The third Thursday of November is National Rural Health Day and ECU Health and the Brody School of Medicine are celebrating team members, faculty, staff and students by shining a light on the work they do to make a positive difference in the lives of the 1.4 million people living in eastern North Carolina.
A note from ECU Health CEO and Brody Dean Dr. Michael Waldrum: National Rural Health Day is a day to shine a light on the contributions of rural health professionals across the country. We created ECU Health earlier this year with high-quality rural health care in mind. The team members who work here truly personify the region and we wanted our name and logo to reflect that. We wanted our patients to know that the care we provide is backed by the educational excellence taking place at the Brody School of Medicine at East Carolina University. More than anything else, we wanted eastern North Carolina to know that ECU Health will always represent them. That’s a testament to the more than 13,500 ECU Health and Brody team members, who embody our mission and serve our communities. Thank you for your service and commitment to our organization, region and patients.

ECU Health serves a vast rural region made up of 29 counties and home to more than 1.4 million people. Like many rural regions, people across eastern North Carolina face a number of systemic socioeconomic challenges which have negative impacts on health outcomes. Perhaps most tragic of all, the region has wrestled for years with higher infant death rates than the state average, driven by difficult socioeconomic circumstances, barriers in access to care and fewer local resources to support expecting mothers.
Dr. Madhu Parmar, an OB-GYN for ECU Health, practices in Ahoskie. She helps facilitate countless healthy deliveries, but the ones that don’t go as planned stick with her the most. That is because many of the complications are preventable, and adequate access to perinatal care helps facilitate positive outcomes for both mother and baby. The unfortunate reality is that rural and underserved communities simply lack access to the perinatal care they need.
“This issue is very personal because I feel like there are not enough resources, people and attention placed on caring for mothers and babies in rural areas,” Dr. Parmar said. “I feel like rural mothers and babies are the ones that need care the most and we must do all we can to ensure they have access to that care. You hear about smaller hospitals closing down their OB units and that just increases the risk to mother and baby. If a community has access to these services, you see how the mother and the baby can thrive. That’s what we’re aiming for at ECU Health, access for all.”
Dr. Parmar says the primary challenges she sees in her patients stem from poverty. Data tells us that 1 in 4 mothers in eastern North Carolina live below the poverty line and 1 in 8 are uninsured.
“Because of poverty, patients are not as healthy,” she said. “Obesity and chronic diseases, such as diabetes and hypertension, are the things presenting difficult challenges for normal patients, and those conditions are even more challenging for pregnant patients. The reality is that we take care of a lot of high-risk patients in the East because many of our patients experience poverty.”
Across the region, more than 50 percent of the mothers delivering babies at ECU Health hospitals are clinically overweight. In Ahoskie, where Dr. Parmar practices, the average Body Mass Index (BMI) is about 40, nearly 15 points higher than the high range of a healthy person.
Keeping patients informed and educated about their health has been a key focus, Dr. Parmar said. Understanding illnesses and what to watch for is half the battle; a healthy mom often times leads to a healthier pregnancy.
“A nurse who specializes in diabetes care comes to our office once a week to educate our patients,” Dr. Parmar said. “She teaches them how to monitor their blood sugar and how to improve their diet so that we have optimal outcomes for the babies. She works with our nurses, too, and makes sure they’re looking through patients’ blood sugar diaries when they come in. The biggest thing we can do is be available to these patients.”
Women’s care close to home
At a time when many rural communities across the United States are losing access to obstetrics and women’s care services, ECU Health is doing its part to maintain and enhance obstetrics offerings in hospitals across the region.
According to the Sheps Center for Health Services Research, 183 rural hospitals have completely shuttered operations since 2005. When a hospital closes in a rural community, it makes it difficult for that community to thrive. One of the initial signs of trouble for an ailing rural hospital is a reduction or elimination of labor and delivery services.
Women’s services closures are often driven by the sustainability of the service itself. Staffing an around-the-clock unit is difficult due to the shortage of health care workers. The absence of nearby maternity services results in longer travel times, higher costs and medical complications.
In 2019, an average of 47 babies were born per day across the 29 eastern North Carolina counties. Those babies represent the future of the communities in which they are born and live, signifying the importance of maintain hospital-based obstetrics and labor and delivery services.
Dr. Daniel Dwyer, an OB-GYN at Outer Banks Women’s Care, said he remembers a time when many mothers in the area used to deliver babies on the way to the hospital. He said having rural hospitals close to where patients are can make the difference for positive outcomes, especially for mothers and babies.
For those living in communities where specialist care may not necessarily be only a few miles away, it is important to find ways to bring services directly to them. At the Outer Banks Women’s Care clinic, Dr. Dwyer said the services they offer keep patients close to home while receiving leading-edge care.
“We have begun to see patients for perinatology consultations, which is an important part of coordinating care for our highest risk patients.” Dr. Dwyer said. “Historically, it would take more than a half day for patients to get a consultation with a maternal-fetal specialist. In addition to the travel, the setting and staff would be unfamiliar for the patient. There is increased anxiety, cost and potential for loss of key information when patients travel for services that can be delivered in their trusted medical home. We hope to continue to leverage the technology and professional relationships to provide specialist care in rural settings. I think this is but one large step in the right direction toward reducing the disparities in access to the highest quality of care for our patients.”
