Washington, N.C. – ECU Health Beaufort Hospital – a campus of ECU Health Medical Center has been designated as a primary stroke center by The Joint Commission and the American Heart/Stroke Association, recognizing the hospital’s preparedness and expertise to care for stroke patients. Stroke is one of the leading causes of death in the state, resulting in more serious long-term disabilities than any other disease. With this designation, all ECU Health hospitals are equipped to provide advanced stroke care in communities across eastern North Carolina.
“Stroke certification from The Joint Commission represents ECU Health Beaufort’s commitment to provide high-quality stroke care to not only patients experiencing stroke symptoms, but to all of our patients,” said Debra Hernandez, president of ECU Health Beaufort. “We are proud of being designated a primary stroke center. The commitment and diligent work of team members across all levels and services made this a reality.”

As a primary stroke center, ECU Health Beaufort can treat and stabilize patients experiencing an acute stroke and care for more complex patients. As part of stroke readiness by all hospitals in the ECU health system, this certification is symbolic of a comprehensive stroke network capable of meeting the needs of all patients across eastern North Carolina.
“Achieving stroke certification for all nine hospitals has been our goal since launching an intentional focus on improving stroke care in eastern North Carolina seven years ago,” said Barry Bunn, chief of medical staff and regional medical director of emergency services, ECU Health. “At the start of this process, ECU Health began a pathway of certifying all of the ECU Health hospitals with some level of stroke certification by the Joint Commission. Stroke certified hospitals were prevalent west of I-95, but there were few certified hospitals in the eastern part of the state. Now, we can proudly say that patients across the region will have access to high-quality stroke care, regardless of where they live.”
Because time is one of the most important factors in treating stroke, it is vitally important to provide stroke care close to home. ECU Health Beaufort’s stroke certification increases proximity to quality care in the Washington area, which reduces the risk of mortality, permanent brain damage and other side effects including memory loss, difficulty speaking and potential paralysis.
During the certification process, ECU Health Beaufort was evaluated on performance measures in stroke care, including education for patients and families on stroke risk factors and recognizing symptoms of stroke. Other performance measures included staff education on stroke protocols and the appropriate prescription of medications to address stroke risk factors such as elevated cholesterol and blood pressure.
The severity and likelihood of having a stroke in North Carolina is significantly higher than the rest of the country as a whole. Eastern North Carolina is at the center of many strokes, often called the buckle of the stroke belt. North Carolina is about 8 percent worse for stroke mortality than the national average, and in eastern North Carolina, that risk is even greater.
“With all hospitals in the ECU Health system now stroke certified, a patient will be offered life-saving care regardless of the patient’s proximity to any of ECU Health’s hospitals and depending upon what additional treatments are needed, can be transported to a location with more extensive services when the patient is stabilized,” said Jay Briley, president of ECU Health Community Hospitals. “This system-wide stroke certification helps fulfill ECU Health’s mission of improving the health and well-being of eastern North Carolina.”
With Fourth of July weekend upon us, summer fun is in full swing. While this weekend brings families together for cookouts and celebrations, we know there are also risks to look out for.
Home firework shows can quickly turn a weekend of fun into a trip to the emergency department.
Ellen Walston, Injury Prevention Program coordinator at ECU Health Medical Center, said that in North Carolina last year, 11,500 people visited an emergency department for a firework-related injury. Of those visits, 70 percent came in July.
“July is the most dangerous month for firework injuries and actually many injuries occur in the summer months,” Walston said. “It’s a very fun time of the year with lots of vacationing, traveling, it’s time to spend with family, but you need to keep safety in the forefront.”

She said the key to safety this time of year is supervision, whether it is around water, fireworks or any other activity with increased risks. Keeping a close eye on children can help limit injury risk.
Walston also noted that many would be surprised to learn that sparklers burn at 2,000 degrees and can easily cause severe burns. Even after sparklers are done burning, they can still be up 450 degrees for minutes after they are extinguished.
“Many times parents don’t realize how dangerous sparklers are because they’re fun,” Walston said. “Children will often run around with the sparklers and may accidentally touch another child with a hot tip. That can be very dangerous.”
This year, there are a couple of particular risk factors that make this season a bit more dangerous. Fire hazards are higher than usual with the recent drought we have faced in eastern North Carolina and with Fourth of July falling on a Monday, many families will take advantage of the long weekend to have a longer celebration.
“We want you to have fun, this is a fun time of year. But we are at a greater risk for increased injuries. We just ask for families to be as careful as possible,” Walston said. “With COVID, we are excited to be able to get out, vacation, spend time with family, but we really need supervision to be at the forefront.”
Walston said letting professionals handle the fireworks is the best and safest way to enjoy the sights while celebrating the holiday. Visit your local municipal website to find firework shows in your area.
With our continued focus on the imperatives of quality, experience and finance, ECU Health’s transplant program at ECU Health Medical Center has consolidated their treatment and office spaces into the newly renovated 3 South. The area is now known as the 3 South Transplant Clinic.
