissue donations in North Carolina and more than 100,000 waiting for a donation across the country.
Learn more about how to become an organ donor and the impact you can make as a donor on Donate Life’s website.
Resources
Survivors of stroke and brain injury had an opportunity to artistically express their journey during a recent Unmasking Brain Injury event at ECU Health Medical Center.
The Brain Injury Association of North Carolina sponsored the Unmasking Brain Injury workshop. This event provides blank face masks and supplies to decorate the masks. Unmasking Brain Injury is an organization that aims to bring awareness to the prevalence of brain injuries and give survivors a voice and the means to educate others of what it’s like to live and recover with a brain injury. The event was the first of its kind in the ECU Health system.
Michele Horvath, stroke navigator at ECU Health Medical Center, helped run the event and said it was a wonderful moment to share with survivors.
“Everybody was really engaged and it was an emotional time for survivors because it made them artistically express their stroke or their traumatic brain injury and some of them are still in recovery,” Horvath said. “They’re really excited to share their story and it was really heartfelt. We’re hoping to bring community awareness to some of these brain injuries.”

Along with a support person, each attendee, many of them members of ECU Health’s Stroke Support Network, decorated a mask to represent their journey and recovery process from their stroke or brain injury.
Molly Twiss, marketing coordinator at the Brain Injury Association of North Carolina, said it was the first Unmasking Brain Injury event she’d helped coordinate and she felt inspired after the event. She explained that the masks could be anything attendees wanted, not just their brain injury or stroke, but about themselves as a whole.
“The masks are a look inside of them, what they’re feeling, what they’ve gone through, what they hope for the future,” Twiss said. “Some can be as small as their favorite TV show, their favorite color or something about what their life was like before their injury. So if they were a skier beforehand and their accident was a ski accident, they can have it ski related. The mask could represent just something to get their mind off of having this invisible injury.”
Discovering New Passions
Wendy Gardner had her first child in 2000. Ten days after her son was born in Wilson, she suffered a hemorrhagic stroke, which has affected the left side of her body.
About a year ago, Gardner joined the Stroke Support Network at ECU Health and she said she’s enjoyed connecting with people in eastern North Carolina who have had similar experiences. She said the Unmasking Brain Injury event was a positive experience for everyone and she hopes for similar events through the support group in the future.
Gardner’s mask was painted red white and blue and adorned with a gold medal, representative of her new found passion — and talent — for archery.
About three years ago, Gardner stumbled upon archery as a sport she could participate in. Today, Gardner is a member of the USA Para Archery World team.

“I hadn’t been able to find a sport that I can do because my whole left side of my body is affected,” Gardner said. “So I can’t run and I really can’t swim and do the usual activities. So I’d kind of given up actually finding something that I could do. We happened to go to a big archery competition because our daughter was interested in it. I saw a guy who has no arms and shoots with his feet and his name is Matt Stutzman. He’s on our team. That is what got me inspired. I thought, if he can do it with no arms and I have one arm I could use, we could find some way for me to do this.”
Wendy and her husband went to work on figuring out some adaptive equipment to help her hone her new craft. She said there are not many resources available to help people with making adaptive archery equipment so they went through a “trial and error” process.
Once the Gardner family got a handle on making adaptive equipment and realized how expensive it could be for others to create their own equipment, they started a nonprofit called GX4 Adaptive Archery.
Her attitude since first suffering her stroke has made all the difference. She said she never expected to be involved in something like the USA Archery Team, and through her determination to try new things—coupled with her relentless effort—Gardner now travels the world doing something she loves.
This includes trips to the United Arab Emirates, Chile and Czech Republic with the team, and she hopes to be in France next summer for the 2024 Paralympic Games.
“I’m always like, ‘Why not me?’ And I would never have done anything like this if this had not happened to me,” Gardner said. “So I always tell people, go try something new. The main thing is show up, you’ve got to show up and don’t be afraid to look foolish doing it. Because sometimes, as someone with a physical disability, you will. But just show up and try and do your best.”
Resources
Stroke Support Network – Upcoming Events
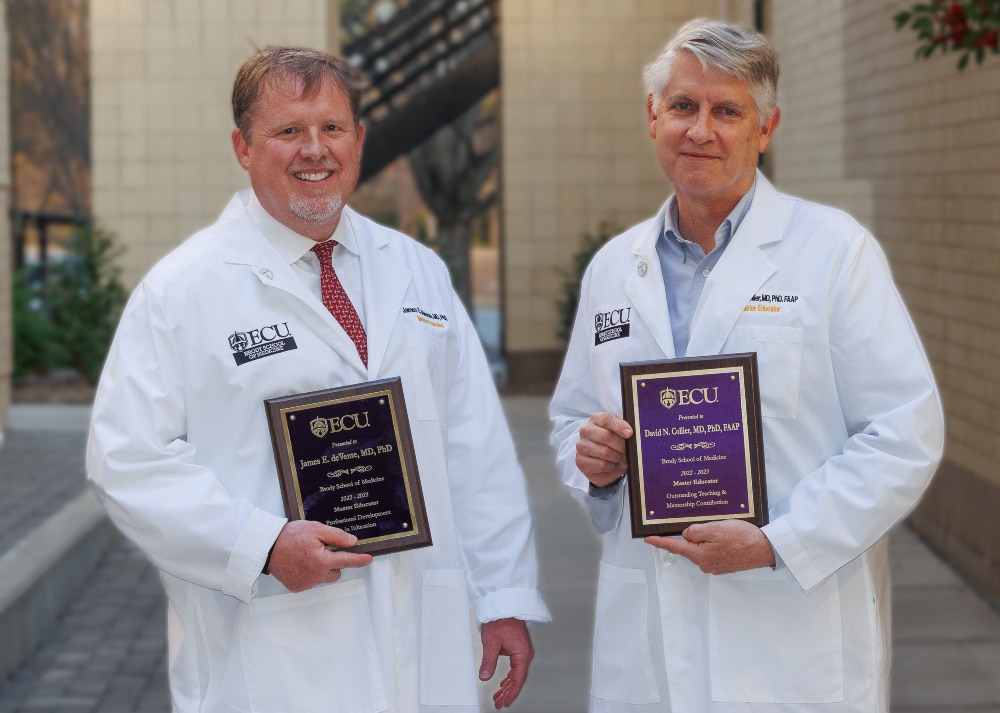
Three physicians – Drs. David Collier, James deVente and Ricky Watson – were recently named master educators by the Brody School of Medicine at East Carolina University. All three are Brody alumni.
