Ahoskie, N.C. – ECU Health Roanoke-Chowan Hospital has earned recertification as a primary stroke center by The Joint Commission and the American Heart Association/American Stroke Association, recognizing the hospital’s preparedness and expertise to care for stroke patients.
“I am proud of ECU Health Roanoke-Chowan’s team members and their commitment to provide high-quality stroke care to our patients and community,” said Brian Harvill, interim president of ECU Health Roanoke-Chowan, president of ECU Health Chowan Hospital and ECU Health Bertie Hospital. “Our hospital’s stroke recertification as a primary stroke center from The Joint Commission – and stroke readiness at each ECU Health hospital – represents ECU Health’s dedication to bringing a comprehensive stroke network to care for all patients across eastern North Carolina.”

Stroke is a leading cause of death in North Carolina and the leading cause of long-term disabilities. As a primary stroke center, ECU Health Roanoke-Chowan can treat and stabilize patients experiencing an acute stroke and care for more complex cases. Located in Ahoskie, North Carolina, ECU Health Roanoke-Chowan serves a rural community and is the closest emergency department for surrounding communities. As a resource for emergency care, ECU Health Roanoke-Chowan’s recertification ensures local community members have access to timely stroke care and extends the comprehensive stroke network capable of meeting the needs of all patients across eastern North Carolina.
The likelihood of having a stroke in North Carolina is significantly higher than the rest of the country as a whole. North Carolina is about 8 percent worse for stroke mortality than the national average, and in eastern North Carolina, that risk is even greater.
“Time is the most important factor when treating a stroke, so it is critical to provide stroke care close to home,” said Dr. Barry Bunn, regional emergency department medical director, ECU Health. “With eastern North Carolina’s high rates of stroke, ECU Health Roanoke-Chowan’s stroke recertification, combined with a network of stroke readiness at all ECU Health hospitals, reduces the time of treatment, the risk of mortality, permanent brain damage and other side effects including memory loss, difficulty speaking and potential paralysis.”
During the certification process, ECU Health Roanoke-Chowan was evaluated on performance measures in stroke care, including education for patients and families on stroke risk factors and recognizing symptoms of stroke. Other performance measures included staff education on stroke protocols and the appropriate prescription of medications to address stroke risk factors such as elevated cholesterol and blood pressure.
Roanoke Rapids, N.C. – The Joint Commission and the American Heart Association/American Stroke Association has recertified ECU Health North Hospital as a primary stroke center by recognizing the hospital’s preparedness and expertise to provide timely and high-quality care for stroke patients.
“I am grateful to our team members across all levels and services for their commitment and diligent work that allows ECU Health North to continue to be designated a primary stroke center,” said Jason Harrell, president of ECU Health North Hospital. “Providing high-quality stroke care close to home is central to our mission of improving the health and well-being of eastern North Carolina. We are proud to be part of the top-notch neurological services provided at ECU Health across the region, which includes a strong network of expert stroke care.”

Stroke is a leading cause of death in North Carolina and the leading cause of long-term disabilities. According to the North Carolina Department of Health and Human Services, both Halifax and Northampton counties have higher incidences of strokes compared to the North Carolina average. As a primary stroke center, ECU Health North can treat and stabilize patients experiencing an acute stroke and care for more complex cases. As part of stroke readiness by all hospitals in the ECU Health system, this certification is symbolic of a comprehensive stroke network capable of meeting the needs of all patients across eastern North Carolina.
The severity and likelihood of having a stroke in North Carolina is significantly higher than the rest of the country as a whole. North Carolina is about 8 percent worse for stroke mortality than the national average, and in eastern North Carolina, that risk is even greater.
“Immediate treatment of strokes can minimize the long-term effects of a stroke and even prevent death,” said Dr. Barry Bunn, regional emergency department medical director, ECU Health. “With our region’s high rates of stroke and mortality from stroke, ECU Health North’s stroke recertification demonstrates our proven results of reducing the time of treatment, risk of mortality, permanent brain damage and other disabilities.”
During the certification process, ECU Health North was evaluated on performance measures in stroke care, including education for patients and families on stroke risk factors and recognizing symptoms of stroke. Other performance measures included staff education on stroke protocols and the appropriate prescription of medications to address stroke risk factors such as elevated cholesterol and blood pressure.
On a February morning, Vietnam veteran Lee Pascasio sat in his brother-in-law’s room on 2 East at ECU Health Medical Center. As Melissa Warren, a nurse on the unit, checked on Willis Johnston Stancill she noticed his blood pressure was spiking, and the team sprung into action.
Pascasio said he watched in silence as the team went to work saving Stancill’s life. He said he’d seen that kind of teamwork before in his time as a Marine. The experience moved Pascasio to gift his Navy Commendation Medal, earned during his service in Vietnam, to Melissa Warren and the rest of the 2 East team. Now, it hangs in the hall of the unit on top of the stars of the American Flag for all to see.