The transplant program performs an average of 80 to 100 living and deceased donor kidney and pancreas transplants per year. Patients that are seen in the clinic include pre-transplant (patients being evaluated for transplant), living donors and post-transplant. This program and the services offered have continued to grow over time, but have been limited by clinic space. To enhance patient and team member experience, the pre- and post-transplant clinics have now consolidated into one, centrally-designed space on 3 South, as they have been operating in separate clinics at the Cancer Center and ECU Physicians.
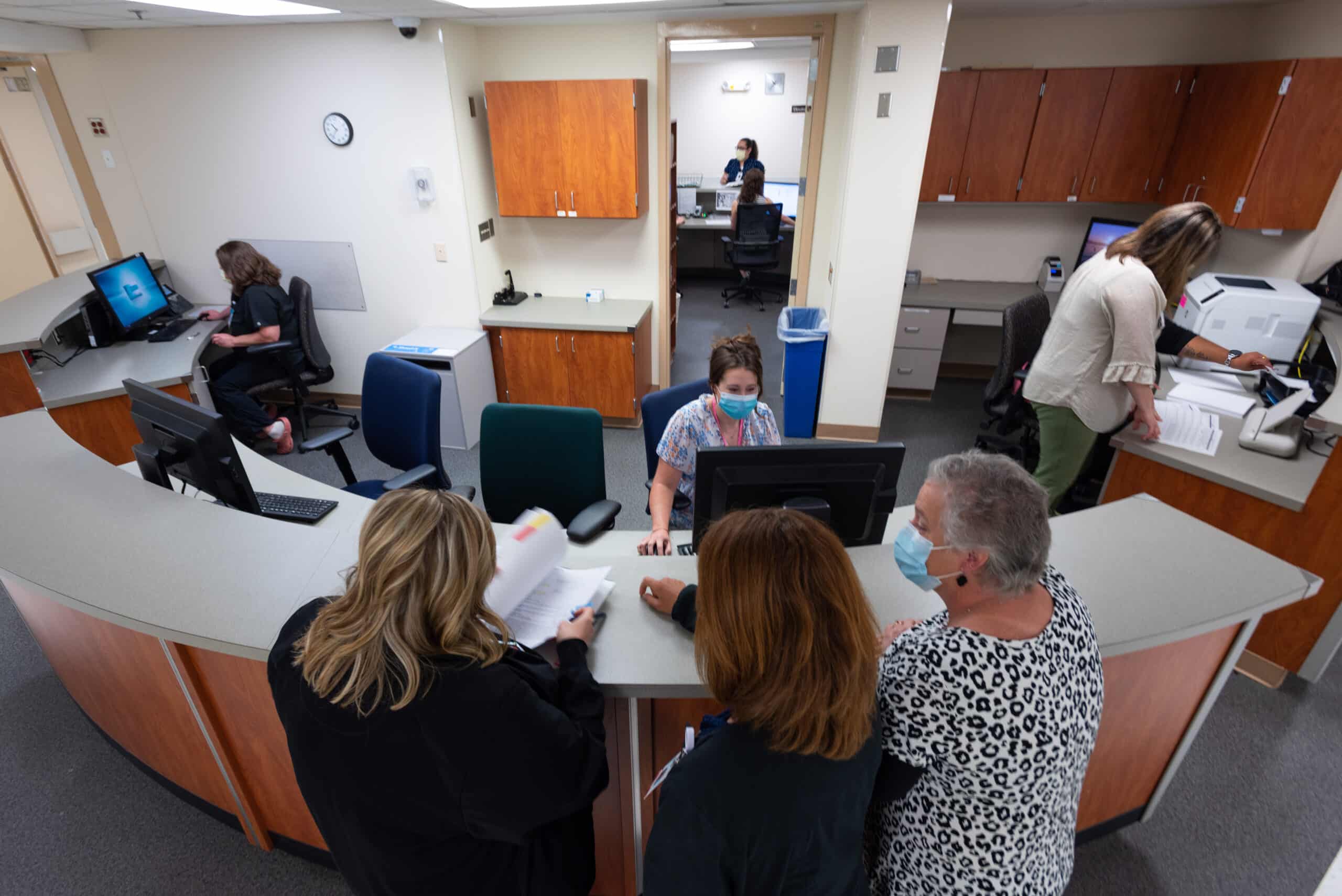
Previously, the transplant team worked in separate clinics, sometimes limited to three rooms. 3 South Transplant offers 18 patient exam rooms, which in addition to consolidating space for patients, will also help to shorten wait times for new referrals and follow up appointments.
Another benefit of 3 South is the accessibility of team members such as dieticians, social workers, pharmacists, nurses and physicians, which provides patients the accessible support of various teams of health care workers critical to patients’ transplant journeys.
Lastly, this consolidation allows for expansion of potential future services such as phlebotomy, expanded pharmacy services, infusion services and vascular access.
In 2022, as we build the future of ECU Health, the exceptional care and services we provide have a positive impact on the communities of eastern North Carolina that we serve through our considerations of patient quality and experience.
For more information on transplant services at ECU Health, visit the transplant section of our website.