The school’s master educator program recognizes excellence in leadership and administration, teaching contribution or mentorship, innovation and curriculum development, evaluation and research, professional development in education and educational contributions by community physicians.
The winners were announced during a Brody faculty meeting on Feb. 16, during which each winner received a white coat featuring a master educator designation, a plaque and master educator pin.
Faculty members and students may nominate faculty members to receive the award, and a committee of faculty members and students decides on the recipients.
Since the program began in 2002, close to 80 Brody faculty members have received the master educator recognition. The awards can be given in the areas of educational leadership and administration, outstanding teaching or mentorship contribution, educational innovation and curriculum development, educational evaluation and research, professional development in education and outstanding educational contribution by a community physician.
“The bestowing of the Master Educator Award allows us to honor faculty who have a sustained record of excellence in education and are who are recognized by their peers and learners as exemplifying leadership in education,” said Allison Flowers, director of Brody’s Office of Faculty Affairs and Leadership Development. “These master educators highlight how the Brody School of Medicine attracts and retains high-quality faculty who are driven by and demonstrate our mission.”
Dr. David Collier
Master Educator in Teaching and Mentorship
Dr. David Collier is a professor of pediatrics and health disparities and director of the Pediatric Healthy Weight Research and Treatment Center. He is associate director of the Integrative Health Sciences Facility Core in the NCSU Center for Human Health and the Environment.
Collier is a graduate of the Brody School of Medicine and completed his residency at Pitt County Memorial Hospital, now ECU Health Medical Center. His research interests include the prevention and treatment of childhood obesity.
Collier’s nominator highlighted his ability to share his knowledge in ways that benefit both his students and colleagues.
“David was a creative interprofessional educator before interprofessional education was a goal or mandate,” according to the nomination letter. “Dr. Collier is shown at his best — not in a classroom, not scripted — but in clinic teaching interprofessionally.”
Dr. James deVente
Master Educator in Education
Dr. James deVente is an associate professor in Brody’s Department of Obstetrics and Gynecology and is director of obstetrics at ECU Health Medical Center. At ECU since 2005, deVente graduated from the Brody School of Medicine in 2001 and completed a residency in obstetrics and gynecology in Greenville as well.
deVente has also served as the medical director for women’s services at ECU Health Medical Center since 2007 and is a trailblazer for innovation in the profession.
“In keeping with Jim’s passionate and tireless work as an educator, he has capitalized on his role to improve our entire health system through an ongoing series of faculty development opportunities,” according to the letter of nomination written for deVente. “Every obstetrical provider in our hospital system, across our portion of the state, has met with Jim for safety drills, new equipment training, fetal heart rate monitoring classes, and systemwide implementation of safety and quality initiatives – many of which he also helped to develop.”
Dr. Ricky Watson
Master Educator in Teaching and Mentorship
Dr. Ricky Watson is a clinical assistant professor and assistant residency director in the Department of Family Medicine. He is a Brody graduate and completed his residency at Pitt County Memorial Hospital, now ECU Health Medical Center. His areas of interest include women’s health, infectious diseases, travel and wilderness medicine and health care delivery systems.
Watson has earned a variety of teaching awards over the years including a Faculty Excellence Award for Excellence in Teaching and Compassion from family medicine residents. He has also received a teaching award from the American Academy of Family Physicians. He joined the ECU family medicine faculty in 2001.
“I know Ricky has delighted in helping other faculty, residents and students, new to our area, understand the needs of our patients,” reads his nominator’s letter. “He has been a steady source of education and inspiration for medical students and residents, fellows and junior faculty. He has been our go-to person for cultural competence and humility training for residents.”
Read more from ECU News Services
![Ricky Watson1[53] Dr. Ricky Watson poses for a photo after he was recently named a master educator by the Brody School of Medicine at East Carolina University.](https://www.ecuhealth.org/wp-content/uploads/2023/03/Ricky-Watson153-scaled.jpg)
By ECU News Services and ECU Health News
Getting through medical school can be tough – long hours, books and tests, and more books. However, in between classes and all-nighters, two students from the Brody School of Medicine have established a flourishing volunteer program to bring doula-like services to a region of North Carolina starved for birthing support.