Supporting hospitals across the region
High-quality perinatal care and labor and delivery services are synonymous with the ECU Health name. Dr. James deVente, associate professor at Brody and medical director of obstetrics at ECU Health Medical Center and Angela Still, senior administrator for women’s services at ECU Health Medical Center, have helped lead a perinatal outreach team that takes high quality training and best practices into other hospitals across the region, including facilities not affiliated with ECU Health.
Since 2012, the outreach team has visited every hospital across the region and has helped smaller hospitals better prepare for expectant mothers and new babies with serious medical conditions. From 2018-21 alone, the perinatal outreach team visited 18 different hospitals across the region, hosting 169 simulation days and educating more than 500 students on advanced life support training, emergency simulations, electronic fetal monitoring and more.
According to Dr. deVente, these efforts are a necessary part of improving care, reducing infant mortality and helping eastern North Carolina thrive.
“Data shows us that when a woman has to travel more than 50 miles to a hospital, her outcomes are worse. Data also shows us that businesses want to come to communities where labor and delivery services are present,” Dr. deVente said. “At ECU Health, we designed the outreach program and cover the cost of this work with those realities in-mind. If we are going to solve the infant mortality issues that our region faces, we are going to have to work together with health care partners across the East. I’m proud to say we are leading the way in that regard and the work is truly making a difference.”
Innovations to bridge gaps
It is no secret that eastern North Carolina is a vast rural region with long travel times between communities. An innovative program launched in 2020 at East Carolina University is helping to make women’s telemedicine, telepsychiatry and nutritional support services more accessible.
The MOTHeRs Project was first offered to patients at primary care obstetric clinics in Carteret County and has since expanded to ECU Health and other clinics in counties across the region. Through formalized partnerships with clinics, patients in the practices are cared for by both an ECU specialist and their local physician through a combination of telehealth and face-to-face visits.
Dr. Dwyer and Outer Banks Women’s Care were the third clinic in the ECU Health system to join the MOTHeRs Project. Maternal-fetal medicine and behavioral health care offerings for expectant mothers has been a much needed addition to the practice.
“We have identified access to mental health care as the greatest need in our rural communities. This need is increased during pregnancy and the post-partum period. Providing this service is a huge addition to maternal health care,” Dr. Dwyer said. “We have already begun to have mental health appointments in our office through the MOTHeRs Project. The feedback from our patients have all been very positive. This is just the beginning of learning how to give the needed specialized care in rural offices.”
Through its ongoing work, the MOTHeRS Project expects not only to provide care to those who need it, but also to generate new knowledge regarding how barriers to care can be better addressed. It aims to be a national model to ensure that every woman in rural America has a safe and healthy pregnancy and delivery.
“ECU Health, Brody and East Carolina University are truly pioneering high-quality rural obstetrics and women’s care services,” said Dr. Michael Waldrum, ECU Health CEO and dean of Brody. “Our hospitals and clinics provide excellent care in communities across eastern North Carolina. The perinatal outreach team trains other smaller hospitals on emergency care, best practices and more. Telemedicine innovations like the MOTHeRs Project makes patient-centered care more accessible. I’m proud of the work that all team members do to help our mothers, babies and communities thrive.”
Resources
Four students at East Carolina University’s Brody School of Medicine have been awarded the university’s most prestigious medical scholarship.
David Murray, Valentine Okafor, Arvind Mallikarjunan and Vaishnavi Siripurapu — all North Carolina residents — have been chosen for the Class of 2026 Brody Scholar and Brody Fellow award, valued at approximately $118,000.
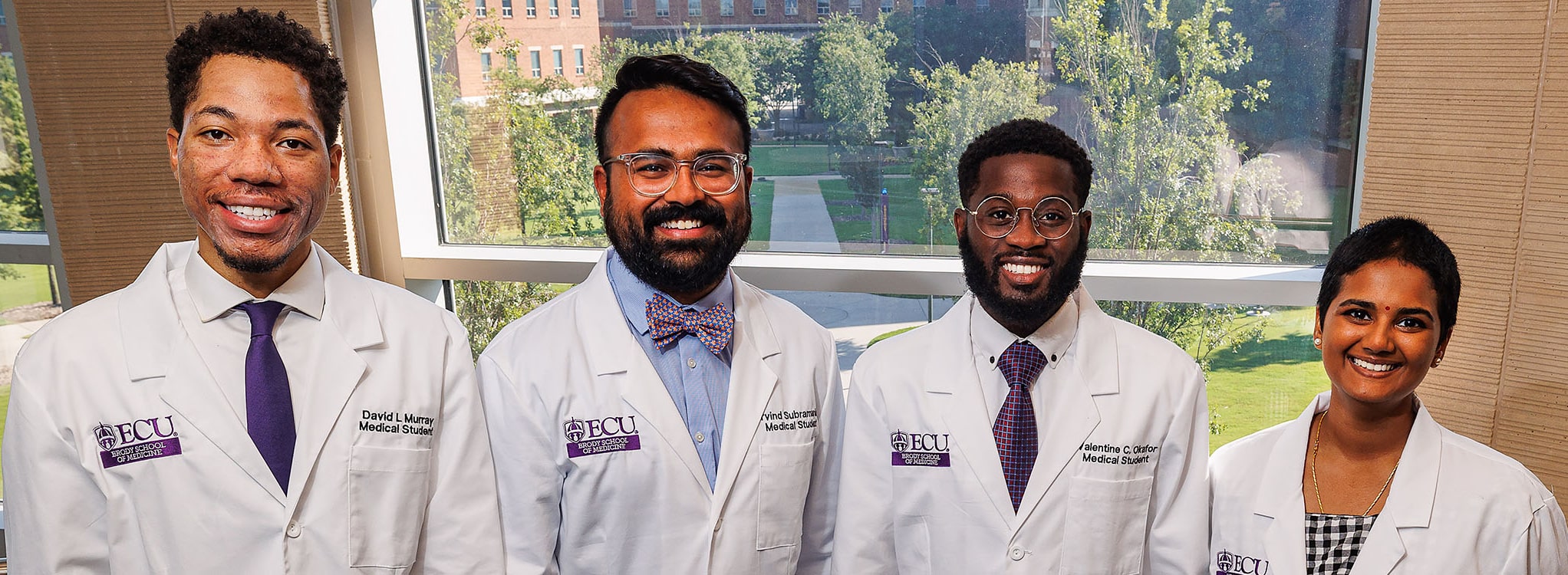
Each student will receive four years of medical school tuition, living expenses and the opportunity to design a summer enrichment program that can include travel abroad. The award will also support community service projects the students may undertake while in medical school.