“This is such a great team,” Warren said. “It’s such a well-oiled machine, it’s like we’re dancing almost when something crazy like that happens. It’s not like you have to ask somebody to do something. We just kind of do it, that’s the team. If something happens, the troops are coming in.”
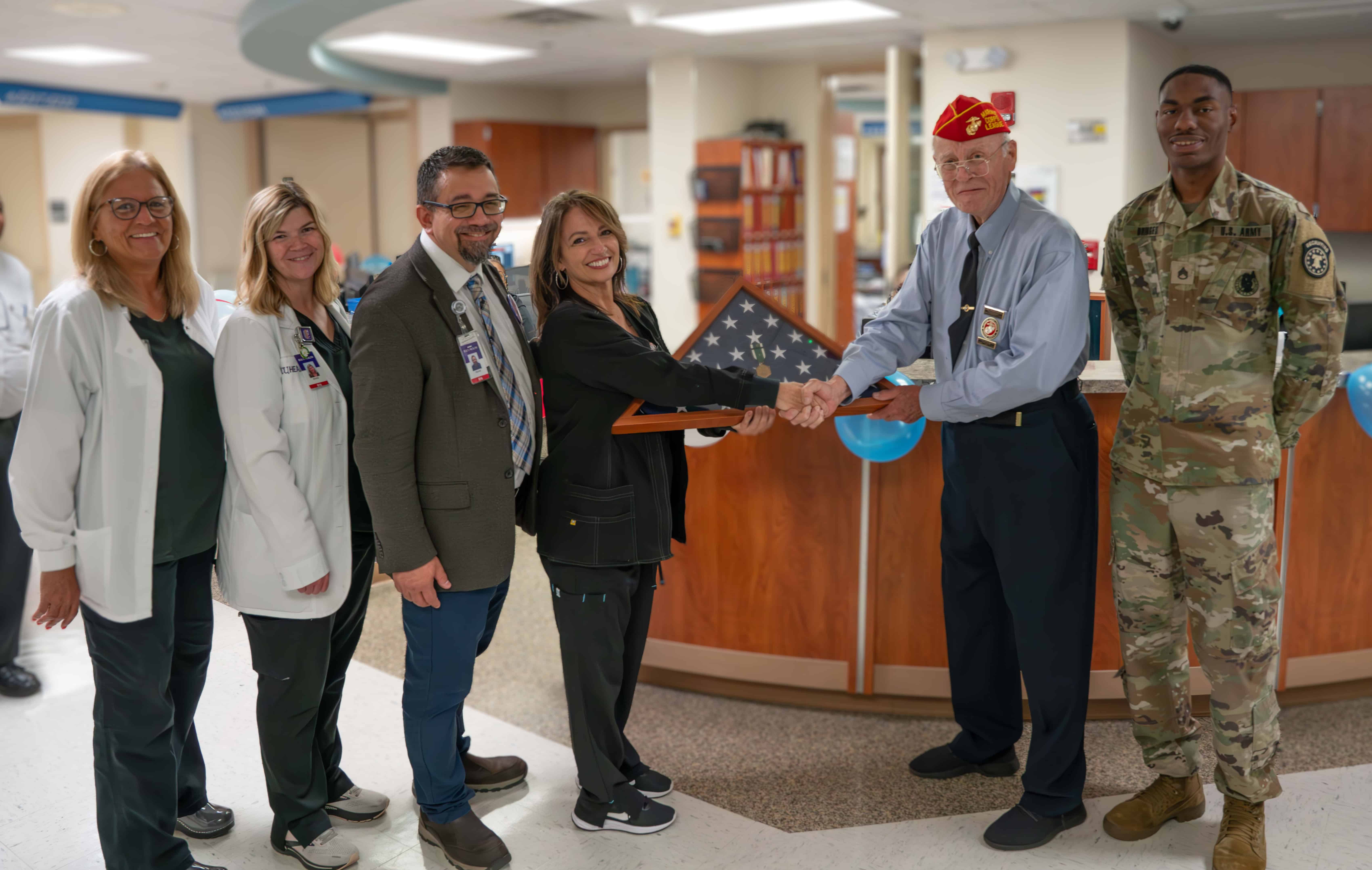
A Medal Earned
Pascasio recalled his time in Vietnam vividly. During his second tour in Vietnam, Pascasio said at 25 years old he was an old man compared to the rest of the First Battalion, Ninth Marine Unit, where he served as sergeant, specializing in explosives.
On June 30, 1969, Pascasio said he was at Vandegrift Combat Base with the Ninth Marine Unit and another platoon in Vietnam. That day, rockets and mortars began to hit the battalion without warning. A lieutenant was killed in the attack, leaving Pascasio in charge. Pascasio sent a sergeant to get a corpsman while he administered first aid to the wounded. When the medevac eventually arrived, Pascasio helped load the dead and wounded Marines so they could receive further care.