The birthing companion program was started in October 2022 by Uma Gaddamanugu and Shantell McLaggan, both second-year Brody students and Schweitzer fellows. The Albert Schweitzer Fellowship supports graduate health professionals drawn from across the state who learn and work to address unmet health care needs in North Carolina.
Gaddamanugu’s and McLaggan’s fellowship project is focused on improving birth experiences of high-risk pregnant mothers in eastern North Carolina through the free birth support program to add an extra layer of support for women in the birthing process.

Patient populations in rural parts of eastern North Carolina simply need more help, Winston-Salem native Gaddamanugu said, from prenatal care through the laboring process, and certified doulas are an expensive out-of-pocket resource for which most North Carolinians must pay out of pocket because health insurance often doesn’t cover the cost.
“We are the only hospital with a high-risk labor and delivery unit for half the state. You think about how far some of these people have to travel, which makes it way harder for their support people to come with them,” Gaddamanugu said.
In February 2022, the North Carolina Institute of Medicine reported that the state’s maternal mortality rate was 27.6 per 100,000 births, which is slightly lower than the national average, but more than double the previous year’s rate of 12.1 per 100,000 births.
A 2021 study by the North Carolina Maternal Mortality Review Committee reported that 60 women died from pregnancy related causes from 2014-2016. Of those, nearly 60% were from minority racial categories and more than one in three were from rural areas. What’s more troubling – the study determined that 70% of maternal deaths could have been prevented by changing “patient, family, provider, facility, system and/or community factors.”
The program
At first, the program had 18 volunteers, but since its inception in October 2022 the ranks of birthing support volunteers have doubled to 37. At the beginning of February, the volunteers had assisted with more than 70 births, which is “way past our goal that we had initially set,” Gaddamanugu said.
Volunteers from the program come from a wide range of backgrounds, though most are medical or nursing students. Some are undergraduate students from main campus who want to be part of a program that serves the community. For now, the program is staffed almost completely by ECU students, though Gaddamanugu and McLaggan will soon hand the program’s day-to-day management off to first-year medical students who aim to open the program up to the public.
“Our program is very much modeled off a program at UNC. They’ve been doing that for about 20 years,” Gaddamanugu said. “A Wake Forest medical student started a similar volunteer doula program two years ago through the Schwitzer Fellowship. It’s just neat to see that it was possible with the structure of the organization to bring that program here, because there’s a whole different need in eastern North Carolina.”
Gaddamanugu stressed that the volunteers in the program, who support the labor and delivery services at ECU Health, aren’t certified doulas but rather are there to help during the immediate labor process. For one delivery, that might be a non-clinical, non-medical role – a friendly face and a hand to hold – and in other cases it might be running through the hospital to find a phone charging cable so a mother can stay in contact with her other children at home.
Leslie Coggins, a charge nurse on the labor and delivery unit at ECU Health Medical Center in Greenville, said the volunteer program has been a great success, both for the mothers in the delivery process as well as for students on track to become the next generation of health care providers.
“We’ve always had a great relationship with our residents, but now we have almost a pipeline — doctors, potential doctors, nurses, someone interested in birth and supporting birth in its natural function,” Coggins said. “To share that experience with up-and-coming providers and nurses who will be taking our places someday is huge.”
While the volunteer program is currently staffed by students, the student organizers and Coggins as the nurse manager of the labor and delivery unit hope to soon include members of the public. Those interested in volunteering should contact the program by emailing [email protected].
Training medical professionals

The ECU version of a volunteer birth companion program is rooted in experiences both medical students had working as volunteers in hospitals in doula-like roles. Gaddamanugu volunteered during her time as an undergraduate at UNC; McLaggan, who is from Thomasville, spent several years after her undergraduate education working at the Cherokee Indian Hospital in western North Carolina and helped establish a volunteer doula program there.
Both students are interested in pursuing a career in obstetrics.
McLaggan’s mother told her from an early age that she was smart enough to be a doctor. After researching the requirements and being captivated by the science of medicine, she fell in love with the idea.
“I feel like I have the mental, emotional and the physical capacity to do something as strenuous as being a doctor,” McLaggan said. “Because I have those qualities, I feel like it’s my obligation to become a doctor and serve people to the maximum of my abilities.”
Medicine was also a calling for Gaddamanugu, who said that the challenge is humbling but she sees a future where she can make a difference by “maternal and child health disparities in our community” which fit the impact that she hopes to make in the world.
She said that the experiences at the bedside have colored the conversations that she has with her medical school peers about the experience of medicine from the patient’s perspective.
“We know birth is hard, but here is what it really can look like,” Gaddamanugu said. “The U.S. has an awful maternal mortality crisis, and we can hear those numbers all day long in school, but the numbers don’t mean anything until you see it in person, and you realize some of these patients are extremely sick.”
For Dr. Kerianne Crockett, ECU Health OB/GYN and Brody clinical assistant professor, the program has clear benefits for the patients she serves. She has heard from patients who appreciated having another source of support during their delivery.
“Delivering a baby is one of the most exhausting, exhilarating, sometimes scary experiences of a patient’s life,” Crockett said. “There is good evidence that patients with a continuous support person present throughout labor — whether that person is a family member, a spouse or a doula — have better birth outcomes, including lower rates of cesarean delivery. I am so proud that our bright, compassionate, empathetic medical students are now able to be that continuous support person for all kinds of patients, including those who otherwise would not have had anyone besides the medical team there for their delivery.”