Since the program began in 1983, 150 students have received scholarships. About 76% of Brody Scholars remain in North Carolina to practice, and the majority of those stay in eastern North Carolina.
“The Brody Scholarship is among the most distinguished in U.S. medical schools,” said Dr. Herb Garrison, interim president of ECU’s Medical & Health Sciences Foundation. “We are forever grateful to the Brody family for establishing and continuing to support the Brody Scholars program and appreciate the Brody Scholars who demonstrate constantly why they’re deserving of this tremendous support.”
David Murray
Murray, from Fayetteville, graduated from East Carolina University and earned a bachelor’s degree in biology with a concentration in molecular and cellular biology. He is also a member of the Phi Kappa Phi Honor Society.
He received ECU’s 2019 Undergraduate Research and Creativity Award for his work on developing new ways to make unique unnatural amino acids and putting them into proteins. He also presented his findings at the State of North Carolina Undergraduate Research and Creativity Symposium held at Duke University. Murray decided to pursue medicine after his cousin was hospitalized for an asthma attack.
“After missing weeks of school, my cousin lost his interest and drive to accomplish his dream of becoming a doctor,” Murray said. “I can’t help but believe that if he had received early care and management for his asthma, like I had, he would have never given up on his dream.”
Murray said he’s passionate about community health and family medicine and hopes to be a primary care physician that practices medicine in underserved, low socioeconomic communities.
“I hope to one day open many primary care clinics in communities that need them most,” he said. “In doing so, I believe we can achieve health equity and mitigate health disparities.”
He is the son of Thomas Rodney Murray and Kareema Cavallo of Canton.
Murray also said he believes being a Brody Scholar goes beyond him as an individual.
“In communities like mine, money is a limiting factor and is a reason to give up,” he said. “This scholarship shows that no matter your socioeconomic status or how much money your parents make or what community you come from, if you can persevere and continue to pursue your dream, you will get help.”
Valentine Okafor
Okafor is this year’s Brody Fellow, who hopes to use the opportunity to make an impact on global health.
Originally from Lagos, Nigeria, Okafor graduated from ECU in 2016 with a bachelor’s in biochemistry and a minor in chemistry. He is the son of Leonard and Chigozie Okafor.
In 2015, Okafor decided to study abroad to explore international health systems and to pursue solutions to health challenges around the world.
“I decided to attend this program after realizing the British National Health Services (NHS) was considered one of the best in the world,” he said. “During this program, I visited the World Health Organization headquarters and spoke with members of Parliament on issues regarding public health, the health care policies in the U.K. and ways in which health care systems in developing countries such as Nigeria can be improved.”
That same year, Okafor served as an ECU Global Ambassador; he was selected shortly after his study abroad experience, among other campus activities.
After graduation, Okafor worked full time as a scientist at Mayne Pharma and Thermofisher Scientific, where he performed various chemistry tests in the lab on life-saving drugs and medications, including vaccines to ensure safety and quality before they get the patients that need them the most.
While rewarding, another profession was his calling.
“I realized I wanted to go into medicine at the age of 9 when I first hand experienced and became a victim of the flaws of the health care system in my birth country, Nigeria,” Okafor said. “I was on the verge of losing my right leg, but ultimately was saved by the immense impact of the excellent physicians and their team in the U.K, I was inspired to dedicating my life’s efforts towards providing top quality health care toward people in underserved communities.”
Okafor has high aspirations for his Brody experience.
“During medical school, I hope to develop the professionalism, cultural perspective and humility needed to be an excellent physician through the opportunities provided by Brody School of Medicine,” he said. “To me, being a Brody Fellow is a huge privilege,” he said. “It gives me the freedom to pursue my passions and interests without the massive financial constraint and opens doors and opportunities for me that I would have not had the opportunity to explore.”