Two years later, Pascasio was presented with the Navy Commendation Medal at Camp Lejeune.
Appreciating a Care Team
In the days following his brother-in-law’s incident on 2 East, Pascasio shared his appreciation in the form of tacos, donuts, coffee, cheesecake, Cracker Jacks and other snacks.
“He’s just so appreciative,” Warren said. “I can’t give like a superhero story or anything about that night. It was what we do. It’s nice to have him, or anybody, recognize what we do. It’s a demanding job with your emotions, high energy, physically, everything. So it is nice for somebody to care that much when we’re just doing our job.”
For Pascasio, the treats weren’t enough to show his appreciation.
 “I said, ‘You know what? I want to do something nice for these people.’ They just saved my brother’s life. He got the best care in the world right here at 2 East,” Pascasio said. “I thought about Melissa and her team of crackerjacks on 2 East and I said, ‘This medal isn’t going to buy her a cup of coffee, but it’s straight from the heart.'”
“I said, ‘You know what? I want to do something nice for these people.’ They just saved my brother’s life. He got the best care in the world right here at 2 East,” Pascasio said. “I thought about Melissa and her team of crackerjacks on 2 East and I said, ‘This medal isn’t going to buy her a cup of coffee, but it’s straight from the heart.'”
“It was about their teamwork to save a life and the concern that we should all have. The nurses and teachers who have been through COVID are overlooked.”
Stancill passed away in May, but Pascasio said he still lives in his heart and in the heart of his wife, Emily Pascasio. He continues to be grateful for the care Stancill received, which Warren and her colleagues continue to find meaningful.
“This is for the whole unit,” Warren said. “I mean, you see the support of all the staff out there. They’re amazing. We are like family. When I come to work, when I walk in, we’re hugging each other. None of us could do this alone.”
Independence Day is celebrated across the country with cookouts, family gatherings, fireworks and more. While fireworks are a fun way to celebrate, they can be dangerous if not handled by professionals and can cause serious harm including devastating burns and other injuries.
More than 3,000 children under the age of 15 are sent to the emergency room each year in the United States because of fireworks, according to Safe Kids. During July 4 celebrations, it is important to remain mindful of safety and injury prevention while enjoying festivities, particularly those involving fireworks.
Ellen Walston, Injury Prevention Program coordinator at ECU Health Medical Center, said firework injuries are far too common, including those that can be sustained from sparklers.
“We have an extended holiday weekend, but we want to send the important message to let the professionals handle the firework displays,” Walston said. “Some children really enjoy using sparklers but we just ask that you use extra caution because the tips of those sparklers can exceed 1,200 degrees and cause a third degree burn.”

She said supervision of children is key when using sparklers and to make sure they are fully distinguished after use by pouring water over the sparkler, as they can still run around 450 degrees after they are finished burning. Walston said glowsticks are a safe alternative option.
From 2018-22, Walston said there were 11 admissions to ECU Health Medical Center for firework-related injuries. Typically, she said, the injuries are to hands and fingers and the most common age group is 20-29.
“Any time that you are in a situation where there are fireworks involved, we ask that you provide very close supervision to any children, don’t let them near the fireworks,” Walston said. “We want everyone to have fun with their families but it’s so important to do so safely and that starts with supervision.”
Leaving a child, senior or pet behind in a car can pose serious danger, even if it’s just for a few minutes.
That was the message of the hot car safety event hosted by Ellen Walston, Injury Prevention Program coordinator at ECU Health Medical Center, along with the Martin-Pitt Partnership for Children, Pitt County Sheriff’s Office, Safe Kids North Carolina and Greenville Fire Rescue.
Walston said it’s dangerous for anyone to be left alone in a vehicle because of how quickly they can heat up, especially for children.
On June 29, Walston and community partners shared the information in the parking lot of Kohl’s in Greenville. During a somewhat overcast afternoon with temperatures around 90 degrees, it took about 15 minutes for the display car on hand to reach 123 degrees inside.
“Our campaign is never leave your child alone, not even for one minute,” Walston said. “That means when you think you can just run in and do a quick errand in the store or any situation, we don’t ever want a child to be left alone in a car, not even for a minute. That also includes our senior adults and pets.”

Walston said leaving the windows cracked for a child, pet or senior with the engine off is not enough ventilation to be safe, and even leaving them in the car with the air conditioning on can pose dangers.
During the event, Walston and team demonstrated how the heat inside vehicles can literally cook s’mores by roasting them on the dashboard. She said there have already been eight deaths in the United States this year from children being left alone in cars. While there have not been any in North Carolina this year, the state had four of the 33 national deaths last year.
“One death is too many, that’s why we’re out here today educating the community,” Walston said. “The car we have out here today actually has a feature that has a reminder to check the backseat when you turn off the engine. It’s important to put something tangible in your backseat that you need to get out when you leave the car – your pocketbook, your cell phone, a briefcase, your lunch bag – just to remind you to always check the backseat.”