Student involvement in health care delivery, and the unique perspectives students offer patients, is a hallmark of a large academic health system like ECU Health. As students learn from the clinical experience of providers at ECU Health, they are empowered to innovate and bring ideas to the table that lead to better patient experiences and brighter outcomes.
“As an academic health system, our medical students help to enrich the patient experience with their energy and ideas,” said Angela Still, senior administrator of women’s services at ECU Health Medical Center. “The birthing support volunteer initiative is a great example of how Brody students go beyond the walls of the classroom and make a direct impact on the patients we’re proud to serve.”
Serving eastern North Carolina
Sometimes the most important support that a birthing companion can provide comes from skills that can’t be taught in a formal doula class.
McLaggan remembers one time she volunteered with a woman who had a number of kids already — the most recent born by C-section. The medical staff recommended another C-section, which the woman was reluctant to agree to due to the complications she had with the previous birth. The challenge that McLaggan was able to help resolve wasn’t convincing the woman to have a C-section, but rather just communicating with her at all. The woman was Haitian and spoke Haitian Creole and little English.
“I happened to speak French, which is very similar to Haitian Creole, so she was able to communicate to me, where she was coming from and what her needs were,” McLaggan remembered. “I was able to bridge that gap and she ended up delivering naturally. I felt so honored and privileged to have been in the room.”
Another of the volunteers in the program has similar experiences with language gaps being a hindrance to quality health care. An undergraduate student recounted to Gaddamanugu how, growing up in eastern North Carolina, she was always saddled with translating for her mother and siblings during medical appointments — a task that shouldn’t really be shouldered by a young person. The student volunteer said, though tears, that she was so grateful to be able to translate for delivering mothers because she knew first-hand the constricting fear and anxiety of being language-locked in a stressful medical situation.
While the language capabilities that some students bring to the hospital bedside are important, Coggins said, patient populations in eastern North Carolina are getting sicker, which often requires the health care team members to devote their attention to the physiological status of the patient.
“We try to promote natural delivery as much as we can,” Coggins said, but sometimes the medical conditions of the mother and baby require doctors and nurses to focus on the immediate illness. “One-on-one support is essential with our patients. A lot of times our sick population are not from around here and don’t have the support system in place, so this is an added benefit so our nurses can focus on what is medically happening and where we need intervene.”
Gaddamaugu is awed at the privilege of being present at a birth.
“I’ve cried every single time; it’s one or two single tears, but they were C-section babies and you could sense the relief in the OR the moment the baby comes out safe and healthy,” Gaddamaugu said.
McLaggan has known that being in the room during the birthing process is what she has wanted to do since before kindergarten. She’s seen a handful of births as a volunteer and continues to be amazed by each one.
“Words don’t describe how amazing childbirth really is. I get so overwhelmed with emotion when I see 37 to 40 weeks of work and love going into this child that is coming into the world,” McLaggan said.
Resources
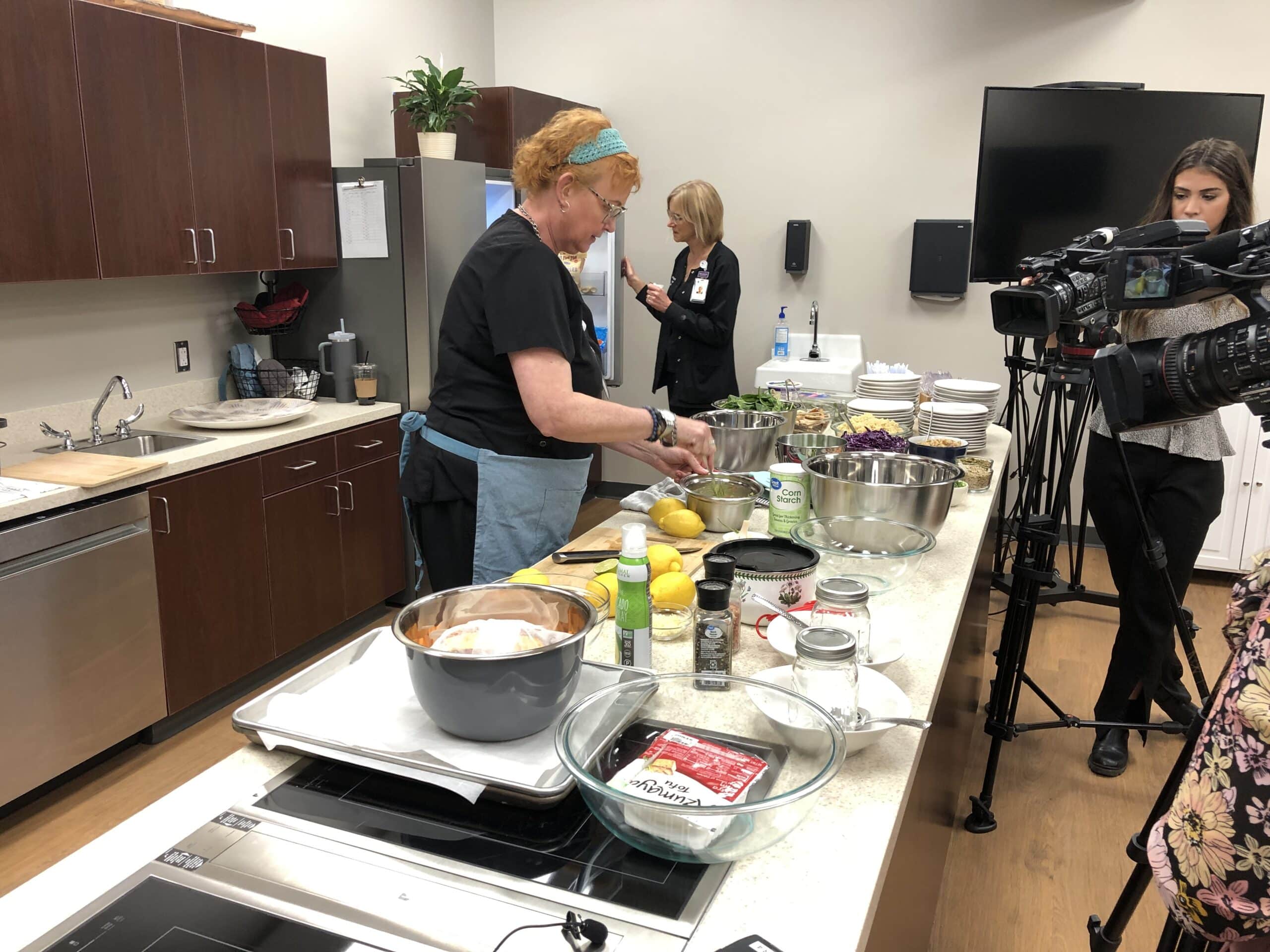
ECU Health hosted an open house on March 7 to introduce community members to the newly dedicated space for the Lifestyle Medicine Clinic located in the ECU Health Wellness Center in Greenville.
The Greenville location is one of 12 across eastern North Carolina, designed to help patients live a healthier life through improved nutrition and exercise.
Dr. David Michael, medical director for the Lifestyle Medicine Clinic, said the space is a dream come true for him and the patients he serves.