Arvind Mallikarjunan
Mallikarjunan wants to explore the parallels between health care and technology.
“I have a deep interest in building technologies to support the care of people living with a variety of diseases, and want to further my usage of technology to better administer care to patients in remote areas,” he said. “I also have interest in machine learning and AI (artificial intelligence) as a tool for predicting the health outcomes of patients.”
Mallikarjunan, from Durham, earned a bachelor’s degree in music and exercise/sport science from UNC-Chapel Hill and a master’s degree in physiology from N.C. State. He had his sights set on medical school even as he performed research at UNC’s Strength and Conditioning Laboratory and the Carolina Affective Science Laboratory. He was also a clinical research specialist for Duke University Health System’s Division of Hematology Sickle Cell Comprehensive Care Unit.
Addressing health problems like sickle cell disease motivates Mallikarjunan to take advantage of opportunities for research and volunteerism.
“While I always knew that I wanted to be in health care, I really solidified the reasoning behind becoming a physician during my time as a research specialist at Duke University,” he said. “Working with people living with sickle cell disease was an eye-opening and truly invigorating opportunity. I realized that there were so many areas in medicine that needed more support, and I felt the best way I could do that was by becoming a physician.”
Mallikarjunan is also an accomplished musician and volunteers to build bridges of access to technology for at-risk community schools across the state. He also founded Nanbar Health, a software suite built to communicate the disease experience of patients to their providers.
He is the son of Chitra Subramaniam.
Mallikarjunan hopes to channel his Brody Scholar experience into caring for the community.
“Being a Brody Scholar means so much to me; it truly is difficult to put into words,” he said. “It’s an amazing opportunity to serve our community without thinking about the debt that greatly affects so many physicians’ lives. It’s an amazing opportunity and one that I will never forget, and I am so thankful to ECU and the Brody family for this gift.”
Vaishnavi Siripurapu
Siripurapu applies a global perspective to her hopes for a future career.
“Throughout medical school, I hope to learn not just about medicine but about communities, cultures and social and systemic forces in order to become a skilled physician to meet the needs of my community,” the Mooresville native said. “I also hope to grow and be exposed to numerous new perspectives that will challenge my own worldview and ultimately help me develop further as both a person and a physician.”
Siripurapu earned bachelor’s degrees in biology and women’s and gender studies from UNC-Chapel Hill earlier this year. She attended the N.C. School of Science and Mathematics. Her journey to Brody afforded her the view of the world as a village.
“I am an immigrant from a very rural area of south India. I actually grew up without running water, wifi or stable electricity,” Siripurapu said. “Ever since I was young, I knew that I wanted to help the people around me as I grew up in a very community-based setting in a rural village.
“When I came to America, I lived exclusively in the American south and was exposed to community care and values of unity throughout my childhood and formative years. What pushed me to medicine was the idea of tangibly making a marked and meaningful difference in the life of another person within my community.”
Siripurapu, the daughter of Sreedevi and Narasimha Siripurapu, hopes to pursue a career in women’s health or a similar field. In the meantime, she wants to take full advantage of the Brody Scholar opportunity.
“For me, being a Brody scholar means that I have the freedom to focus my efforts entirely on the underserved communities that made me who I am today,” she said. “I hope to grow and develop alongside my cohort throughout our four years of medical school and give back to the people of North Carolina.”
In recognition of Veterans Day, ECU Health hosted a series of special events to recognize veterans from across the health system.
At each of the nine ECU Health hospitals, team members came together at 9:05 a.m. to recite the Pledge of Allegiance to honor the service and sacrifice of those who have served the country in the military.
The morning celebration at ECU Health Medical Center included a moment of silence and reflection as well as a role call for each branch of the military represented.
Mark Dunn, chief diversity, inclusion and talent management officer at ECU Health, shared his appreciation for veterans as the son of a U.S. Army veteran. He said hosting this event for the first time as ECU Health was a special opportunity to welcome new faces to a tradition at the hospital.

“We wanted to make sure we included our friends and family at the Brody School of Medicine,” Dunn said. “I wanted to give a special welcome to our Brody family as being part of ECU Health itself, as we continue to integrate and partner together. At one point we would have celebrated approximately 542 veterans from legacy Vidant, but as ECU Health today we celebrate approximately 1,400 veterans.”
The event gave special recognition to self-identified ECU Health veterans with a pamphlet listing their names.
Brian Floyd, president of ECU Health Medical Center and chief operating officer of ECU Health, offered a reflection and moment of gratitude for veterans and their families during the event — which is typically celebrated outside and near the United States flag that welcomes guests to the hospital — and today took place indoors due to inclement weather.
He said it is a special choice for our military veterans to continue to serve their country in health care, especially in a rural community.
“It’s so important to remember, it’s not just what you do in the military, but who you are in the military,” Floyd said. “That’s why we want to celebrate you today because what you choose to do is service, what you choose to do is honor other people, what you choose to do is sacrifice. At one point, that is military duty but you’re here in this organization because it carries through your life and you’re still serving and you’re still honoring and you’re still protecting.”
Transplant surgeon reflects on U.S. Army service
Dr. David Leeser, a transplant surgeon at ECU Health and a U.S. Army veteran, said he was raised to have a service heart.