Walston said that while many parents think this could never happen to them, it can be as easy as breaking your routine to make a parent forget a child is still in the car. More than 50 percent of child deaths from hot cars are from children that have been forgotten in vehicles, and only 17 percent have been intentionally left.
Walston earns North Carolina Coordinator of the Year
Allan Buchanan, Safe Kids North Carolina director, was on hand during the event to recognize Walston as Safe Kids North Carolina Coordinator of the Year.
Buchanan said Walston is a great role model for other Safe Kids Coordinators and is a great leader for the program across the state.
“She does a wonderful job here in Pitt County, getting the message out on injury prevention,” Buchanan said. “In North Carolina, we actually have 46 coalitions across the state. Ellen does a fabulous job here in Pitt County for injury prevention program across a number of different risk areas. She’s just a vital access to the community and creating risk reduction in this area. We’re very fortunate to have Ellen as a coordinator.”
Last year, Safe Kids Pitt County was recognized as the North Carolina Coalition of the Year. Walston said she’s just happy to share the recognition with her many community partners across Pitt County and eastern North Carolina.

She said the nomination was anonymous but she believes the events her team hosts, the collaboration with community partners and the work that Safe Kids Pitt County does with other Safe Kids coalitions across the state helped earn the award.
“I do think when they see these type of events and the work that we do in Pitt County and beyond that, they pay attention and we really try to partner with other Safe Kids coalitions,” Walston said. “So I’m all about sharing resources and working together, that’s how you make it happen. We’re really fortunate to have such great partners.”
ECU Health nurses from every area of expertise across the health system gathered on June 20 at the East Carolina Heart Institute for the 10th annual ECU Health Nursing Summit where they shared best practices and innovations that will help chart the future of nursing in eastern North Carolina.
Titled “Connecting with: Minds, Hearts and Purpose,” nursing leaders at ECU Health designed the summit to acknowledge what nurses have experienced over the last three years, including what the COVID pandemic taught them as professional nurses, what they have lost and what it will take to move nursing forward together, according to Trish Baise, ECU Health chief nursing executive.
“With the ever-changing health care environment, it is important for ECU Health nurses to hear from state and national colleagues,” said Baise. “We are proud to welcome experts who are making a positive difference in the field by advocating and influencing policy, as well as nurturing innovations that address the workforce, the nurse practice environment and the health and wellness of nurses.”

In total, more than 178 nurses attended the summit, which was held face-to-face for the first time since 2019. Topics included policy advocacy, building positive environments, communicating across generations, self-care and wellness. The summit featured presenters from both ECU Health team members and experts from other areas, including North Carolina State Senator Gale Adcock and keynote speaker Katie Boston-Leary, director of nursing programs for the American Nurses Association.
“The Nursing Summit gave me ideas, things to research and refreshed my mind to help navigate this different health care world that we live in,” said Paula Bush, MIU manager at ECU Health Edgecombe Hospital.
The summit also served as an opportunity for ECU Health nurses across various levels of expertise and experience to connect directly with health system leadership, fostering a sense of community among health system nurses.
“Sharing best practices from both within and outside the health system helps spark a culture of innovation within nursing,” said Daphne Brewington, ECU Health system vice president of nursing excellence. “When we harness the expertise of our nurses, we can lead improvements and create environments where nurses thrive here at ECU Health.”
Greenville, N.C. – The 2023 ECU Health Board Quality Leadership Award winners were recognized by the ECU Health Board of Directors June 27. These winning teams are a representation of excellent work across the system that drives the quality goal of zero harm, creates exceptional experiences and improves patient outcomes. Numerous nominations were reviewed by the committee, and the winning team are as follows:

ECU Health Medical Center – Navigating Insurance Authorizations: Increasing Internal Authorization Requests to Decrease Turn-Around Times to Facilitate Skilled Nursing Home Placement – Case Management. The project leader was Nancy Keith, MS, MSW, LCSW, ACM-SW – Care Management.