“I’ve always dreamed that my physician’s office or doctor’s office would look more like a fitness center than a hospital,” Dr. Michael said. “I thought if I could do that, I’d be onto something. So it’s just a blessing to have the lobby of our Lifestyle Medicine Clinic right in the fitness center itself. Exercise and physical activity are such important pillars to healthy living.”
There are six traditional pillars to healthy living that the clinic follows in its work with patients. Those pillars are:
- Healthy eating, including whole, plant-based foods
- Increased physical activity
- Develop strategies to manage stress
- Avoiding risky substances
- Improved sleep
- Form and maintain relationships
Brenda Leigh, director of Lifestyle Medicine at ECU Health, said the program is designed for each individual patient, and the patient’s wants and needs dictate how the program is developed.
“A lot of times people will start with one pillar and try to figure out what’s most important to them, and sometimes it might not even be what they think,” Leigh said. “They come in and say, ‘We want to lose weight.’ After the navigator talks with them for a bit, we realize all the stressors going on in their life. So we might say, ‘First, you really need to work with a social worker or a counselor and set some priorities and get some things ready in your life to then make the nutrition and exercise changes that might help your weight loss.’”
During Tuesday’s open house, the Lifestyle Medicine team also hosted a free “Lunch with a Doctor” and “Dinner with a Doctor” event. During these sessions, ECU Health providers cooked a healthy meal for participants, showed them how to prepare the meal and shared ways to get whole, plant-based foods into their diet.
Susie Houston, a nurse practitioner with ECU Health, prepared the meal for the “Lunch with a Doctor” event. She said educating attendees and showing them how to cook a tasty meal with the ingredients that typically get left behind in the grocery store is a priority during these events.
For lunch, the team put together a power bowl with tofu, vegetable toppings and a homemade dressing that attendees could choose from.
“When you think of the color of the rainbow with what we’re preparing today, you’re pretty much getting all the vitamins, minerals and then fiber that you need,” Houston said. “So if we use food as medicine, it’s this great idea that in the grocery store, if we could stick in the produce section or the perimeter in the store, that just makes a difference.”
The team plans to continue to host these free events in the future.
Leigh said she knows this program can change lives for patients as studies have shown healthy habits like diet and exercise can help slow, stop or even reverse chronic health conditions like diabetes and heart disease.
March is National Nutrition Month – start your journey to better health with the Lifestyle Medicine programs available across eastern North Carolina by calling 252-847-9908.
Resources
In a ceremony laced with excitement, anticipation and tradition, fourth-year medical students in the Brody School of Medicine at East Carolina University learned where they will spend the next three to seven years completing residency training.
The March 17 event marked a milestone for the Class of 2023, whose medical school journey included the historic events of learning through the COVID-19 pandemic and the integration of Brody and then-Vidant Health, which became ECU Health in 2022.
Match Day is arguably the pinnacle of medical school, when students discover their next destination surrounded by friends, family and Brody faculty and staff who have guided them over the years. Michael Waldrum, dean of the Brody School of Medicine and CEO of ECU Health, said that wherever the students are matched, they already have a reputation of being health care providers who put the individual patient at the center of their practice.

“Brody students come out of medical school knowing how to do hard work and take care of humans. It’s a very hands-on practical education. They learn how to take care of people which is what becoming a doctor is all about, and the experience they get here sets them apart,” Waldrum said.
The students were presented to the audience of family, friends and members of the Brody community with collages of photos along with music that each selected.