When he was accepted into medical school, he decided to enlist in the U.S. Army.
“When I was in the Army, we had action in Afghanistan and Iraq,” Dr. Leeser said. “I ended up in Baghdad and it was during some of the surges and we took care of a lot of folks. It’s hard seeing young people in their late teens and early 20s injured in very profound ways that their lives will never be the same.”
Dr. Leeser said it was meaningful to him to be part of a team that helped send veterans back home to their families. He said his military experience is still something he carries with him today.
In gratitude
ECU Health would like to extend a heartfelt thank you to our veteran team members and all veterans for their service to our country.
It’s been sixteen years since Brent Carpenter’s life-changing injury.
“I dove into the pool with a shallow dive, hit the front of my head, and that knocked me out completely,” Carpenter said. “And I woke up on the surface where I couldn’t move any extremities.”
Paralyzed by the accident, the eastern North Carolina resident never gave up.
“The smallest little things can help you tremendously. So I have a saying that small steps are monumental gains,” Carpenter said.
Those small steps have served him well. Brent has since regained partial function of his hands and arms. He’s also tackled a massive personal goal, completing an annual charity event called “The Crossing” that takes place at Lake Gaston.
“The idea is that you’re crossing this part of the lake, which is give or take a mile, and however you want to – you can swim, you can kayak, you can float, paddle board, however you can get across,” Carpenter’s trainer, Susan Callis, said.
“A lot of people thought, ‘You are swimming this with a life-jacket, right?’ I was like, ‘Absolutely not.’ I wanted to do this just like everybody else was doing this and show people that anything’s possible,” Carpenter said.
Brent’s mindset and persistence served him well.
“We started out working on pool entry and exit,” said Callis, “and then working on water safety skills, working on breath control and lap swimming, holding his breath underwater.”
“It started as a half mile”, said Carpenter, “then I got three quarters there and then I got to the point where I was doing it consecutively during the week”.
It’s evidence-in-action that anything is possible with commitment, dedication and no shortage of cheerleaders.
“You do whatever you can to get across, first of all”, said Carpenter. “But I have always swam on my back when it comes to long distances. So when I came up to the finish line, I couldn’t see, you know, I didn’t have eyes in the back of my head. But when I turned around and Susan was right beside me like, you know, I heard the biggest applause I’ve had since playing sports when I was walking. To achieve a goal like that is, it’s priceless”.
It’s one impressive goal down with many more to follow.
“I think my goal each year is to make the world more accessible”, said Carpenter, “to not only my friends, but just people in my community that’s going through the struggle like me.”
Resources
A pink ribbon is one of the most recognizable symbols in health care. This is because breast cancer, the disease for which the color represents, is the second most common cancer in women, affecting one in eight women. Breast cancer develops when an abnormal growth occurs within the breast tissue, typically caused by uncontrolled cell growth in the breast. These rapidly growing cells form a potentially cancerous lump or mass and can spread to other areas, including lymph nodes.
Breast cancer often presents as:
- A lump or mass in the breast
- A change in size or shape of the breast
- A change in nipple appearance, including a newly inverted nipple or discharge
“I encourage everyone to know and understand what their breast tissue should look and feel like so they’re aware of any potential change,” said Dr. Karinn Chambers, breast surgical oncologist, ECU Health and ECU’s Brody School of Medicine.
It is never too early to begin self-exams of the breast, according to Dr. Chambers. However, women should begin breast cancer screenings annually at age 40, according to the American Cancer Society. This consists of a mammogram, which is an x-ray of the breast.

Dr. Chambers also emphasized that everyone, including men, should be aware of their breast health.
“Anyone can get breast cancer,” said Dr. Chambers. “I have seen breast cancer in people of different ages, the young and the elderly. Men can also get breast cancer.”
While breast cancer in men is much less common than in women, the American Cancer Society predicts that about 2,710 new cases of invasive breast cancer will be diagnosed in men in the United States in 2022.
“When a man is diagnosed with breast cancer, typically they present with the same symptoms as women – a new mass or lump within the breast,” said Dr. Chambers. “The causes and risk factors of breast cancer in men and women are also very similar.”
Breast cancer has both unknown and known risk factors. While experts still do not fully understand all of what causes breast cancer, genetics and lifestyle play a role in breast cancer.
“We recommend that women and men with a close family history of breast cancer undergo genetic testing to understand if they have a mutation on either the BRCA1 gene or the BRCA2 gene,” said Dr. Chambers. “BRCA1 and BRCA2 genes prevent proteins from rapidly growing out of control, which can cause certain cancers. For those who have the mutation, we do recommend prophylactic bilateral mastectomies, or removal of both breasts, as a preventative means to try to reduce their risk of breast cancer.”
While genetic risk factors are out of an individual’s control, there are behavioral changes one can make to lower their risk for breast cancer. The first is eating a healthy diet and exercising.
“Obesity is a big risk factor for breast cancer, and the rise of obesity in our population has led to an increased risk of breast cancer,” said Dr. Chambers. “Excess alcohol use can lead to increased risk of breast cancer as well.”