The Brody School of Medicine at East Carolina University has experienced recent success in recruiting a diverse group of patients to participate in clinical trials for new medications and treatments.
Data shows that from March 2019 to March 2020, 202 patients participated in oncology clinical trials in ECU’s Division of Hematology and Oncology; 50 percent of them represented races other than white. The following year, 419 participants were accrued, and 56 percent represented races other than white. That year, 50 percent of clinical trials participants were Black or African American.
“Our patient population, as well as Brody’s mission, has led to our success,” said Susan Eubanks, clinical trials nurse specialist in Brody’s Division of Hematology and Oncology. “Part of our core values is to cultivate a clinical environment of robust learning, innovation and discovery. There have been trials with participants here in eastern North Carolina that have led to new treatments in diseases and in some cases where there were few options.”

Now, researchers and providers hope to build on that momentum for future clinical trials studies.
Providers and researchers in the school continue to seek minority participants in clinical trials for new and potential pharmaceuticals — and to collect invaluable information on how some treatments impact patients of various races.
Doctors want to ensure that the drugs they are studying match the demographics for all the patients who could rely on those medicines in the future — by including people from a wide variety of backgrounds and races in the studies.
“We all agree that as much as possible, the drugs we give should be approved through clinical trials that match the demographics they will be prescribed to,” Eubanks said. “There has been chemotherapy that has shown promising results in one country but doesn’t carry the day in another. So, overcoming this disparity — whatever the cause — is essential.”
One of the latest innovations in oncology is the use of immunotherapy, the treatment of disease by activating or suppressing the immune system. Data that reviewed participation in those trials showed that less than 4 percent of participants in key immune therapy trials were African American.
“This is a problem,” Eubanks said. “Given the low representation we can’t predict if there will be a differences in outcomes related to differences in response from tumor biology. It is not highly understood why we see differences in drug efficacy and toxicities among different ethnicities, but it drives the point home, we need to do all we can to include the best representation of our population when bring new therapies to market.”
Dr. Darla Liles, professor and division chief of ECU’s Division of Hematology and Oncology, said diseases like prostate cancer and colorectal carcinoma see more African Americans impacted than other races, and the diseases begin earlier in those patients as well.
“Also, the distribution of the DNA mutations are different across races,” she said. “We might have a drug that works wonderfully well in Caucasians but not so well in African Americans or Hispanic individuals because of these different DNA changes. But we only know that if enough minorities participate.”
Recruiting challenges
Even with the critical need for data that better illustrates potential patient outcomes, recruiting minority participants in clinical trials can be difficult.
“Accruing to clinical trials in general is difficult, but minorities are typically underrepresented in clinical trials,” Eubanks said. “This can be an access issue, a reluctance issue and, at times, both.”
There can be many reasons recruiting minority participants to clinical trials can be a challenge, Liles said, but keeping those reasons in mind and understanding that they vary from person to person help build trust.
Brody’s mission draws heavily on a theme of access for all: to a medical education, to health care, and to resources that can sustain health and wellness. That’s one reason access to clinical trials in the medical school is vital to the study and approval of novel treatments.
“Part of our commitment to the health care of all eastern North Carolinians is ensuring the pharmaceuticals and treatments that we study are safe and effective for every patient who may need them in the future,” said Dr. Michael Waldrum, Brody’s dean and CEO of ECU Health. “Our efforts to widen the participant base in our clinical trials programs reflects the importance of thorough and inclusive studies that yield results that we are confident meet our mission.”
Liles said that people are more likely to trust providers and those running clinical trials if they feel they share common bonds with them.
“Several times when I presented a trial to a patient, afterwards the CRA has told me that they went to high school with the patient or knew them from church,” she said. “Being able to relate to the people who are treating you is essential.”
Education is key as well, Liles said.
“When I offer a trial to a patient, I often understand this is starting a conversation over several visits to ensure patients know about and understand what they are signing up for,” she said. “The consent forms for clinical trials are jam-packed with important information about the treatments, and sometimes people use that as a starting point for knowing what to ask about their treatment. I never regret giving a patient a consent form and talking to them about a trial. Even if they eventually decide not to do it ,they are better informed by participating in the process.”
Eubanks said the COVID-19 pandemic and reluctance by some to take the vaccine are a reminder of how to approach building trust in clinical trials.
“We must think beyond just education in the office,” she said. “We must reach people where they are.”
One way Brody is working to reach many different patients is having trials open for a variety of specialty care areas.
“The biggest step is understanding your population and having trials open for the specialty areas you see,” Eubanks said. “Brody has trials open with many specialties. In adult hematology/oncology we use databases and the tumor registry when approached about upcoming trials to help us determine if a trial is potentially feasible in our area. We also have the benefit of having local resources such are the University and Medical Center Institutional Review Board (UMCIRB) and leaders such as our associate dean for research and graduate studies, Dr. Russ Price, that provide expertise and infrastructure needed to offer clinical trials.”
Liles uses word of mouth to share clinical trial opportunities to patients.