Kari Beasley, from Cary, wanted to use the song “Soulful Strut” from the movie “The Parent Trap” — but only if one of her mentors, Jason Higginson, agreed to learn the handshake from the movie and perform it on stage with her.
Beasley, who matched with Virginia Commonwealth University in Richmond to pursue an obstetrics and gynecology track, said that both Jason Higginson, the executive dean of Brody, and his wife Amanda Higginson, Brody’s interim associate dean for student affairs, were an important part of her medical school experience.
“Being the amazing dean that he is, he said, ‘Of course, absolutely, I’ll do the handshake with you.’ Today, we pulled it off,” Beasley said. “It made it more special that he and I got to do the handshake together because the Higginsons have been a great part of my experience here at Brody.”
While Higginson had seen the movie, he didn’t remember the handshake and dance until she showed him the clip.
“She asked me if I would do it with her and I said you’re really challenging an old man with no rhythm. We practiced it yesterday in my office and then I practiced it with my daughter all night last night,” Higginson said.
The relationships that he and fellow faculty members build with their students is unique because he didn’t have interactions with the administration when he was in medical school.
“This is probably one of the best days in the life of a medical school. This is the day where all of your dreams get realized,” Higginson said. “A lot of them are staying here, which is something we are proud of. Almost 50 percent of the class is staying in North Carolina and that’s fantastic. That’s our mission.”
The Class of 2023 is a snapshot of Brody’s mission to serve the state. The 77 members of the class represent more than 25 North Carolina counties, from Buncombe in the west to Pasquotank in the northeast.
With envelopes in hand that revealed their futures, the students took time to celebrate their accomplishments and reflect on what comes next.
‘What small change can I do?’

When there’s a problem, Merdi Lutete is busy seeking a solution.
Lutete, who was born and raised in Kinshasa, Democratic Republic of Congo, has the mindset of not standing by and expecting others to act — instead, she wants to know how she can help and how her skills and knowledge can lend to a long-term resolution.
“With a lot of issues we encounter, we see a problem and we say, ‘Well, someone else can do it,’” she said. “What’s helped me has been that mindset of, ‘Well, there’s a problem. What can I do about that? I’m probably not even going to get to the surface of the issue, but what small change can I do for this?’”
Lutete has used that formula throughout her life, including medical school. Lutete founded I Am First, an organization that partners first-generation medical students with mentors who can guide them through the medical school process.
“I think it will definitely contribute a lot,” she said. “I was able to apply it to school and I can put it to other areas too, and medicine as well.”
Lutete matched in adult neurology at Duke University Medical School in Durham. As she opened her Match Day envelope, she was surrounded by family and friends, some whose smiles shown through phone screens. Her hands shook as she revealed the folded paper printed with her next destination.
“I was nervous,” she said, laughing as those around her cheered, “but I feel good.”
Lutete studied neuroscience at ECU during her undergraduate years; she initially became interested in neurology in high school, when she took a psychology course and witnessed her father face a health challenge. His doctor was careful to include the family in medical conversations and make sure they understood the situation and options.
“That personal thing really touched me a lot,” she said. “I really wanted to do something like that with patients as well.”
Seeing her own family go through a health challenge and now having the perspective of a student doctor helped Lutete better understand the sacrifices her family and community have made to help her get where she is today. Her parents moved the family from Kinshasa to Raleigh in 2005 to pursue more opportunities. The Congolese community in Raleigh has also rallied behind Lutete and her success. Lutete worked with other students and Brody faculty and staff on an initiative to share information with the families of medical students so that they better understand the process their students will experience in the coming years. It was her way of acknowledging the village that it takes for students to succeed.
“It truly means a lot to them and a lot to me to see that,” she said of the support she’s received from those around her. “One thing about first generation that I really think is powerful is that you’re standing on the backs of many people’s sacrifices. You know that the successes you have you can’t attribute to yourself because you know every single person had a role in that. You’re literally standing on the backs of other people’s sacrifices.”
When Lutete thinks about community, she thinks about how Brody has prepared her for her next steps.
“Brody does a great job of teaching you how to care for the individual, how to care for the patient that you’re seeing in front of you,” she said. “I can give you a prescription for medication, but can you afford it? I can tell you to come back next week for an appointment, but can you afford to come back? Brody really teaches you how to think about the patient and how their story applies to the situation.”
Success found through love, teamwork

When you start off down an arduous path, it’s good to have a friend by your side. When that friend ends up being the person you fall in love with and plan to keep walking life’s paths hand in hand, all the better.
The first week of classes at the Brody School of Medicine in the fall of 2019, Bethany Laden and Caleb Oakley were out with mutual friends working through the awkwardness of meeting the classmates you’ll share the next four years with. He bought her a drink, she told him her favorite book was The Great Gatsby (from which he quoted the last line — smooth) and Bethany said, “we’ve been together ever since.”
Laden was raised in an Air Force family and lived in England and Guam, but mostly in Harrisburg, near Charlotte. She studied biology at NC State and initially intended to apply for a physician assistant program but applied to Brody after graduation. She spent a year as a medical assistant and two years of conducting urology research in Durham. Witnessing a baby being delivered set her mind to being an obstetrician and gynecologist.
“I really like working with my hands — being in the operating room and doing surgery. When I was on my women’s health rotation that’s where I found my passion — working with women, empowering them through their pregnancies and the rest of their lives,” Laden said.