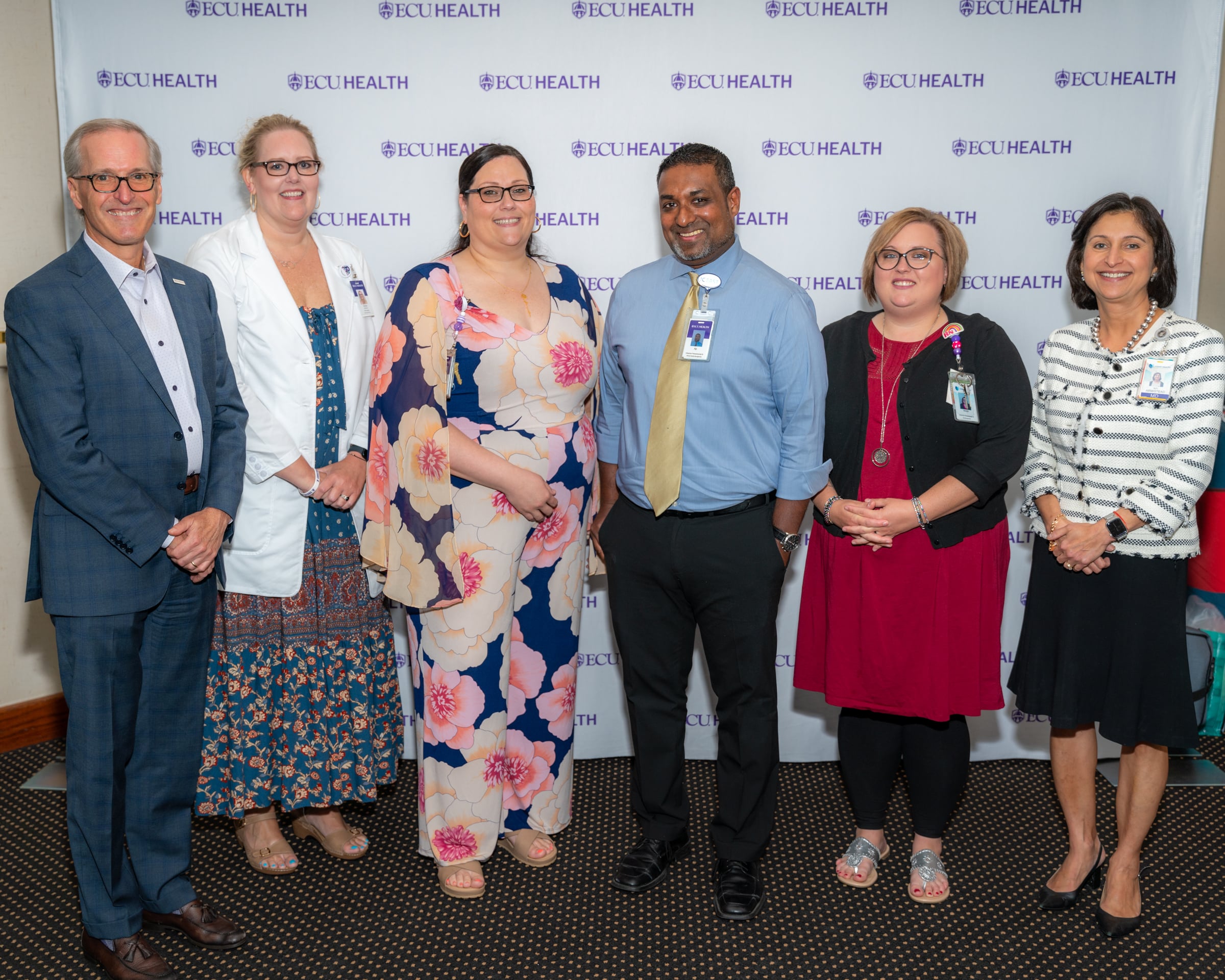
ECU Health North Hospital – Impact of Hospital-Wide Prevention and Reduction of Clostridium difficile (Cdiff), an ECU Health North’s Multidisciplinary Collaborative: An Evaluation on Reduction in Hospital Acquired Infection (HAI). The project leaders were Krista Turner, MSN, RN – Infection Preventionist III and Aparesh Balla, MPH – Infection Preventionist II.
To receive this honor, team members submitted projects that demonstrated at least two of the following requirements:
- Quantifiable improvement in an organizational quality priority with sustained excellence over time
- Demonstration of empathy and compassion in patient care
- Implementation of innovative solution to patient care problem
- Community outreach that addresses the social determinants of health in a meaningful way
“We are proud to recognize the winning teams for their hard work and dedication to caring for patients and families,” said Robert Greczyn, chair, ECU Health Board of Directors. “The Board Quality Leadership Awards represent the great consideration our team members take to make safety a top priority for our patients. These honorees have continued to innovate and improve the health and well-being of eastern North Carolina, and we are grateful for all that our team members do to deliver high-quality care.”
The Maynard Children’s Hospital at ECU Health Medical Center is celebrating its 10th year of offering high-quality, compassionate care in a soothing environment for patients and families in eastern North Carolina.
Dr. Matthew Ledoux, pediatrician in chief at Maynard Children’s Hospital, said the children’s hospital has immensely benefited the youngest patients in the East and made for more seamless care.
“The children’s hospital itself has given us the opportunity to grow services – we started an ECMO program, we’ve started and developed a dedicated Children’s Transport Team that flies all over the region and picks up kids and brings them back here,” Dr. Ledoux said. “The fact that we have all the subspecialty care, we have all the surgical care and generalized pediatric care here makes all the difference. It’s really a shining light in the East.”