“I often tell my patients about new and innovative trials that are on the horizon, even if they do not fit the criteria for the trial,” she said. “I think it is important for patients to understand that there are new things being developed all the time. Education is our best way to ensure patients know about and participate in trials.”
Liles also believes the combination of specialties and resources in the creation of the ECU Health brand will have a positive impact on the clinical trials program. With close to 1.4 million people in the system’s service area, there is promising potential to reach people through improved infrastructure for research opportunities.
Read more from ECU News Services.
A team from the Brody School of Medicine’s Internal Medicine Residency Program won first place and the Osler Cup in the American College of Physicians Doctor’s Dilemma competition.
Coached by Dr. Lacy Hobgood, clinical associate professor in East Carolina University’s Department of Pediatrics, the team competed for three days against some of the world’s brightest medical residents, including teams from the United States, Canada, Central America and the Caribbean. Drs. Alex Bradu, Omar Khdeir and Swethaa Manickam earned the right to compete at the national level by first winning the North Carolina chapter’s competition.
Past winners of the ACP Doctor’s Dilemma competition include the India chapter, Albert Einstein Medical Center, Indiana University School of Medicine, Northwestern University and the Mayo Clinic.

Khdeir said Doctor’s Dilemma is the biggest competition based on knowledge of internal medicine, featuring as many as 60 teams each year in a friendly but highly competitive environment. The format is similar to the television show “Jeopardy,” with each game consisting of a set of questions teams must buzz in to answer, and a final round in which they must wager their points before seeing the question.
“We wagered all of our collected points in the final dilemma and got the question right,” Khdeir said. “After we won, we took turns calling our parents on speakerphone. Seeing our parents and siblings proud and happy was the biggest award.”
Dr. Herb Garrison, associate dean for graduate medical education, said the team’s performance on the national stage reflects the quality of medical education at Brody and also helps enhance its reputation.
“They competed against the best residents from around the world in a test of medical knowledge and speed and emerged as the winning team,” Garrison said. “In addition to demonstrating the type of great physician trainees we have at the Brody School of Medicine and ECU Health, this win provides us a huge recruiting advantage as other schools will take notice and want to send their best medical students our way. … I couldn’t be more proud.”
The Internal Medicine Residency Program is an integral part of the Brody School of Medicine and the ECU Health Medical Center. The Department of Internal Medicine includes nine subspecialty divisions and serves the Greenville and Pitt County area as well as 29 surrounding counties.
Read more from ECU News Services.
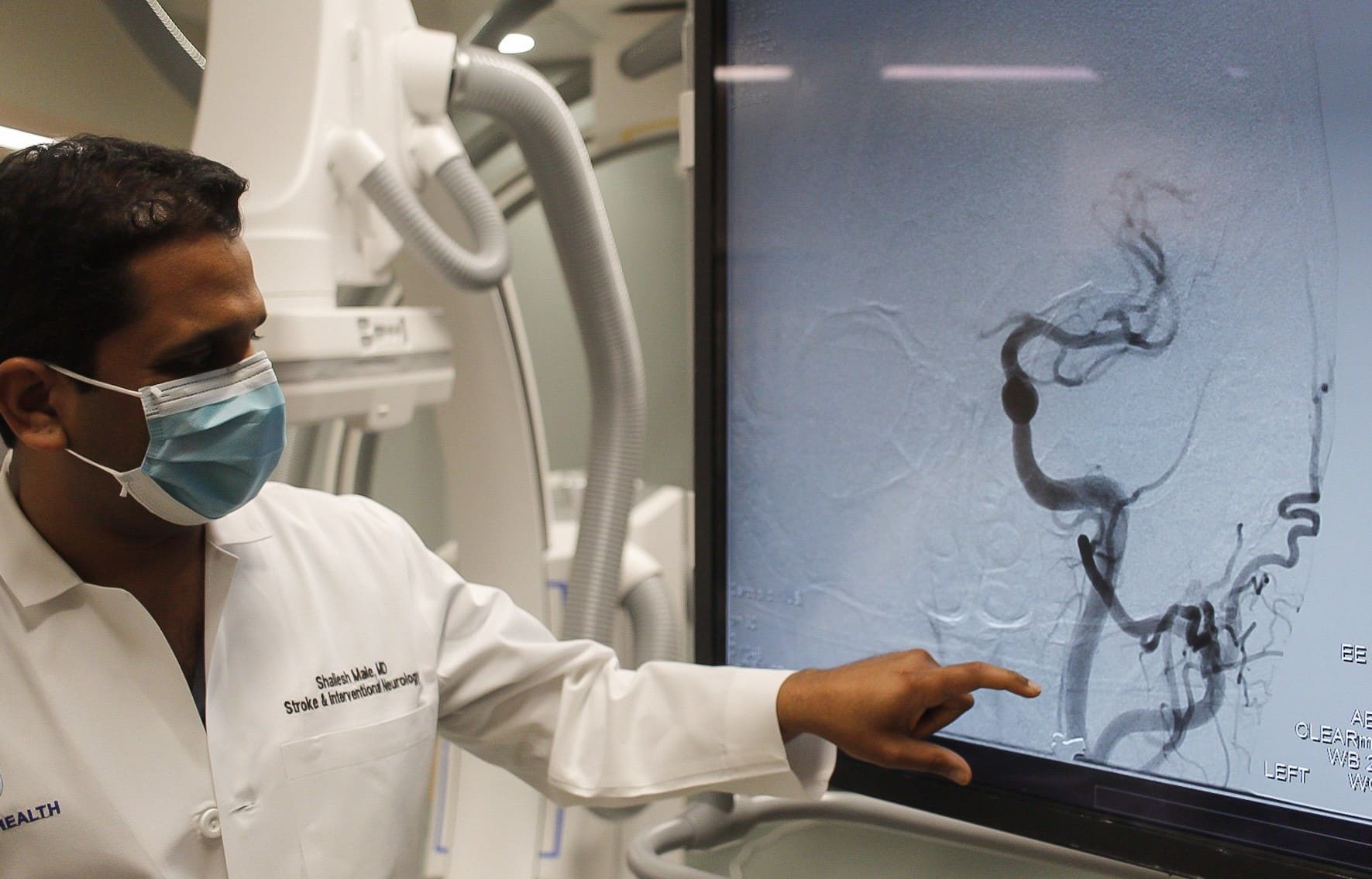
Younger people are increasingly suffering from strokes according to medical experts at ECU Heath. While risk of stroke increases with age, health care teams have seen an increase in strokes in young people, partly due to a combination of COVID-19, an increase in consuming processed, sugary and fatty foods as well as smoking and vaping.
“With COVID-19, we have noticed an increase in strokes, especially in younger populations,” said Dr. Shailesh Male, stroke medical director, ECU Health Medical Center. “During the peak of the pandemic, my colleagues and I noticed that young patients who do not have vascular risk factors were having strokes. COVID-19, like other infections, increases the risk of forming blood clots and, in turn, can lead to higher risk of strokes.”