Oakley is from Roxboro and knew he wanted to be a doctor since high school. A teacher showed the movie “Chernobyl Heart,” which chronicled missionaries who fixed the cardiac conditions faced by children who were affected by the Chernobyl disaster. Oakley’s family was particularly religious and did missionary work along the east coast and the film inspired him to be the same kind of doctor who helped people who needed the most help.
He worked as a medical scribe in high school, and then again during his undergraduate education at ECU, where he double majored in biology and chemistry. His first application to medical school didn’t work out, so Oakley taught as a substitute, trained to be a paramedic, worked on food trucks across eastern North Carolina and even prepped alligator meat at a seafood company in Morehead City.
Oakley’s intended career path lies at the other end of the birthing process from Laden. As a doubled-board certified doctor working in internal medicine and pediatrics, he’ll be able to treat patients across the continuum of birth to death.
“They tell you when you start medical school that you’ll find your niche. I had a really good experience out at ECU Health-Duplin which confirmed it for me,” Oakley said.
Early in their relationship they agreed that school would come first and “I’m not going to let you distract me,” Laden remembered. But before long, when she finished studying at 11 p.m., she would try to track him down in the Brody building.
Their relationship took some work, because relationships on their own are difficult Oakley said. Layering the physical, mental and emotional challenges of training to be a doctor on top of creating a new life with another person makes things even more challenging, but with great challenges come great rewards.
“I don’t say this all the time, but she’s my rock. If I feel I need to lean on somebody, I’m going to her,” Oakley said.
Laden agreed. Having someone in her corner, someone who understands the specific challenges of medical school, has been invaluable.
“There’s so much that we go through that people don’t understand,” Laden said. “Not just the logistics of how medical training works, but the terminology and the emotional work that you have to do.”
Match Day is incredibly stressful for any medical student — will you get the hospital you want? Will it be on the other side of the country? For a soon-to-be-married couple, the stressors compound — would they be assigned to hospitals close together or separated by circumstance?
Laden and Oakley interviewed at more than a dozen of the same hospitals to find a place that could support both of their training paths. When they opened their envelopes, surrounded by their families, the learned their residency would take place at ECU Health Medical Center in Greenville.
“Both of our families live in North Carolina, so we don’t have to worry about moving and we’ve already set up a good sense of community,” Oakley said. “It feels like home.”
The art of emergency medicine
Andrés Gil had graduated from Winthrop University in South Carolina when he came upon an opportunity to be a medical interpreter at a hospital near Charlotte.
The talented violinist was preparing to audition for orchestras and embark on a classical music career when another type of art caught his eye. During his experience as an interpreter, he witnessed a baby being born.
“I remember I was interpreting, the lights were down in the room, it was the early shift so the sun was a nice orange glow lighting up the whole room, and everything was going well,” Gil said. “All of sudden you just hear this cry. It was like art. Watching life come into the world was amazing.”
Gil, who was born and raised in Colombia, made his way to the Brody School of Medicine from there, after selecting the school based on its small class size and its community focus. After realizing he was on the path of his purpose, he began to immerse himself in service and making a difference in others’ lives.
“I never pictured myself as a student doctor in eastern North Carolina,” he said. “It was just never on my radar.”

Gil has flourished, becoming close with his classmates and being inducted into the Gold Humanism Honor Society, a community of medical students, physicians, and other leaders who have been selected by their peers for their compassionate care. Gil was surprised to be named to the group but wants to continue on the path that earned him the recognition.
“The people I get to share that honor with are all beautiful human beings,” he said. “I like having that in my wheelhouse for others to know that this is an opportunity to highlight your career.”
Gil matched in emergency medicine at Carolinas Medical Center in Charlotte. When he opened his Match Day envelope, tears filled his eyes and he couldn’t speak. A tight circle of family members teared up as well, cheering when he was able to reveal his next stop.
“Charlotte?!” a colleague passing by exclaimed.
“Yes, yes!” Gil nodded, overcome by a fresh burst of tears.
Emergency medicine felt like the right fit for Gil, who has learned to temper his expectations as he went through medical school, hoping for the best but understanding that contingency plans are important to have in place. The specialty also drew him in because of his overwhelming passion for helping people and healing patients who seek him out for assistance.
“Anyone who comes through those doors is not at a great point in their life,” he said, “whether they have pain, addiction, substance abuse, a car accident or things aren’t great at home. These people humble themselves enough to come and seek our help. Knowing that I have an opportunity to somehow have an impact on their lives moves me to a degree that I really can’t describe.”
As Gil prepares to leave Greenville and head west for the next chapter in his story, he hopes that what he’s learned at Brody will help add vitality to his patients’ stories as well.
“An opportunity to give someone grace, to restore their dignity, is so important to me,” he said. “It makes all the scary things about emergency medicine go away. That moment gives you an impetus to work harder to restore this person, so when they leave, they can go back to their life and complete their narrative.”
Read more from ECU News Services.
More than 100 ninth grade students from Pitt County Schools and Duplin County Schools attended ECU Health’s career fair for Health Sciences Academy students on March 2. Over 20 hospital departments and exhibitors from partners including Pitt Community College and Beaufort County Community College attended the event which included interactive and creative booths to educate students on different health care careers.
“Health Sciences Academy offers high school students the opportunity to explore different careers in health care and receive real experiences in the health care setting,” said Nancy Turner, program coordinator, Workforce Development, ECU Health. “Presenters in the career fair were able to tell students their career path, including where they went to school, how long degree programs take and degree/certification requirements for their careers.”
The Pitt County Health Sciences Academy is a partnership between ECU Health, Pitt County Schools, Pitt Community College, East Carolina University, the Brody School of Medicine, Colleges of Allied Health Sciences, Engineering and Nursing at East Carolina University, School of Dental Medicine at East Carolina University, the Eastern Area Health Education Center and the Greenville-Pitt County Chamber of Commerce.

The Health Sciences Academy originally launched at six high schools in Pitt County in 2000 and has expanded across schools in Pitt County and in Duplin County. Last year alone, 282 students completed the program and were awarded more than $3.9 million in scholarships to help on their health care career journeys. Those students completed 106,225 volunteer hours at ECU Health.
“Health Sciences Academy allows for ECU Health to develop our workforce locally with students who are passionate about health care and helping people,” said Turner. “One of the most exciting things about the career fair was seeing a former Health Sciences Academy student who volunteered at the hospital and graduated from the program. She completed nursing school at Pitt Community College and ECU. She is now a pediatric nurse at ECU Health and managed a booth at the career fair to tell students about her experience. It truly has come full circle.”
During high school, Health Sciences Academy students complete a minimum of six courses that expose them to potential health care careers and prepare students to pursue college-level health science programs upon graduation. They participate in job shadowing, mentoring, internships, medical research opportunities, career exploration and volunteering.
Students say they participate in the program because they have an interest in working in health care. The career fair taught some students about health care careers they had never heard of or considered. The ninth graders who attended the career fair will soon have the opportunity to volunteer and shadow in those fields.
“Many students here in Pitt County and in Duplin County attend community college and universities locally and end up staying and working at ECU Health,” said Turner. “We are really growing our own workforce. That’s why we created Health Sciences Academy.”
To learn more about Health Sciences Academy in Pitt County Schools, please click here; for Duplin County Schools, please click here.
Greenville, N.C. – ECU Health CEO Dr. Michael Waldrum issued the following statement:
“This is an important moment for rural health care in North Carolina as our legislators have struck a deal to move Medicaid expansion and the Healthcare Access Stabilization Program (HASP) forward in the legislative process and one step closer to passage. Medicaid expansion will provide coverage to more than 100,000 people in the East and HASP is vitally important to stabilize health care delivery in rural North Carolina. On behalf of ECU Health and the communities we are proud to serve, I extend my deepest gratitude to our elected leaders for this important development and we look forward to it becoming a reality. While this won’t solve all of the challenges we face in rural health care, this is a critical and necessary step.”

Resources
Mental health in the United States has been an ever-escalating problem for many years that has now become markedly worse due to the COVID pandemic. Fear, anxiety and isolation stemming from the pandemic exacerbated depression, substance abuse and even the incidence of spousal abuse.

Dr. Michael Lang
In my role as chair of the Department of Psychiatry & Behavioral Health at the Brody School of Medicine and ECU Health, I have seen firsthand the impact a lack of mental health resources can levy on our most vulnerable citizens. Others in our community see and experience it as well, as evidenced by the large turnout and lively conversation at the Mental Health Town Hall hosted by the North Carolina Department of Health and Human Services in Greenville on Feb. 9. The themes and stories shared at the town hall were common, consistent and heartbreaking. I am grateful for the legislators and community members who came together to have an open, honest discussion and we all agree that urgent action is needed.
Emergency departments across the state are overrun with patients in psychiatric distress with few outlets available to provide them help. This has particularly been the case for patients with substance abuse disorders, our elderly and children. I personally have seen so many children in the emergency department that doctors had to treat other conditions in the waiting room. We owe our patients appropriate mental health services in a safe location with qualified professionals who are not only delivering excellent care but training the next generation of providers to take up the mantle of behavioral health care.
To that end, ECU Health’s partnership with Acadia Healthcare to build a new 144-bed freestanding mental health hospital here in eastern North Carolina is a step in the right direction. This facility, scheduled to open in 2025, will provide state-of-the-art care for not only the people of our region but also the entire state. The hospital will house distinct units that will be devoted to the care of specific populations of behavioral health patients. Included will be a geriatric unit, a substance abuse area, a space for those with significant co-morbid medical problems, the intellectually disabled and a 24-bed child/adolescent unit. Within its walls, every evidenced-based treatment available will be utilized to maximize our ability to rehabilitate, stabilize, and allow our patients successful community reentry.
Given the large number of disparate patients with varied diagnosis, the new behavioral health teaching hospital will serve as a training area for physicians, nurse practitioners, physician assistants, psychologists, occupational therapists, family therapists, substance abuse counselors and more. The hospital will be closely aligned with ECU Health Medical Center for access to the wide array of clinical and diagnostic resources our tertiary care center has to offer.
Our vision is for this facility to serve as a symbol of the commitment we at ECU Health and the Department of Psychiatry and Behavioral Medicine have to provide state of the art care for the people of eastern North Carolina. I am excited to form new partnerships and engage our community leaders to ensure that all citizens, whether they have schizophrenia or opiate use disorder, can live and prosper here in our wonderful region.
Michael Lang, MD, is chair of the Department of Psychiatry & Behavioral Health at the Brody School of Medicine and ECU Health.