Over the past 10 years, countless improvements have been made that have positively impacted the lives of many children and their families in eastern North Carolina. Other key expansions included the Pediatric Day Medical Unit, Pediatric Radiology Unit, and Pediatric Pharmacy among several other additions.
 Kim Crickmore, PhD, RN, senior vice president for Women’s and Children’s Hospital and Community Health Programs, said the Maynard Children’s Hospital is an integral part of health care in eastern North Carolina today. Over the last 10 years, the children’s hospital has delivered more than 37,000 babies, with more 61,000 inpatient admissions, 216,000 emergency cases, 223,000 outpatient cases and an additional 700,000 pediatric outpatient visits through the ECU pediatric outpatient center.
Kim Crickmore, PhD, RN, senior vice president for Women’s and Children’s Hospital and Community Health Programs, said the Maynard Children’s Hospital is an integral part of health care in eastern North Carolina today. Over the last 10 years, the children’s hospital has delivered more than 37,000 babies, with more 61,000 inpatient admissions, 216,000 emergency cases, 223,000 outpatient cases and an additional 700,000 pediatric outpatient visits through the ECU pediatric outpatient center.
“When we consider the impact to the region over the last 10 years, it’s really unbelievable,” Crickmore said. “It means so much to us here at the hospital that we’ve been able to provide care, primarily under one roof and unite all the services and to be the destination in eastern North Carolina for children who are sick or injured and need the specialty care we provide.”
Crickmore and Dr. Ledoux both said one of the services they are most proud of is the Children’s Transport team. The team consists of intensive-care trained nurses and respiratory therapists skilled in providing the specialty care many children need from the onset of transport to arrival at Maynard Children’s Hospital. Crickmore said it has been an intentional focus to build the program over the last five years and the program has seen many successes.
The Space
The amenities offered in the under-the-sea-themed Maynard Children’s Hospital are designed with patients and families in mind. Soothing young patients in a health care setting is no small task, but the children’s hospital is uniquely equipped to handle the challenge.
Dr. Ledoux said the community has stepped up time and again to provide resources and make donations that make a real difference for patients and families.
When thinking about his favorite area of the Maynard Children’s Hospital, Dr. Ledoux came back to the light tower, which can be seen when driving past the hospital. He said it’s a reminder of why he, and every children’s hospital team member, shows up to work every morning – to take care of the youngest patients in eastern North Carolina. He said he’s often asked what the colors on the light tower mean when people drive by at night.
“The reason is, we’re generally celebrating a child, we’re celebrating the end of a treatment, they’ve finished chemotherapy, or maybe they’ve been in the NICU for two or three months and they’re getting to go home,” Dr. Ledoux said. “We really try to make sure that the families and children get to pick the color and the time, but any time you see the color change anything different from our usual light blue, we’re celebrating a child and a family so it’s pretty exciting.”

Into the Future
Crickmore and Dr. Ledoux both said the next 10 years are something they’re looking forward to with the Maynard Children’s Hospital. They hope to continue expanding services and looking more to the region to bring specialty care closer to home for patients and families.
Dr. Ledoux said he and other physicians in the system have enjoyed their time spent in the region and the ability to help patients and bring key services closer to home for patients makes it special.
“I think the biggest thing is the distance that people have to travel,” Dr. Ledoux said. “We know that it’s a very underserved population and there’s a lot of poverty. People have challenges paying for gas or even having a car. The closer we can be to them to provide those services, the better.”
Another upcoming project that will impact pediatric patients in the East is the behavioral health hospital, slated to open in Greenville in 2025. ECU Health is partnering with Acadia Healthcare to build the state-of-the-art facility that will feature 24 inpatient beds specifically for children and adolescents with mental health needs. These beds will be the first of their kind in ECU Health’s 29-county service area and the only child and adolescent beds within 75 miles of Greenville, North Carolina.
Join us in celebrating the Maynard Children’s Hospital and all of its team members for the last 10 years of service to eastern North Carolina.
Four students in the Brody School of Medicine at East Carolina University have been named to the 2023-24 class of the North Carolina Albert Schweitzer Fellowship (NCASF) program and will spend the next year working on projects that address social factors that impact health and health care. Their projects will be completed in part at ECU Health facilities.
They are part of a class of 29 North Carolina graduate students — including two other Brody students and two students in the ECU School of Dental Medicine — representing medicine, dentistry, physical therapy, occupational therapy, public health and law.
“Schweitzer Fellows are not given a project or told to address a specific health need,” said Barbara Heffner, executive director of the N.C. Albert Schweitzer Fellowship. “They follow their passion and the needs of the community to develop innovative approaches which fill gaps in our health care system.”
Schweitzer Fellows develop and implement service projects that address the root causes of health disparities in under-resourced communities, while also fulfilling their academic responsibilities. Each project is implemented in collaboration with a community-based organization. Schweitzer Fellowships include an intensive leadership component, with fellows working closely with community and academic mentors during their fellowship year.