Strokes are considered the heart attack of the brain. A stroke occurs when a blood clot compromises blood flow to the brain. This leads to loss of brain function, manifesting in symptoms including: weakness or numbness on one side of your body, slurred speech or difficulty understanding others, blindness in one or both eyes, dizziness and/or a severe headache.
Risk factors for stroke can be broken down into two categories: modifiable and non-modifiable.
“We like to focus on the modifiable risk factors, the ones that you can change,” said Dr. Male. “These include hypertension, cholesterol, diabetes, smoking, physical inactivity and obesity.”
The increase in younger people having strokes are mostly attributed to modifiable risk factors. The rise in popularity of e-cigarettes and vaping has largely been in younger populations. Smoking reduces the amount of oxygen in the blood, makes the heart beat faster and raises blood pressure. Additionally, younger people are generally less healthy than previous generations in terms of diet and exercise.
“Processed, fatty and sugary foods are increasingly becoming a regular part of our diets at a younger age,” said Dr. Male. “This combined with an inactive lifestyle increases almost all risk factors including obesity, diabetes, high blood sugar, hypertension and high cholesterol.”
Non-modifiable risk factors include older age, gender (men face higher risk of stroke), family history, genetics and even race. According to The Office of Minority Health, African Americans are 50 percent more likely to have a stroke than non-Hispanic whites adult counterparts and 70 percent more likely to die from a stroke.
“African Americans have higher incidences of hypertension, diabetes and high cholesterol, which in combination, increases the risk of strokes,” said Dr. Male.
It is important to discuss risk factors with your primary care provider. If you have had a stroke, your doctor may prescribe preventative medications to address risk factors like blood thinners, cholesterol medication or blood pressure medication. Additionally, lifestyle changes such as exercising more and eating healthier foods are proven to lower your risk of stroke.
“With great treatment options now widely available, it is important to remember, time is of the essence,” said Dr. Male. “The sooner we implement treatment, the better the odds that the patient will recover to their baseline. The benefit of early treatment is preventing long-term disability.”
If a stroke is not caught quick enough, long-term disability and health issues are possible. Most commonly, patients may lose strength on one side of their body or have problems speaking.
The acronym B.E. F.A.S.T. can help quickly identify the signs and symptoms that you or a loved one may be experiencing a stroke:
- B – Balance problems
- E – Eye issues like blindness or seeing doubles
- F – Face drooping
- A – Arm weakness
- S – Speech slurring
- T – Time to call 911
Dr. Mike Waldrum, ECU Health CEO and dean of the Brody School of Medicine at East Carolina University was recently named to Business North Carolina’s 2022 Power List. ECU Chancellor Dr. Philip Rogers was also named to Business North Carolina’s 2022 Power List in the Education section.
This yearly list names the most influential leaders in the state of North Carolina across various industries. The awarded leaders are nominated for this list based on their influence as strong leaders.
“This recognition represents the tireless work ECU Health team members do every day to serve the region and educate the future physicians for North Carolina,” said Dr. Waldrum. “At ECU Health, we strive to become a national model for rural health delivery by providing high-quality care to the region we proudly call home. Our regional health care organization, combined with the Brody School of Medicine, strengthens our shared mission to improve the health and well-being of eastern North Carolina. ECU Health will continue to innovate and provide high-quality care to those we serve.”