Experts highly encourage individuals to discuss screening with their primary care providers to understand their own risk for breast cancer based on their hormonal history, family history, health and age. The early detection of breast cancer allows for less invasive treatments, a greater variety of options and a greater potential to prevent the spread of breast cancer. When a person is unfortunately diagnosed with breast cancer, there are a variety of treatment options.
“The treatment of breast cancer consists of local tools and systemic tools,” said Dr. Chambers. “Local tools like surgery and radiation target the tumor directly. Systemic tools such as chemotherapy and hormone therapy can reach cancer throughout the body and may be used if the cancer has spread beyond the initial breast tissue.”
The bottom line?
“To prevent breast cancer, an individual should first discuss screening with their primary care providers so that they understand when and how often to get breast cancer screening,” said Dr. Chambers. “The second part of that would be to understand their own risk for breast cancer. Lastly, always remember to practice self-exams and know what is normal for your breasts. If you experience any changes, notify your primary care provider.”
Early diagnosis and a variety of treatment options have largely increased the odds of curing and managing breast cancer. ECU Health continues to offer 3D mammography at ten convenient locations throughout our region. Patients can take advantage of ECU Health’s free online risk assessment tool, talk with a provider and schedule a screening that meets their needs.
To learn more, please visit ECUHealth.org/breast-cancer.
Greenville, N.C. – ECU Health donated Stop the Bleed Kits to public schools in Tyrrell, Currituck, Northampton and Halifax counties as part of its goal to distribute these life-saving resources to public schools across eastern North Carolina. These kits provide resources such as tourniquets, trauma dressing, compressed gauze, gloves and training for school staff in the case of a bleeding emergency before professional help arrives.
“ECU Health is excited to continue expanding our distribution of Stop the Bleed Kits in the counties we serve in eastern North Carolina,” said Erika Greene, pediatric trauma program manager for Maynard Children’s Hospital at ECU Health Medical Center. “Time is of the essence for traumatic injuries, and early intervention can save lives. In rural areas like eastern North Carolina where the distance between schools and hospitals may be greater, these kits enable school staff to treat children early, improving chances of better outcomes.”
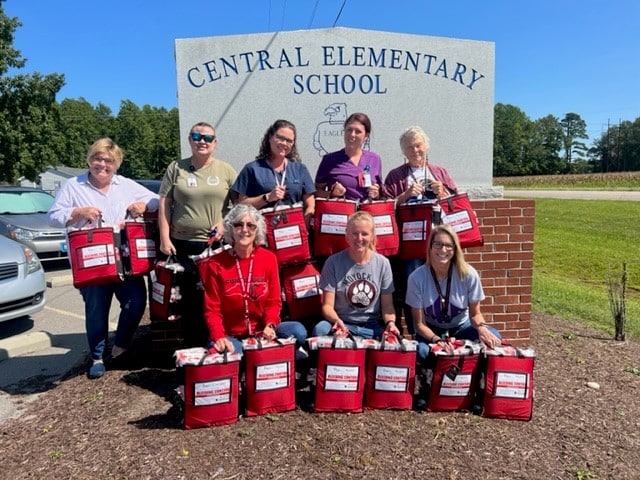
Stop the Bleed Kits are funded by Children’s Miracle Network with training provided by Maynard Children’s Hospital. ECU Health has donated more than 64 Stop the Bleed Kits to schools this year, with a total of 354 kits in 12 counties since the program started in eastern North Carolina. School nurses in each county help train staff to use the kits, which ensures more children can be treated with supplies that do not expire.
“We are thankful for the generous gift of Stop the Bleed Kits provided by Maynard Children’s Hospital for every school in Currituck County,” said Jennifer Solley, school nurse, Currituck County Schools. “An emergency in the school setting can occur at any moment. Stop the Bleed training and equipment in each school will equip the staff with the knowledge and tools needed to respond to any bleeding emergency. With these kits, we are prepared and able to reduce or eliminate the loss of life due to an emergent bleeding situation whether it be a single playground injury or a mass injury situation.”
Preventable blood loss is one of the most common contributing factors in trauma-related deaths. Approximately 40 percent of trauma-related deaths worldwide can be attributed to bleeding or its consequence. If bleeding is managed early, the chances of recovery and survival are much greater. The items in the kits help control the loss of blood, leading to positive outcomes for those who sustain injuries.
Pediatric patients at the James and Connie Maynard Children’s Hospital at ECU Health Medical Center got a little taste of Halloween as they had the chance to dress up and see ECU Health team members and community groups participate in a parade.
During the parade, floats with team members dress up as everything from Disney’s Up characters to safari themes poured by while patients and families had an opportunity to step outside of their rooms and enjoy some fresh air on a warm afternoon.
Quionna Lofton, the mother of pediatric patient Emoni Salvant, said it was a great experience for her and her daughter.
“It makes me feel really good,” Lofton said. “I didn’t think she would get to experience Halloween today because we are here. This is very nice and well thought out, it was just very lovely.”

Emoni said her favorite float was the Trolls characters and her mother agreed, since she got to see her daughter’s smile light up as it came by.
Various community partners came out to bring a little joy to the youngest patients at ECU Health Medical Center. The Greenville Fire Department brought two trucks to the parade while the Pitt County Sherriff’s Office showed off a safari-themed float. The Down East Wood Ducks baseball team mascot, DEWD, gave patients a big wave from the back of a Jeep while ECU’s mascot, PeeDee the Pirate, interacted with patients and families.