The ECU Schweitzer Fellows working on projects through ECU Health sites are:
Miranda Freeman and Michael Burt, Brody School of Medicine

Miranda Freeman

Michael Burt
A.C. Reid Schweitzer Fellows
Academic Mentor: Dr. Rima Panchal
Site Mentor: Dr. Margaret Clifton
Site: Palliative care unit at ECU Health Medical Center and Service League of Greenville Inpatient Hospice
Freeman and Burt are developing an end-of-life companions volunteer program to provide compassionate end-of-life companionship to palliative care patients who do not have anyone able to visit them. Volunteers will receive basic inpatient and outpatient hospice training, participate in narrative medicine workshops and will become knowledgeable advocates for the role of palliative services in modern patient care.
Freeman, a fourth-year medical student and native of Eagle Springs, said her passion for the project comes from her father’s recent cancer diagnosis.
“I saw how incredibly important it is to have support and care during scary difficult moments in life,” she said. “End of life should not have to be something individuals go through on their own. This program aims at providing more support to those at the final stages of their lives.”
Burt, a fourth-year medical student from Williamston, said the project aims to bridge a gap for a vulnerable population that deserves support.
“One group of individuals who are often not appreciated in conversations about loneliness is those who are in hospice care,” he said. “There are unfortunately many people who find themselves alone as they approach the end of their lives, and we believe they deserve the option of compassionate companionship, outside of their health care team, during this time.”
Vaishnavi Siripurapu and Elisabeth “Ella” Whitfield, Brody School of Medicine

Vaishnavi Siripurapu

Elisabeth “Ella” Whitfield
Academic Mentor: Dr. Lisa Moreno
Site Mentors: Dr. Hannah Florida, Dr. Lauren Sastre
Site: ECU Physical Medicine and Rehabilitation Inpatient Unit
Siripurapu and Whitfield are launching a cardiovascular health intervention for patients at the ECU Physical Medicine and Rehabilitation Unit focused on individualized goal setting, nutrition education, behavioral health and community support.
Siripurapu, a second-year medical student from Mooresville, said her passion for the project comes from watching her father’s diabetes journey.
“After following his journey and realizing the impact that chronic cardiovascular disease has on many people in my rural community,” she said, “I decided to pursue a project in order to address this unmet need that has manifested in my own life.”
Whitfield, a second-year medical student from Durham, said the project will address continuity in support from the hospital to home.
“During their hospital stay, patients are provided with structure, nutritional counseling and convenient healthy meals, therapy such as physical and occupational therapy, and support from hospital staff. However, upon discharge, this support structure is removed, leaving patients feeling isolated and powerless in their circumstances,” Whitfield said. “With the status quo, patients have a difficult time creating lasting change. We hope to ease this transition for CVD patients, and prevent future re-hospitalizations, by providing an abundance of supportive measures during this gap in care. We want to support individuals in a holistic way and help to empower them to feel confident in their ability to take charge of their own health journey.”
The NCASF is funded through the Blue Cross and Blue Shield of North Carolina Foundation, Delta Dental of North Carolina, Duke University School of Medicine, ECU Brody School of Medicine, North Carolina Area Health Education Centers, North Carolina Central University School of Graduate Studies, University of North Carolina School of Medicine, North Carolina Oral Health Collaborative, UNC Office of Interprofessional Education and Practice, ECU Health, Wake Forest University Health Sciences and individual donors.
NCASF began in 1994 as a local chapter of the national nonprofit, the Albert Schweitzer Fellowship, and has trained more than 600 leaders in health care. Nationally, more than 4,000 U.S Schweitzer Fellows have served individuals and communities in need and are continuing to shape health care policy and provide direct service.