We are proud to have strong leadership moving ECU Health forward to meet the joint mission of improving the health and well-being of eastern North Carolina by training the providers of tomorrow, collaborating with community partners to solve complex issues and bringing clinical innovations that improve the lives of those who proudly call this region home.
To read the Business NC Power 100 List article, please visit https://businessnc.com/2022-power-list/.
Two Vidant leaders were recognized on Friday, March 18 and inducted into the East Carolina University (ECU) College of Nursing Hall of Fame along with seven other recipients.
Dr. Julie Kennedy Oehlert, chief experience officer at Vidant Health, and Dr. Kamilah Williams, administrator for nursing professional practice, development and clinical education at ECU Health Medical Center (VMC), were each honored last week after being nominated by colleagues and accepted into the ECU College of Nursing Hall of Fame.
Dr. Williams is a 2005 graduate of the ECU College of Nursing and an eastern North Carolina native. She said she is proud to serve the community she calls home and the induction was a great honor.

“I’m so humbled and proud to be a Pirate nurse,” Dr. Williams said. “I’m proud to give back to my community here in eastern North Carolina, where I grew up as a young child. It’s an honor to serve and care for the population that I grew up with. I’m just grateful.”
Dr. Williams is tasked with developing nurses in her role at Vidant. Under her leadership, VMC achieved accreditation for the Nurse Residency Program and has developed an International Nurse Fellowship Program.
She said she loves what she does and is happy to give back to her profession and region through her role.
“When I think about the mission of our organization and being able to improve the health of the people here in eastern North Carolina, it’s exactly why I do what I do,” Dr. Williams said. “As a young child, I always knew I wanted to be a nurse and be able to give back to my community. Now in my role, to be able to help develop future nurses, it’s just a humbling experience.”
Dr. Julie Oehlert has used her experience as a nurse to improve the experience of patients, families and Vidant team members across eastern North Carolina. Dr. Oehlert came to Vidant and eastern North Carolina in 2016 and said the recognition made her feel at home.
“For me, I was so humbled and excited to be recognized with other Pirate Nurses,” Dr. Oehlert said. “I came from outside of Vidant but my heart is with Vidant and ECU. I feel welcomed into this community. I was so overwhelmed when I was nominated and accepted.”
Dr. Oehlert said she is proud to be part of a health system with so many Registered Nurses as leaders in different areas. With nurses in non-traditional roles lending their health care expertise and compassion for patients and families, the nursing heart can be seen in many facets of the health system.
“I don’t get to work directly with nursing but the nursing heart of all the leaders that have RNs behind their name, is pretty darn special at Vidant,” Dr. Oehlert said. “Many of our presidents and executives have that RN heart and that means we are always caring about our communities, we always have a holistic view on care and I love that.”
With the nine inductees for 2022, the ECU College of Nursing Hall of Fame that started in 2011 has grown to 150 members.
One of the past inductees on hand for the event was Dr. Daphne Brewington, senior vice president nurse executive at ECU Health Medical Center.
“It’s just been an amazing night and both Dr. Williams and Dr. Oehlert are so deserving of this award,” Dr. Brewington said. “I’m so proud that they have been inducted into the ECU College of Nursing Hall of Fame. I was inducted in 2018 so it’s just really special and surreal to be able to support colleagues that are on this journey as well.”
Inductees into the Hall of Fame also help fund a scholarship for ECU College of Nursing students, which has raised $170,000 throughout the years to support the next generation of nurses.
Learn more about the ECU College of Nursing Hall of Fame on ECU’s website.
For the first time since 2019, one of East Carolina University’s most exciting annual events returned to an in-person format Friday when 82 fourth-year medical students learned where they will be spending the next three to seven years completing residency training.
Surrounded by their family and friends during the Match Day event in ECU’s Health Sciences Student Center, the students simultaneously opened envelopes containing the location and medical specialty they will practice.
In staying true to the Brody School of Medicine’s mission to increase the number of primary care physicians who serve North Carolina, especially in rural and underserved areas, 61% of this year’s students matched into primary care residencies. And 35% of the class matched into residency programs in North Carolina.
“We continue to excel in our mission,” said Dr. Michael Waldrum, dean of the Brody School of Medicine and CEO of Vidant Health. “So this a special day filled with excitement, optimism and pride in what these students have accomplished and where they’re going. We trained them and now they’re ready to go.”

For Waldrum, the Match Day event was special on a personal level.
Not only was this his first Match Day as Brody’s dean, his college roommate’s son, Mark McAlister, was one of the Brody students who matched this week.
Before McAlister chose a medical school, his father reached out to Waldrum — who was still years away from becoming Brody’s dean — to ask his opinion on which medical school to choose.
Waldrum recommended Brody because he considered it the highest value medical school in the nation and would provide him with quality preparation for any career path he chose.
Four years later, McAlister said he was glad he followed that advice.
“As fourth-year students we started to learn what good work goes on here, in terms of patient care and learning. And it felt like this was a spot where we could continue to excel as professionals and develop our careers,” he said.
That advice also helped McAlister meet his soon-to-be wife, Jacqueline Poston, who was the first classmate he met at Brody.
On Friday, McAlister and Poston learned that they both matched at ECU Health Medical Center and ECU in Greenville.
“Our priority was staying together and being part of a good program, so we are lucky that we got both of those things,” said Poston, who will be training in internal medicine-pediatrics. “We’ve grown so much as medical students here and I can’t wait to see how much more we grow as residents. It’s an amazing place to be, so we’re really happy.”

Improving accessibility for all patients
K’Shylah Whitehurst knew that wherever she matched, home is right here waiting.
Whitehurst, a Greenville native and ECU chemistry graduate, wants to eventually practice in Pitt County with her family close by and the special patient base she spent years preparing to care for — children.
On Friday afternoon, she opened her envelope, read it and then flipped it over to show her family that she will complete a residency in pediatrics at University of North Carolina Hospitals in Chapel Hill. As she hugged one of her grandmothers, the tears began to flow and continued with each hug as she went down the row of her family members in attendance.
“I’m so excited. I’ll be close to home. My family will still be nearby. This is one of my top programs, so I’m really, really happy. I’m so excited to continue on this next chapter,” she said. “This will be my first time living outside of Greenville, but it’s not too far so that’s fine.”
Whitehurst said she looks forward to returning to eastern North Carolina after residency to care for children in this region.
“One of the main reasons I decided to go into pediatrics was how resilient children are. Most of the time the children that we’ve seen in the hospital here at Vidant are going through the scariest times of their lives,” she said. “Caring for children not only involves nurturing relationships with my patients, but also gaining the trust of parents to care for their little ones. I’m so excited to start my career as a pediatrician.”
Whitehurst, a first-generation college student who knew she wanted to be a doctor by the time she was 8 years old, said Brody’s focus on serving the underserved and ensuring a diverse student body made the difference for her.
“I love the fact that year after year, the school works to have the most diverse student body. Now that I’ve reached the end of my four years of medical school, I know that I 100% made the right decision to come to Brody,” she said. “The connections that I was able to form with the faculty here is something that I will forever be grateful for.”
During her Brody experience, Whitehurst was selected for the service-learning distinction track, a four-year program that encourages students to work extensively with medically underserved, marginalized and rural populations throughout medical school. She volunteered at the Lucille Gorham Intergenerational Community Center and worked with Brody’s Department of Pediatrics to improve resource accessibility to patients. She also earned an ethnic and rural health disparities graduate certificate through the track.
Whitehurst also had the opportunity to participate in a national research project, “WE CARE Project-Reducing Socioeconomic Disparities in Health at Pediatric Visits,” which studies social determinants of health and works to increase patient access to resources. Whitehurst used a special database to learn about resources in Pitt County.
“Through participating in the WE CARE Project, I was able to learn about what resources are available for patients here in Pitt County,” she said. “When treating a patient, it’s so important to remember that they are a human being first. Ensuring that their basic needs such as food security and electricity in their homes are met are so significant toward the patients being able to even consider making it to a yearly doctor’s appointment. I do feel better equipped to consider every aspect of a patient’s life to provide the best treatment for them.”
A calling answered
After graduating from the University of North Carolina at Chapel Hill with a degree in political science, Lumberton native Ross Masters worked in Washington, D.C., for a year in sales before realizing that career path was not the right fit for him.
He instead found his true calling in medicine after taking an EMT-Basic course back home in North Carolina. Shortly after completing the course, Masters witnessed a hit-and-run automobile crash and experienced the fulfillment of “knowing what to do and being useful” during a real-life emergency.
Masters went back to school to complete his medical school science prerequisites and earned a Brody Scholar award, which is ECU’s most prestigious scholarship.

On Friday, Masters and his fiancée, Camille Bauer, learned that they both matched to Vanderbilt University Medicine Center in Tennessee where Bauer will train in obstetrics-gynecology and Masters will train in psychiatry.
“It’s an indescribable feeling,” Masters said. “Brody has treated us fantastic. We have had access to awesome mentors. Everyone has been super supportive and prepared us well for residency. So we’re feeling great about what Brody has done for us and we’re feeling great about the future as well.”
When Masters arrived at Brody, he was drawn to family medicine because he wanted to help address some of the social determinants of health that he witnessed as an EMT. However, his focus changed after he took part in patient psychiatry education at Brody.
“We were sitting down with social workers, pharmacists and therapists and I felt I was able to provide that whole comprehensive treatment to patients through psychiatry,” he said.
For Masters and Bauer, Match Day represented a major life moment, but it will not be the only one before they start residency training.
“We got a successful couple’s match, which is what we really cared about today,” Bauer said. “We met our first year and started dating about six months later. And now we’re getting married next month.”
‘I want to walk alongside my patients’
Emmanuella Mensah’s journey from her hometown of Charlotte to the Brody School of Medicine has come full circle. After graduation, she will be returning to Charlotte for a family medicine residency with the Carolinas Medical Center Biddle Point Urban Track, where she will train to care for underserved populations.
Mensah’s parents, Ofori and Theresa Mensah, and siblings Gloria and Ofori Jr., all from Charlotte, along with friend and third-year medical student Merdi Lutete were with her on Friday. Her mom said she was so happy that her daughter would be returning home for residency.
“I feel blessed, and I feel good. Thank you Jesus,” Theresa said. “I can have my baby back.”
The residency location was Emmanuella’s top choice, and after reading the match letter, everything was still sinking in.
“I’m very excited and I’m very grateful to know that someone wanted to train me,” she said.
Mensah earned her undergraduate degree at UNC-Chapel Hill and completed Brody’s Summer Program for Future Doctors, which helped her decide that ECU would be a good fit for medical school.
“The magic of Brody is the medical students, and meeting students during that summer, I really felt at home, and I really wanted to be a part of that legacy,” Mensah said. “Brody has meant everything to me. Brody took a chance on me when no one else would take a chance on me, and they’ve been instrumental in my growth as a student.”
Born and raised in Ghana before moving to Charlotte at 10 years old, Mensah believes she can make a difference through family medicine in communities near and far.
“For me, there is no separation between the community and medicine — to take care of a person, you have to understand who they are and what they face when they step out of the clinic,” she said. “I came into medical school with a strong interest in family medicine because I want to provide valuable health care to underserved populations in North Carolina and in Ghana.”
Mensah used her participation in the medical education and distinction teaching track to explore narrative medicine — the use of stories to create a therapeutic alliance between patient and physician — in helping students develop empathy and listening skills. She wants to continue that exploration during her residency.
“We all carry our own stories, but how do doctors represent their patients’ stories accurately? This has been an interest that has developed here at Brody, and I look forward to seeing how it transforms during residency,” she said.
Mensah is also a co-founder of the I Am First organization at Brody, a group that provides first-generation medical students with mentorship from community physicians.
“Even though COVID-19 shut down the world before our first official meeting, due to the diligence of the team members, we were able to keep the organization going,” she said. “I am excited to see how I Am First will continue to grow as it seeks out more mentors and maintains our community.”
Mensah is also a member of the Gold Humanism Honor Society for her service to the community. Her penchant for service, medicine and improving the world led her where she is today.
“Although I am nervous for my next step in my journey, I believe Brody has prepared me well to handle the stress and pressures of residency,” she said. “I will always remember to keep the patient and myself first as I learn the intricacies of residency — extending grace where it is needed. Ultimately, I think Brody has prepared me to begin to effectively address both the science and art of medicine.”
Read more through ECU News Services.
Edenton, NC – March 17, 2022 – Dr. Michael Waldrum, CEO of Vidant Health and Dean of the Brody School of Medicine at East Carolina University, joined Vidant Chowan Hospital President Brian Harvill at the Edenton Rotary Club meeting Thursday to discuss the exciting future of ECU Health and the impact high-quality health care has on the vibrancy of eastern North Carolina.
The presentation to the Edenton Rotary Club is one of several planned this spring and summer to meet with community groups throughout the region.
“Every time I visit Edenton, I’m reminded that Vidant Chowan is one of the most important parts of this community,” Dr. Waldrum said. “Edenton and the surrounding towns have a great hospital where they can deliver babies, receive high-quality care and build their sense of community. We value the role of rural hospitals and that is why it is so important for us to have conversations about how we can best deliver health care across the region.”

ECU Health – the joint enterprise between Vidant and Brody launching in the spring – was at the top of the agenda. Vidant Health enables the two organizations, which have worked collaboratively for years, to come together under a shared brand to provide streamlined care across the hospital system. A logo will be revealed in April and re-branding, which is expected to take months to complete, will begin in May.
Dr. Waldrum said ECU Health is the natural culmination of the two organization’s long partnership and shared mission of improving the health of eastern North Carolina. ECU Health will build on successful innovations such as the MOTHeRS Project, which is a grant-funded program through Vidant that connects mothers in rural areas to resources for nutrition, behavioral health needs and maternal fetal medicine resources. This program is beginning in Edenton and highlights the importance of collaboration to solve complex health issues in the region, Dr. Waldrum said.
“Having babies and being able to give birth here is really important to Edenton,” Dr. Waldrum said. “Babies that are born here are more likely to stay here when they grow up. We want to support that in an innovative way by providing access to care that meets the community’s need. The MOTHeRS Project is a great example of how Brody, Vidant and the future ECU Health will tackle complex challenges and bring a higher quality of care to the region.”
With Rotary Club members in attendance, Dr. Waldrum also spoke on the impact that access to care has on a community’s economic vibrancy. He shared that Vidant, which employs more than 13,500 team members, has a $4 billion economic impact on the region. Locally, Vidant Chowan has more than 500 team members and has a $61.3 million impact on the local economy. These numbers, Dr. Waldrum said, represent Vidant and the future ECU Health’s commitment to caring for the community.