Karolyn Martin, Miss North Carolina 2022, was on hand for the parade as well. She said it was a great experience, and a personally meaningful cause for her.
“My younger sister actually has Crohn’s Disease,” Martin said. “When she was diagnosed, she was in a hospital for about eight months of her year in 8th grade. I know how important it is for families to have people come that care about their children and also to celebrate the people that are making sure children are safe and healthy – that’s so important and why I was so excited to be here.”
Patients had the opportunity to select a costume from those available in the Maynard Children’s Hospital and got to select a party favor, including books and other fun activities.
Chloe Williams, a Child Life intern who helped organize the event, said it was special to see the smiles on the faces of patients and families after the time spent planning.
“I think it’s great. I think it provides a sense of normalization to the hospital experience, because a lot of the time they don’t get to have a Halloween if they’re here,” Williams said. “Just to provide something that they can enjoy and the parents can enjoy, too, is a really special thing.”
Williams said it’s also something team members look forward to each year. Whether they are dressing up and riding along on a float or out in the sea of children, it’s a welcomed opportunity to see patients in their natural setting – enjoying time as a kid.
With an audience of more than 90 Brody School of Medicine at East Carolina University first-year medical students, leaders from ECU Health and Brody discussed the power of storytelling and narrative medicine during the 14th Annual Jose G. Albernaz Golden Apple Distinguished Lecture.
Narrative medicine is an increasingly popular technique that utilizes storytelling for health care providers to understand their patients as people and help process their own emotions around their work. At ECU Health, where compassionate care for patients and for the care team are foundations of how the organization meets its mission, the benefits of narrative medicine can make a difference in the clinical setting.
For first-year Brody students, the lecture provided an opportunity to learn about the value of narrative medicine so that they can apply it to their own education and future careers.

Dr. Christina Bowen, chief well-being officer of ECU Health, was once a first-year Brody student herself. In her opening remarks, she challenged students to take up narrative medicine early in their journey to becoming providers.
“The profession of medicine brings cases that will touch your hearts with much joy and sorrow. Write those stories down,” Dr. Bowen said. “These stories will be with you the rest of your medical career. Embracing the power and importance of these stories will support your emotional well-being and your growth into an excellent physician.”
Dr. Sharona Johnson, the nursing Advanced Clinical Practice administrator at ECU Health, served as the keynote speaker for the event. She said storytelling is key to understanding our humanity and helps leave a legacy for all people.
Dr. Johnson, who is a published author, is an advocate for narrative medicine – both to understand patients and as a well-being tool to get her own feelings down on paper.
“We’re learning that stories are important because we’re telling our stories,” Dr. Johnson said. “Physicians and health care professionals are writing books. We’re finding that our life has to have meaning. You can’t go through your life without thinking about, ‘Why am I here, what is the purpose, why is this patient sitting in front of me?’ It has to have meaning.”
Dr. Jason Higginson, chief health officer of ECU Health, said he received a written note from the first patient he gave a full clinical exam to in medical school. He said he can still picture himself in the exam room and remembers the patient frequently because of the heartfelt note the patient shared. He reflected that he wished he’d known more about narrative medicine as a young doctor so he could have captured more experiences like this from early in his career.
The relationship between ECU Health and Brody is important for many reasons. The opportunity for experienced providers to share valuable lessons with medical students in a clinical setting is one of the special benefits. Dr. Michael Waldrum, CEO of ECU Health and dean of the Brody School of Medicine, said the teaching offered at Brody and ECU Health stretches beyond the walls of the classroom.
“This was a really important lesson today for students and a great reminder for anyone already in health care,” Dr. Waldrum said. “Narrative medicine and storytelling help in many aspects. Brody School of Medicine concentrates on producing physicians that actually understand humanity. I’m really proud of that.”
Dr. Waldrum said that understanding humanity and human interaction is what led him to being a pre-med English major as an undergraduate.
Learning the humanities, he said, helped lay a foundation for him as a person and care provider. The lessons learned as an English major were reinforced in his first clinical rotation during his third year of medical school when a mentor told him to learn something from each patient, whether it is a personal or medical fact. He said that stuck with him and taking it into action paid off.
“That’s the story of humanity and history, understanding and respecting differences,” Dr. Waldrum said. “Stories are about history and looking backwards, but it’s also about creating an optimistic and positive future. That’s what we’re doing here: creating a new health system, evolving our school of medicine, always changing and making sure that we meet our communities needs and that we educate the best humans on the planet.”
The Albernaz Golden Apple Distinguished Lecture series is a great example of how ECU Health and the Brody School of Medicine collaborate to bring excellence in the clinical and academic setting for the betterment of eastern North Carolina.
Greenville, N.C. – After an extensive search and interview process with stakeholders across the organization, ECU Health is pleased to announce and welcome Andrew (Andy) Zukowski, MBA, as the health system’s new chief financial officer (CFO), effective Nov. 28.
 “It is my great honor to welcome Andy as the next CFO of ECU Health,” said Dr. Michael Waldrum, CEO of ECU Health and dean of the Brody School of Medicine at East Carolina University. “Andy brings more than 20 years of experience in highly-matrixed health care organizations with expertise in value-based care models and strategic financial planning and analysis that drive positive results. In addition to Andy’s vast financial background, his mission-focused mindset and passion for serving others are attributes we value and are at the core of who we are as ECU Health.”
“It is my great honor to welcome Andy as the next CFO of ECU Health,” said Dr. Michael Waldrum, CEO of ECU Health and dean of the Brody School of Medicine at East Carolina University. “Andy brings more than 20 years of experience in highly-matrixed health care organizations with expertise in value-based care models and strategic financial planning and analysis that drive positive results. In addition to Andy’s vast financial background, his mission-focused mindset and passion for serving others are attributes we value and are at the core of who we are as ECU Health.”
Financial operations are a critical component of the joint operating agreement between ECU Health and Brody which outlines the goal of establishing a shared leadership and shared services model to support the enterprise. The CFO position will directly report to the health system’s CEO and have additional oversight and responsibility for Brody’s financial services and structure. This structure creates a more effective approach to integrating financial services and realizing efficiencies that will benefit patients and care teams across the organizations.
“This is an exciting time for me personally and professionally,” said Zukowski. “ECU Health and the Brody School of Medicine are both synonymous with rural academic and clinical excellence. I look forward to joining the leadership team at ECU Health to advance the important mission-driven work positively impacting the lives of the 1.4 million people who call eastern North Carolina home.”
Prior to joining ECU Health, Zukowski served as UNC Rex Healthcare’s chief financial officer since 2016. Zukowski’s arrival to ECU Health comes in succession of current CFO David Hughes’ planned retirement Dec. 30 after serving the organization and eastern North Carolina for 25 years.
“David’s leadership and expertise were instrumental in our ability to lay the building blocks that have positioned ECU Health to successfully realize its vision of becoming a national academic model for providing rural health care,” said Dr. Waldrum. “I greatly appreciate David’s contributions to our region and wish him the very best in his retirement.”
ECU Health looks forward to welcoming Zukowski to eastern North Carolina where his expertise, leadership and partnership will help the organization continue to deliver high-quality care as well as educate and train the next generation of health care professionals.
It’s no secret prostate cancer is one of the most common cancers among men. In fact, nearly one in eight men will be diagnosed with prostate cancer in their lifetime. What many may not know is if caught early, prostate cancer can be easily treated and even cured. That’s why experts at ECU Health are urging men who have delayed getting a prostate cancer screening to return to their regular screenings to prevent advanced prostate cancer diagnoses.
The prostate, which only exists in men, is a walnut-sized gland tucked under the bladder and is involved in the reproductive process. The prostate can develop cancer and is one of the leading cancers diagnosed in men.
“We love to catch prostate cancer before there are any signs or symptoms. In order to do that, you need a blood test called a prostate-specific antigen, commonly known as a PSA blood test,” said Dr. Caroline Ames, ECU Health urologist. “Because the prostate is tucked up under the bladder, you may not have symptoms until it’s advanced.”
Dr. Ames says if prostate cancer grows large enough that it is causing symptoms, there may be blood in the urine or semen or difficulty urinating. More advanced stages can present symptoms such as bone pain, weight loss and swollen lymph nodes.
“Many of the people we take care of in eastern North Carolina are high risk for prostate cancer, especially African American and Latino men between the ages of 45 and 65,” said Dr. Ames.

African American men are more likely to develop prostate cancer and twice as likely to die from prostate cancer, as compared to non-Hispanic white men, according to the Office of Minority Health.
“This is likely due to genetics, lack of access to health care, general mistrust in health care and socioeconomic factors,” said Dr. Ames. “Those men with a family history of prostate cancer and men over the age of 65 who take one or two medications and are overall healthy, need a PSA screening every year.”
The screening process may look a bit different from what many may have experienced before. Dr. Ames, along with many other urologists, now do the blood PSA screening as the first line of screening. These providers will do a physical exam after the PSA screening indicates cause for concern. According to Dr. Ames, this method has brought in many more men for prostate screenings that may have not gotten one before due to anxiety or hesitancy of the physical exam. Men are encouraged to talk to their provider about the screening process.
“If you are diagnosed with prostate cancer, we will look at all of the treatment options available,” said Dr. Ames. “While some with low-risk disease may not need aggressive treatment, there are options available such as hormone therapy, radiation or prostate removal.”
The best treatment is prevention. Eating a healthy diet high in fruits and vegetables and low in processed foods and red meat can help reduce your risk of prostate cancer, along with quitting smoking.
“Obesity and smoking are two of the leading causes of prostate cancer,” said Dr. Ames. “Once you have been diagnosed and treated for prostate cancer, obesity increases the risk for the cancer coming back in the future.”
During the COVID-19 pandemic, screenings across the board significantly lowered. This is a significant concern amongst medical experts.
“Many people postponed their cancer screenings, and we are very concerned about that,” said Dr. Ames. “This increases the chance for a larger number of patients to be diagnosed with advanced or later stage cancers, including prostate cancer.”
The bottom line?
“You need to return to your cancer screenings, whether it be prostate, breast, lung or colon cancer screenings, especially if you skipped them during COVID-19,” Dr. Ames said. “Early detection can save lives.”
Resources





