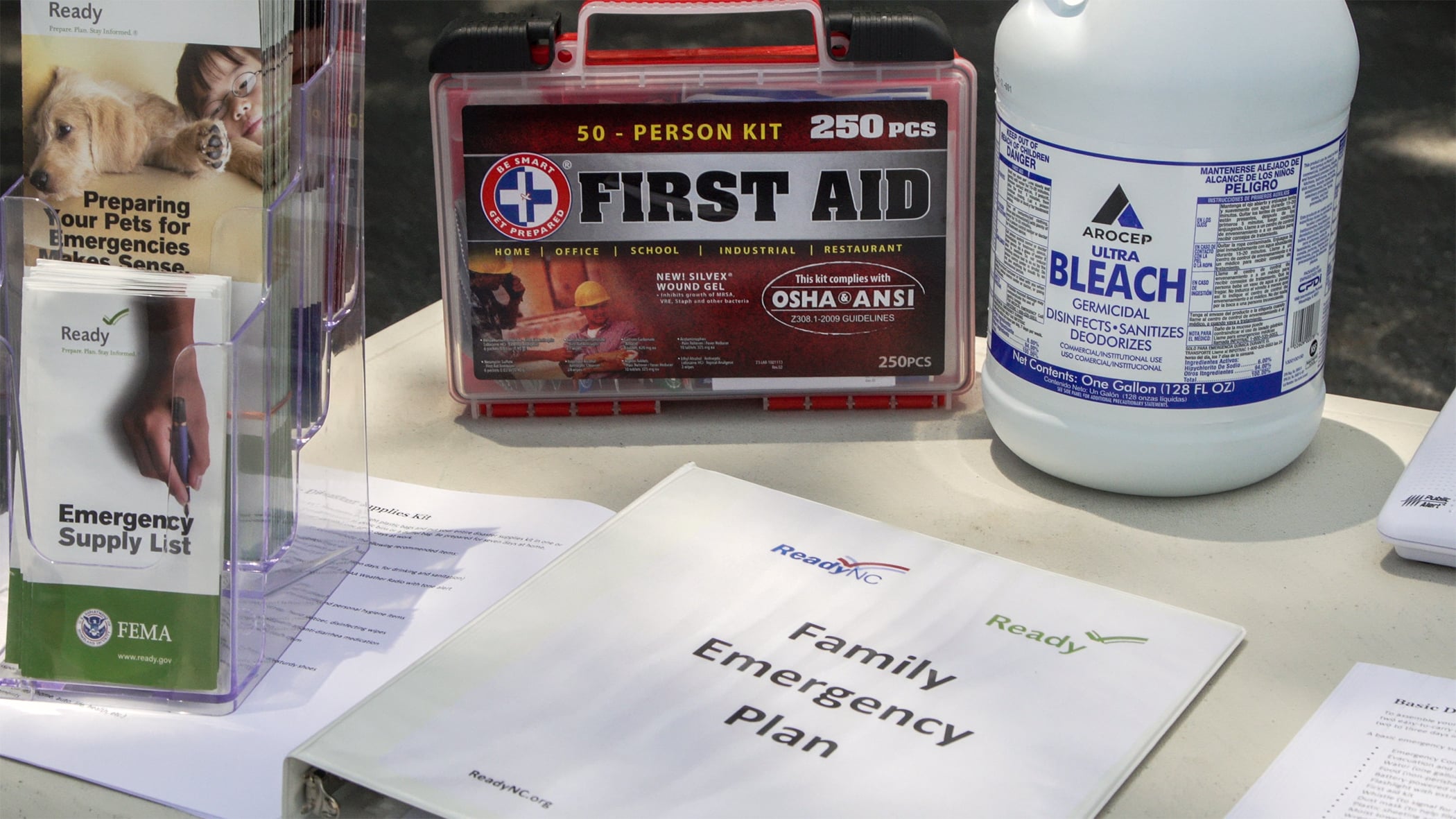
Hurricane season is underway in the Atlantic and according to the Eastern Healthcare Preparedness Coalition (EHPC), it’s expected to be an active season.
The EHPC team said that while hurricanes are difficult to predict, we can all do our part to prepare for the best possible outcomes. That includes preparing yourself, your family and your home for potential storms.
“If something goes off unexpectedly and you’re unable to leave your house potentially due to flooding, do you feel like you could provide for yourself and your family, including your pets, for about 72 hours?” Stephanie Seals, disaster services specialist with EHPC, asked. “Historically, we know the rescue services aren’t able to help for about the first 72 hours, so we always recommend having enough food, water and medications at your home to take care of yourself, your family and your pets for that time.”
Other key items to keep in mind for your preparedness kits include important phone numbers, documents like birth certificates, marriage certificates and wills, and a first aid kit.
“You don’t necessarily have to go out and buy a brand new first aid kit, you can kind of buy your equipment and piecemeal it together yourself, but it’s important to make sure it’s stocked,” Seals said. “The big things that we see needed after these storms are things such as band aids, ace bandages and gauze to wrap up injuries and your basic antiseptic ointment to clean off those wounds.”
Ready.gov is a federal government website with helpful information about how to properly prepare for a hurricane. This includes guidance on Creating a plan that meets the specific needs of your household and building an emergency kit that contains supplies to help you stay adequately prepared for a natural disaster like a hurricane.
The EHPC team is ECU Health-based while proudly serving all of eastern North Carolina, which enables Seals to pursue her passions on both the personal and professional fronts.
“Getting to help people when they need it the most is incredibly important to me. I think helping people help themselves is one of the coolest things we get to do, too,” Seals said. “We have heard back from people that we get to train and educate and they’ll say, ‘When this happened unexpectedly, we had a house fire or another situation, I was ready because of the things that we put together.’ That just means the world to me.”
Resources
Hurricanes can form quickly. Take the time now, before a hurricane impacts our region, to educate yourself on how to prepare and respond. Below are helpful links for federal and state websites: