Each day at Vidant Health, incredible nurses go above and beyond to care for the patients and families of eastern North Carolina.
In February, ECU Health Medical Center (VMC) volunteer Frank Crawley had a moving experience with nurse Felicia Parker at ECU Health Cancer Care that he felt compelled to write about.
“What you don’t know is you did something to me that day,” Crawley said to Parker, as the two met again exactly a month after their interaction. “You moved me to do some things that I’ve wanted to do for a long time. That’s to write about some things having to do with this hospital and how much it has meant to me.”
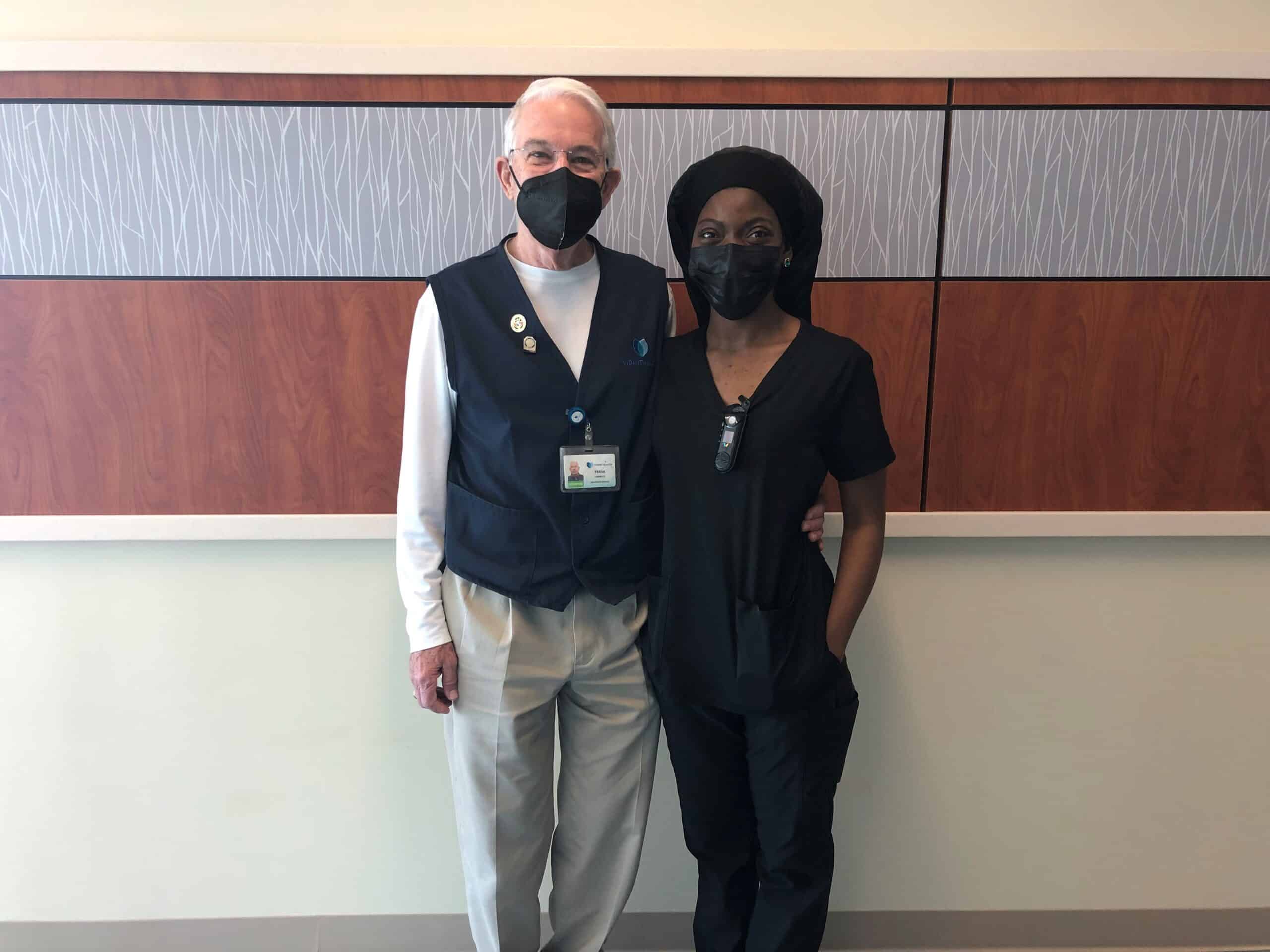
This National Health Care Volunteers week, we are proud to share the below story written by Crawley after his experience at VMC.
“On the morning of Feb. 15, 2022, a call came to Patient Escort to bring a wheelchair to the Cancer Center, room 418, to transport a patient to the Dental Clinic. I took the call. When I arrived, I knocked on the door, opened it, greeted the occupants and announced that I was there to take the patient to the Dental Clinic. Lying in the bed was a frail, elderly man. Standing by his side was his wife, who immediately said there was no way her husband was able to make the trip to the clinic in a wheelchair.
I left the room and located the nurse assigned to room 418, whom I later learned was Felicia Parker. She and I both entered the room. Ms. Parker explained to the patient’s wife that her husband desperately needed dental work. The wife seemed very concerned that her husband lacked the strength to make the trip, that his blood pressure would drop and that he could have a seizure, particularly if taken in a wheelchair. She said that he might be able to make the trip in his bed. The soft-spoken Ms. Parker explained that the bed was too large to transport into the clinic. Additionally, she said that to alleviate the wife’s concerns, she would accompany her husband to the clinic, assuring her that every precaution would be taken. First, she explained that we would exchange the Staxi for a Stryker wheelchair, carry an oxygen tank with us, along with a blood pressure/heart rate attachment to monitor her husband’s vital signs.
The wife began to weep quietly. She walked into the bathroom and continued to sob, fearing for the welfare of her husband. Ms. Parker followed her to the bathroom. She spoke softly, lovingly to the patient’s wife, hugged, consoled and reassured her that we would take every precaution to see that her husband made the trip to the clinic without incident. Still hugging, Ms. Parker told the patient’s wife that she would call her once we reached the clinic. I was so impressed at that moment with the love, patience, caring and empathy Ms. Parker showed her — far beyond what I had expected to witness that day. With the wife comforted and reassured, Ms. Parker and I located a Stryker chair, added an oxygen tank and a vitals’ monitor. Next, Ms. Parker said that she was raising the bed to a sitting position so that the patient could sit upright for a few minutes and adjust to the change in position. Doing so, she explained, we would be able to see whether his blood pressure and heart rate would respond favorably to the positional change. Next, Ms. Parker and I moved the Stryker chair next to the bed and slowly moved the gentleman’s feet off the side of the bed. All went well — at first.
Within seconds of moving his feet off the bed, there was a sudden drop in the patient’s blood pressure and a change in heart rate. Carefully but quickly, Ms. Parker moved the patient’s feet back onto the bed and slowly lowered the bed. She immediately left the room and called for backup help — not calling for a “code blue” but the next level below, as I heard her say. Within a few minutes, the room was filled with attending physicians, nurses and aides. I quickly moved back, stepping out of the room to allow Ms. Parker and the medical staff space to work. Within what seemed like only a few minutes, the patient’s vital signs were restored to normal, and the room was calm again. Ms. Parker then turned to the patient’s wife, hugged and comforted her.
With the room restored to calm and the father’s vitals stable, Ms. Parker came to me and thanked me for my help.
“No,” I said. “Thank you for allowing me the privilege to witness, firsthand, nursing at its very best.”
Not only was Ms. Parker highly competent, as evidenced by the technical skills she displayed, she also possessed that rare ability to sincerely comfort, console and empathetically connect with the very distressed patient’s wife. Empathy is near impossible to teach. Neither can it be faked. Deeply moved and with tears in my eyes, I hugged Ms. Parker.
“Never had I expected to report to volunteer duty Tuesday morning and see the loving, compassionate face of Jesus on display,” I said.
That day was most rare and wonderful, and I knew it.
After writing down his experience, Crawley shared this with the volunteer team and eventually it found its way to Parker. When she received the email, she had her daughter read the story to her sons. Parker said she was moved by him sharing his experience with her and her family.
“It’s nothing that I gave a second thought to – it’s just what we do every day,” Parker said, who will celebrate three years in the system in June. “Sometimes we kind of don’t look at what we do, how it impacts others. Especially, we feel like it’s just something that we’re just supposed to do. You’re supposed to get up, you’re supposed to greet people when we see them. We don’t think anything of it. That’s what it was for me. It was just, ‘Hey, what you do does matter.’”
Crawley said he has been volunteering at the medical center for nine years. Previously, he was an education professor at East Carolina University.
“In the busyness of life, and I think it has a lot to do with my age, I look for those moments that I can connect with people or when I can see them connecting, because I believe that’s what we were born to do,” Crawley said.
“We do a lot of things for which we get paid and it’s difficult to find something in you down deep that in that busyness,” Crawley said. Then looking at Parker, he continued, “I know you had lots of other patients, but in that busyness to console the woman who wasn’t your patient. You saw something there that was a greater need and you met that need. That was just powerful.”
We are so proud to have experiences like this unfold along the halls of Vidant hospitals each day. Thank you to the care teams, volunteers and team members who serve eastern North Carolina. If you are interested in joining the Vidant team, visit our Careers site.
Greenville, N.C. – April 14, 2022 – Vidant Health and East Carolina University are excited to announce a logo for the ECU Health system, which will launch in the region starting in May.
“Eastern North Carolina’s vibrancy depends on strong collaboration between the institutional pillars that have long represented this region’s unique needs,” said Dr. Michael Waldrum, Vidant CEO and dean of ECU’s Brody School of Medicine. “The ECU Health logo is a symbol of our shared commitment to transforming and elevating health care for millions, training the providers of tomorrow, collaborating with community partners to solve complex issues and bringing clinical innovations that improve the lives of those who proudly call this region home.”

The ECU Health logo captures the essence of an innovative regional health system comprised of more than 13,000 dedicated health care workers, a thriving university, current and future generations of doctors committed to caring for North Carolina and the unwavering commitment of two organizations working collaboratively to transform the East.
“It is exciting to be a part of ECU’s continued transformation as we work to build pathways for sustained excellence here in Greenville and the region,” said ECU Chancellor Philip Rogers. “This partnership strengthens our institutions’ shared mission and ultimately betters the communities we serve. Sharing the new ECU Health logo begins an exciting chapter as we work collaboratively to build the health care enterprise for the region and expand our reach further into eastern North Carolina.”
The rebranding process for most Vidant entities is expected to begin in May and will take several months to complete. The Brody School of Medicine’s name will not change.
Naming conventions are as follows:
Hospitals:
- ECU Health Medical Center
- ECU Health Beaufort Hospital – A Campus of ECU Health Medical Center
- ECU Health Bertie Hospital
- ECU Health Chowan Hospital
- ECU Health Duplin Hospital
- ECU Health Edgecombe Hospital
- ECU Health North Hospital
- ECU Health Roanoke-Chowan Hospital
- The Outer Banks Hospital
- ECU Health Maynard Children’s Hospital
Other entities:
- ECU Health Physicians and ECU Physicians: the naming of the practice groups will be shared at a future date.
Vidant and ECU have a rich history of collaboration in health care, education and research. Vidant’s role as a regional rural health care leader, and Brody’s status as North Carolina’s leader in graduating physicians who practice in state, in primary care and in underserved areas is a natural partnership that will advance the combined mission of ECU Health.
ECU Health will strive to more effectively and efficiently address current issues facing the region – such as health disparities and care delivery obstacles – while also better anticipating future health care and educational needs.
“The rebranding to ECU Health is symbolic of the importance and longstanding cooperation of ECU’s Brody School of Medicine and Vidant Health. Together, we have long stood side by side advancing the health delivery, research and education mission for eastern North Carolina,” said Dr. Jason Higginson, executive dean of the Brody School of Medicine. “Having one brand will make our close and important relationship apparent to everyone.”
In February of 2018, Pol Solanelles had his life’s plan in place.
The Barcelona native had recently completed his last year of eligibility competing in track & field and cross country as an East Carolina University student-athlete. Now on his to-do list: finish the last semester of his Master of Business Administration degree, get into a doctorate program and land a job at a university in the United States.
He’d made a home for himself over four years in Greenville and everything was on time and on track. Until his accident.
While riding his bike home from ECU’s campus on Feb. 12, 2018 and just a hundred or so yards from his residence, Solanelles fell off of his bike and was run over by a car. He suffered a traumatic brain injury, broke many bones and had many hurdles in front of him as he was rushed to Vidant Medical Center (VMC).

He had surgery that same night and was placed in an induced coma for nearly a month while his body recovered from the crash. When he woke up and his recovery process began, Solanelles said he never questioned his plan moving forward.
“The accident happened and the only thing I could think of was, everything is going to be delayed,” Solanelles said. “I wasn’t thinking, ‘I’m not going to be able to do that.’ I was just upset because everything was going to be delayed.”
He described the beginning of his recovery as starting from scratch.
For his brain injury, it started with simple memory and speech exercises. In the early days after coming out of his coma, he was still confined to his bed but started to stand up and walk as his rehabilitation progressed.
He said that as a former athlete he felt confident in getting his body back on track over time. So, during his recovery, he focused heavily on his mental exercises and keeping his brain sharp.
“I was pretty obsessed with getting back to normal,” Solanelles said. “With my body, it was like, ‘OK, I really don’t care that much but my brain, I’m going to have to rely on it for the rest of my life.’ I focused a lot on my head with the exercises that we were doing.”
His time at VMC and with the rehabilitation team was instrumental to his recovery, he said. It was a rigorous program and one that let him re-learn quickly.
“Vidant had a very proactive approach of trying to deal with as many things as possible on a short time window, because that’s when the brain is more susceptible to any learning process,” Solanelles said. “Kind of like when we are kids, it’s easier to learn things. I was doing maybe six hours of rehab every day. It was like my whole day and I would finish exhausted.”
Solanelles said those long, challenging days of rehabilitation were made easier a few different ways. He felt his time as a student-athlete helped him recover more quickly between rehabilitation days. He was also highly motivated to get back on track with his studies and to complete his degree program.
Perhaps most importantly, though, was his positive attitude and the support of the rehabilitation team at VMC.
“It was very important to have an optimistic outlook from the beginning,” Solanelles said. “The staff in the rehab department, they were very helpful in keeping me in a good mood. I would have fun most of the time doing the exercises or just chatting with them. That helped to stay motivated and, again I think I got back to normal.”
Missy Moore, a physical therapist at VMC, said her job is constantly motivating as she sees patients through their recovery process.
“The best part about working in rehab is the connection you get to make with the patients and their families,” Moore said. “You get to spend time with them and work with them every day, and they become part of your rehab family. You experience their highs and lows with them. Whatever injury someone has suffered is just a speed bump in their story. Watching them move over the hump and keep on driving is why I love what I do.”
Speech-Language Pathologist at Vidant Medical Center Amanda Rice said the compassion for each patient’s journey is vitally important in rehabilitation.
“It’s important to remember that as therapists what we encounter may be part of our every day and what we do,” Rice said, “but that is not true for our patients. Understanding the patient’s experience and how we can best support them in their journey and recovery is important. I feel fortunate to be a part of that journey.”
After four months at VMC, Pol returned to Barcelona and spent two additional months in a hospital in his home city and completed his rehab. As things slowly started to return to normal, his academic and career goals came back into view. He started with some online courses to work back toward his MBA and returned to Greenville to complete his program in the spring of 2019.
Now, things are back on time and on track for Solanelles. He started his doctoral program in business management at the University of Mississippi in August of 2019 and is currently halfway through the program.
March is Traumatic Brain Injury Awareness Month and Solanelles said through all of his rehabilitation and experience with friends, family and support groups that talking about his experience has been a source of comfort for him.
“Talking about it helps a lot. I’ve always been able to talk about it as if ‘Oh, I went to do groceries.’ That has helped me deal with it with humor,” Solanelles said. “People get surprised about that. I think talking about it helps both yourself and your family. That was healing.”
Resources:
Trauma Survivors Network at Vidant Medical Center
Two Vidant leaders were recognized on Friday, March 18 and inducted into the East Carolina University (ECU) College of Nursing Hall of Fame along with seven other recipients.
Dr. Julie Kennedy Oehlert, chief experience officer at Vidant Health, and Dr. Kamilah Williams, administrator for nursing professional practice, development and clinical education at ECU Health Medical Center (VMC), were each honored last week after being nominated by colleagues and accepted into the ECU College of Nursing Hall of Fame.
Dr. Williams is a 2005 graduate of the ECU College of Nursing and an eastern North Carolina native. She said she is proud to serve the community she calls home and the induction was a great honor.

“I’m so humbled and proud to be a Pirate nurse,” Dr. Williams said. “I’m proud to give back to my community here in eastern North Carolina, where I grew up as a young child. It’s an honor to serve and care for the population that I grew up with. I’m just grateful.”
Dr. Williams is tasked with developing nurses in her role at Vidant. Under her leadership, VMC achieved accreditation for the Nurse Residency Program and has developed an International Nurse Fellowship Program.
She said she loves what she does and is happy to give back to her profession and region through her role.
“When I think about the mission of our organization and being able to improve the health of the people here in eastern North Carolina, it’s exactly why I do what I do,” Dr. Williams said. “As a young child, I always knew I wanted to be a nurse and be able to give back to my community. Now in my role, to be able to help develop future nurses, it’s just a humbling experience.”
Dr. Julie Oehlert has used her experience as a nurse to improve the experience of patients, families and Vidant team members across eastern North Carolina. Dr. Oehlert came to Vidant and eastern North Carolina in 2016 and said the recognition made her feel at home.
“For me, I was so humbled and excited to be recognized with other Pirate Nurses,” Dr. Oehlert said. “I came from outside of Vidant but my heart is with Vidant and ECU. I feel welcomed into this community. I was so overwhelmed when I was nominated and accepted.”
Dr. Oehlert said she is proud to be part of a health system with so many Registered Nurses as leaders in different areas. With nurses in non-traditional roles lending their health care expertise and compassion for patients and families, the nursing heart can be seen in many facets of the health system.
“I don’t get to work directly with nursing but the nursing heart of all the leaders that have RNs behind their name, is pretty darn special at Vidant,” Dr. Oehlert said. “Many of our presidents and executives have that RN heart and that means we are always caring about our communities, we always have a holistic view on care and I love that.”
With the nine inductees for 2022, the ECU College of Nursing Hall of Fame that started in 2011 has grown to 150 members.
One of the past inductees on hand for the event was Dr. Daphne Brewington, senior vice president nurse executive at ECU Health Medical Center.
“It’s just been an amazing night and both Dr. Williams and Dr. Oehlert are so deserving of this award,” Dr. Brewington said. “I’m so proud that they have been inducted into the ECU College of Nursing Hall of Fame. I was inducted in 2018 so it’s just really special and surreal to be able to support colleagues that are on this journey as well.”
Inductees into the Hall of Fame also help fund a scholarship for ECU College of Nursing students, which has raised $170,000 throughout the years to support the next generation of nurses.
Learn more about the ECU College of Nursing Hall of Fame on ECU’s website.
Work culture makes a difference in recruitment, retention and team well-being, and all health care organizations strive to offer a more loving work environment where team members can thrive.
Vidant Health Chief Experience Officer Dr. Julie Oehlert joined the SEE YOU NOW podcast, from Johnson & Johnson and American Nurses Association, and discussed leading organizational change on Episode 64: Reporting Powers: Leading With Love.
A new, loving culture
Dr. Oehlert said “power-over” or hierarchical relationships are at the core of many relational issues, and missed opportunities in health care. She encourages all of health care to work together with team members on culture innovations.
“I think most organizations use the definition of culture of ‘How we do things around here,’” Dr. Oehlert said. “That cultural definition is like you’re a fish swimming in a bowl. It is not actionable. We believe that culture is defined by how our relationships are structured with each other – how we treat each other, how we treat patients, how we treat our community, and that definition is very actionable and everyone can impact the culture.”
As team members partner to create a new, loving environment, team and organizational goals become much more achievable. Dr. Oehlert said measures such as whether team members are afraid of reporting safety events, if they feel heard by their manager, and if the community believes the health system is their partner, are key indicators of a positive, changing culture.
Dr. Oehlert noted the importance of looking to an organization’s own team members to change cultures and innovate in their own space. She believes that health care can improve if they listen to their team members who want to have a voice in their own work environment.
“You don’t need other people to help you with your culture. Do you know you have innovators sitting around in your hospital? They’re everywhere,” Dr. Oehlert said. “Your EVS and food services workers will redesign your food delivery in a hot minute. Don’t bother to pay a consultant. Your innovation awaits you if you walk into your departments. Give them an environment and ask them, listen to them and they will design beautiful things.”
It starts at the top
A culture shift in health care must include changes to leadership development. Transformational leadership is full of love, kindness and mentorship.
So, she and the Organizational Development department felt they needed to carve its own path.
“I called our chief operating officer and I had all of these books sitting around me, you know your scholarly books on leadership development,” Dr. Oehlert said. “So I’m looking at all these different models and I’m putting my head in my hands and I’m like, ‘None of these are going to take us where we want to go. We’re going to have to develop our own leadership curriculum and our own leadership framework.’”
A team came together and different and new frameworks were pulled together to create a unique system for Vidant to develop talented team members and grow leaders.
This new system was necessary to transform and later maintain a culture of love, empathy and power-with attitudes from organizational leaders.
“Leadership development is so important because the leaders are at the top of the hierarchy; if they are perpetuating fear or dominance, whether intentional or not, because some leaders were just taught to lead that way, that has to shift,” Dr. Oehlert said. “A new leadership way of being has to emerge.”
Policies reflect culture
Policies are a reflection of the workplace culture and policies can frequently be outdated and not in line with the culture of the organization.
Dr. Oehlert said as the culture shifted, the organization needed to review policies and procedures.
“It’s amazing how many policies, once you read them with a lens of caring and love that you realize – ‘This is terrible. Why would we have this policy?’” Dr. Oehlert said. “Are your policies by their nature punitive? How do you handle mistakes and coaching and errors with your team members? Do you have grace when they are humanly failing? Do you have grace for their mental health issues? You really have to dismantle that.”
Looking for more?
Find and listen to the SEE YOU NOW podcast, Episode 64. Reporting Powers: Leading with Love, wherever you get your podcasts.
Read more on Dr. Oehlert’s previous appearance on the SEE YOU NOW podcast.
Vidant Health continually reinvests dollars back into the health system to fulfill our mission of improving the health and well-being of eastern North Carolina. With a focus on team member and patient experience, we reinvest in our care environments, including technology and unit aesthetics throughout the health system every year.
The Renal Dialysis Unit (RDU) at ECU Health Medical Center (VMC) moved to a new, reconstructed space on 1 East with upgraded amenities, more space and increased privacy for patients.

The RDU provides numerous treatments for patients including hemodialysis, peritoneal dialysis and apheresis. Laura Respess, manager of Patient Care Services, said hemodialysis (or the removal of waste from the blood) involves two venipunctures if the patient has a graft or fistula, or by accessing the central line, and then hooking the patient to a dialysis machine. Blood is pulled out a little at a time, goes through the dialyzer to remove toxins and/or fluid and is then returned to the patient. Intensive treatments such as hemodialysis mean that patients spend a lot of time in the hospital, and the new RDU offers a more peaceful and private experience for patients while receiving treatment.
The new space on the first floor offers easier accessibility for patients due to location, and improved patient flow with an increased bay count from 12 to 20. Additional amenities such as TVs in each bay offer patients a welcome distraction from treatment.
This upgraded unit has received glowing reviews from patients, providers and the RDU care team in the short time it has been open. Patients have praised the larger bays with TVs and privacy, while providers have been excited about new machines and the presence of windows that provide brightness in the space.
“The team experience is enhanced because we are all on one floor (previously it was split on two floors). There is plenty of storage space, and everything is new, clean and inviting,” Respess said.
By reinvesting back into the system, we are improving the quality of care for patients, and enhancing experiences for patients and team members. As we look toward our future as Vidant Health, the care and services provided, such as renal dialysis treatments, will have even greater impact for those we proudly serve.
GREENVILLE, N.C. (Nov. 12, 2021) – Today, East Carolina University’s Brody School of Medicine and Vidant Health took the first step in the final approval process in creating ECU Health with a goal of becoming a national academic model for providing rural health care.
ECU’s Board of Trustees approved a joint operating agreement between the Brody School of Medicine and Vidant Health that will enable the two organizations to more effectively and efficiently address current issues facing the region — such as health disparities and care delivery obstacles — while also better anticipating future health care and educational needs.
Under the joint operating agreement, the Brody School of Medicine and Vidant Health will retain their separate legal entities, but will function collaboratively under a new, shared brand launching in 2022, known as ECU Health. Most Vidant entities and ECU Physicians will operate under the new brand while the Brody School of Medicine’s name will not change.
“This agreement represents an important milestone in the long-standing affiliation between two entities bound by the same mission as we work toward the creation of ECU Health,” Chancellor Philip Rogers said. “It signals the point where we can begin to move forward together on our journey to launch a clinically integrated academic health system and deliver on the commitment to provide quality health care for all eastern North Carolinians.”
The agreement also requires approvals from the Vidant Health Board of Directors, ECU Health Medical Center Board of Trustees, the Pitt County Board of Commissioners, and the University of North Carolina Board of Governors. The UNC Board of Governors is expected to consider the agreement for final approval during its Nov. 17-18 meeting.
The majority of Vidant Health’s locations, ECU Health Physicians and ECU Physicians will rebrand to ECU Health. However, there are no changes to the employment status or benefits of current employees – and no assets are exchanged – as a result of the approval of the joint operating agreement.
ECU and Vidant Health announced their intentions to clinically integrate in June when Dr. Michael Waldrum, chief executive officer of Vidant Health and distinguished professor at the Brody School of Medicine, was appointed dean of the Brody School of Medicine. Waldrum continues to serve as CEO of Vidant Health in a dual role that is further outlined by the joint operating agreement.
“Today’s announcement is about the residents of eastern North Carolina and brings into reality the collective vision our two institutions have shared for nearly 50 years,” Waldrum said. “Rebranding Vidant to ECU Health in 2022 further signals and strengthens our commitment to bring the best research, doctors and care to the East. We have proven in recent years, and particularly during the pandemic, what can be accomplished when we focus our energies on the mission to improve the health of eastern North Carolina.”
The joint operating agreement is a legal framework that will allow the work of clinical integration and rebranding to begin in earnest with the purpose of:
- Improving the value of and the access to quality care and providing patients with a more streamlined health care experience.
- More efficiently using clinical staff across the combined operations, regardless of which organization employs them.
- Helping to facilitate new strategies and interventions for the most prevalent health needs of eastern North Carolina.
- Creating operational efficiencies and reducing costs.
- Establishing a shared leadership and governance structure for ECU Health.
Under the terms of the agreement, which will be effective Jan. 1, 2022, the two organizations will work together to:
- Evaluate and modify existing practices to improve quality and coordination of care.
- Integrate certain management structures and strategic planning efforts.
- Develop a plan for shared services to support the integrated entity.
- Leverage the capabilities of each organization to advance the collective research and education infrastructure.
- Coordinate philanthropic initiatives.
“Our mission has not and will not change. How we execute the mission is what is at issue,” said Dr. Jason Higginson, executive dean of the Brody School of Medicine. “We are going to be looking at areas where efficiencies can be built into our process and where value can be added to what we’re doing to improve the final outcome. So rest assured, what Brody is here for and what it stands for is not changing.”
Waldrum noted that the Brody School of Medicine has a rich history of training physicians for North Carolina and that mission will continue as ECU Health serves the 1.4 million residents of eastern North Carolina.
“Through harmonizing our operations wherever possible and building on our unique expertise in caring for rural and underserved communities, ECU Health will set the standard and be a national model for rural health care delivery,” Waldrum said.
About Vidant Health
Vidant Health is a mission-driven, 1,708-bed academic health system serving a region of more than 1.4 million people in 29 eastern North Carolina counties. The not-for-profit system is made up of more than 13,000 team members, nine hospitals including an academic medical center, home health, hospice, wellness centers, and ECU Health Physicians, a multi-specialty physician and provider group with more than 500 providers in more than 100 practice sites in eastern North Carolina. Vidant is affiliated with The Brody School of Medicine at East Carolina University. As the largest employer in the East and a major resource for health services and education, Vidant’s mission is to improve the health and well-being of eastern North Carolina. For more information, visit VidantHealth.com.
About East Carolina University
East Carolina University, or ECU as it’s best known, offers 87 bachelor’s, 68 master’s and 18 doctoral degrees to 28,000 students on its Greenville, North Carolina, campus and through an acclaimed online learning program. ECU also boasts the largest business school enrollment and largest number of new nurses and education professionals produced by a four-year North Carolina university, in addition to the largest studio art program in the state. Located near Atlantic coast harbors where pirates once roamed, ECU adopted the “Pirates” mascot in 1934 for its athletics program and competes in NCAA Division 1. Visit: www.ecu.edu.
The Brody School of Medicine at East Carolina University was founded more than 40 years ago to increase the supply of primary care physicians serving North Carolina, improve the health status of eastern North Carolina and enhance access of minority and disadvantaged students to a medical education. Each year, the school graduates close to 86 medical students and welcomes about 125 residents and fellows. Brody consistently ranks No. 1 in North Carolina – and in the top 10% nationally – for graduating physicians who practice in-state, practice primary care and practice in rural and underserved areas. It also ranks in the top 10% nationally for graduating Black and Native American physicians.
Over the last seven years, Vidant Medical Center (VMC) has partnered with organizations across eastern North Carolina to host Project SEARCH for exceptional Pitt County students.
Project SEARCH is an international transition program that provides real life work experiences to high school graduates with intellectual and developmental disabilities. The one-year program helps students learn various marketable skills that can help them gain employment after graduation from the program.
Lisa Lassiter, director of workforce development at Vidant Health, said Pitt County Schools approached Vidant about the possibility of partnering in the program. She took the lead on the Vidant side and attended meetings, worked with community partners and, with support and approval from senior leaders at the hospital, had a classroom for these students created at VMC.

Lassiter said she is grateful for the program, the students, community partners and everyone involved.
“I think this program and these kids have taught me more than I have ever been able to expose to each of them,” Lassiter said. “I was very limited in what I knew about exceptional children when the program began and they have opened my eyes and amazed me many times.”
Seven years in, the 2021-22 Project SEARCH class is the largest to date with nine students. These students spend time in the classroom learning employable skills and go out to internship sites throughout different departments at VMC to practice and refine these skills.
A Shining Example
 For students that have an internship experience at the VMC cafeteria, they get a chance to work with a program graduate.
For students that have an internship experience at the VMC cafeteria, they get a chance to work with a program graduate.
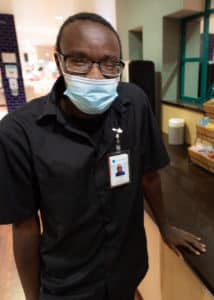
David Jenkins is a utility worker and is a direct supervisor for the Project SEARCH interns placed in the main cafeteria. Jenkins graduated from the program in 2019 and said he loves helping those going through their internships.
“I enjoy that a lot. I get to teach them about stuff that I know and I can sit back and watch them grow because of things that they learn from me,” Jenkins said. “Hopefully that will help them be a better citizen in this community.”
Jenkins had opportunities to intern in different areas throughout VMC during his year with Project SEARCH but enjoyed working in the cafeteria most. He said he felt a breakthrough when he asked to join team meetings during his internship and learned a lot about team goals.
He said it was important for him to go through the program and learn the important skills that have set him up for success today.
“My favorite part of going through the program was pretty much experiencing stuff that would be like the real world, such as advocating for myself, learning how to manage money, working with other people and how to interact with other people,” Jenkins said.
Katie Nagler Houmard, Project SEARCH instructor, said she was proud to see Jenkins’ growth from his time as a shy student to the leader he is today. She also said it’s important for current students to see what they can accomplish with Jenkins setting the example.
“We’ve seen that when they hear it from someone who has been where they are, they’re much more likely to really grasp it and take the advice,” Houmard said. “Sometimes when we tell them something, they could think, ‘What do you know? You’ve never been in my shoes.’ I think it’s inspiring for our current students to see him now in his role and working as part of the team at Vidant. It definitely gives them a good goal to work toward.”
Quintequa Weaver, Project SEARCH job coach, agrees. “I think just seeing him be a role model to the kids now is such a great thing to see,” she said.
It Takes a Village
Lassiter said community partnerships are an important part of what makes the program so special. While VMC hosts the classroom and offers the locations for internships, other community organizations contribute so much.
Pitt County Schools provide a teacher and identify students who make great candidates. RHA Health Services offers up a job coach to help students learn skills and work with them to find positions after graduation. On a state level, the North Carolina Council on Developmental Disabilities and North Carolina Vocational Rehabilitation provide support as well.
Internally to Vidant, team members who support the program are invaluable. Bernard Dixon, assistant manager for Central Services at VMC, is one of many team members who supports Project SEARCH and students going through the program. He said he appreciates the opportunity to work with these exceptional students and help them grow as team members.
When a student is preparing for an internship, they go through the typical steps that any team member would take before joining a department.
“They come down and they interview for the position as a typical employee would and we sit down and talk with them,” Dixon said. “Once we sit down and talk, we find out what exactly they can do and what their skill level is. Once we determine what their skill level is, we treat them just like we would any other employee.”
He has found that as he works with the students in Project SEARCH, once they are comfortable in their role, they often exceed expectations. He said supporting the students—and not putting labels or limitations on them while also helping them learn employable skills—is the most important thing his team can do.
“We don’t want them to be labeled or anything like that,” Dixon said. “It’s not about saying they can’t do this or they can’t do that – no. Let them do what they do. We find out that a lot of them can do more than we think they can.”
Learn more
- For more information on Project SEARCH, contact Lisa Lassiter via email at [email protected]
- Vidant Health News: Project SEARCH
- Project Search at ECU Health Medical Center 2021 Graduates
Burnout in health care providers is not a new concept but ideas and theories of how to avoid it are developing in unique ways.
Dr. Stephen Trzeciak served as the featured lecturer for the 13th annual José G. Albernaz Golden Apple Distinguished Lecture presented by ECU Medical & Health Sciences Foundation and Vidant Health. Dr. Trzeciak, chief of medicine at Cooper University Health Care and professor and chair of medicine at Cooper Medical School of Rowan University in Camden, New Jersey, discussed compassion and the importance of meaningful connections in health care and everyday life.

A few years ago, Dr. Trzeciak was facing burnout as a health care provider and knew something needed to change.
As a person who loves research, he began to dig into related literature and studies that focused on combating burnout in providers. In medical school, he said, he was taught that caring too much and having too much compassion could cause a provider burnout more quickly. What he found in studies, however, painted a different picture.
“What the literature shows is that there is an association with compassion and burnout – but it’s inverse. If there’s high compassion, there’s low burnout. Why? Well, we don’t know for sure but I have my hypothesis,” Dr. Trzeciak said. “Because when you connect with people through compassion, and have a relationship that flows from that, you get the fulfilling part. If you don’t have that then all you have is a really stressful job.”
Key to Resilience is Relationships

He tested his hypothesis on himself, as a study subject of one and found that when he leaned into caring more rather than detaching, his feelings of burnout began to lift. It wasn’t just about connecting with and showing compassion to patients and families, but to everyone he worked with and interacted with—professionally and personally. He believes this method can work not only within health care but in every walk of life.
He challenged everyone who is feeling the effects of burnout to give his method a chance, not just because it has worked for him and helped change his life, but because it is backed by science.
He highlighted a Harvard University study that tracked students at the university and Boston-area teenagers throughout their lives and found the best predictor of good health and well-being into your 80’s is your midlife quality of relationships. Dr. Trzeciak said this and many other studies show that the key to resilience is relationships.
“That’s why it is vitally important in our health systems, in our medical schools, everywhere – at the shopping mall, at the grocery store – that we take good care of each other,” Dr. Trzeciak said. “You don’t have to be a health care provider to feel burnout, especially in 2021.”
Compassion in Health Care
Compassionate and caring environments not only help team members face less burnout, but also help patients see better outcomes.
During his lecture, Dr. Trzeciak discussed many studies pointing to positive results for patients whose health care providers show compassion in various ways. He said that he does not have any magical thinking about compassion and that the top determinant of clinical outcome is still clinical excellence.
However, he said no patient and no provider should have to choose between clinical excellence and compassionate care. It’s not an either-or choice, but a both-and.
In eastern North Carolina
 Dr. Michael Waldrum, chief executive officer of Vidant and dean of the Brody School of Medicine, said it was no mistake that Vidant chose compassion as one of its core values six years ago—a thoughtful selection rooted in understanding what behaviors help patients, the communities Vidant serves and team members.
Dr. Michael Waldrum, chief executive officer of Vidant and dean of the Brody School of Medicine, said it was no mistake that Vidant chose compassion as one of its core values six years ago—a thoughtful selection rooted in understanding what behaviors help patients, the communities Vidant serves and team members.
“As I think about that time and the now the world we live in today, with the most profound social and health care disruptions, with more Americans that died in any event in over 102 years… at no time is compassion more important than right now,” Dr. Waldrum said. “That is a really hard thing to deal with, those realities. The great thing is that we know we have solutions to the challenges we face and compassion is one of those solutions.”
Typically, the José G. Albernaz Golden Apple Distinguished Lecture is set for the first day of class for first-year Brody School of Medicine students. However, due to the COVID-19 pandemic, the event was held for a smaller audience with a few representatives from the first-year Brody class.
Dr. Waldrum said during the event that he recently had dinner with a group of first-year Brody students who discussed the need to bring greater compassion to health care.
“It was so impactful to me because I left that meeting last night and I’m just so proud to be in eastern North Carolina and having that dialogue and making compassion cool,” Dr. Waldrum said. “Because I think that’s what it takes. It takes intention in talking about it, understanding it and knowing we’ll never be perfect, but we’re all on this journey.”
COVID-19 continues to evolve and expand its grip across the country and here in eastern North Carolina.
“This is one of the most diabolical viruses I’ve ever seen,” said Dr. Paul Bolin, chief of Adult Medical Services at ECU Health Medical Center, and the chair of the Department of Medicine at Brody School of Medicine at East Carolina University.
“We were in a good place. Transmission had slowed down, more and more people were getting vaccinated and protected, hospitalization days started to really come down, number of cases started to come down – and many of us thought we were in the last leg of this marathon,” said Dr. Niti Armistead, chief medical officer for Vidant Health. “What changed was the vaccination rates just hit a wall.”
“In North Carolina, in the past three to four weeks, we have seen a tripling in the number of cases, and in the number of hospitalizations,” said Dr. Bolin. “We’re seeing the same things as we did last fall and winter, but it’s in a much younger and much healthier population.”
Another difference now – we have a vaccine.
“It’s like wearing your seatbelt – your chances of being in an automobile accident are very low, but your chances of surviving that with a seatbelt are much greater,” said Dr. Bolin. “Your chance of surviving COVID are 25 fold better with the vaccine than without it.”
Even still – roughly half of the country remains unvaccinated, enabling the virus to mutate and variants to cause an increase in infections and complications.
“The virus didn’t slow down just because our vaccination rates dropped,” said Dr. Armistead.
Experts say most concerns about the vaccine don’t outweigh the risk of being unprotected.
“I think the most important thing to understand is this: there have been some very small number of complications from the vaccine. And that is a one-time event that occurs after the vaccination,” said Dr. Bolin. “Your risk of dying from COVID if you’re not vaccinated continues day after day after day after day, until this pandemic is over with.”
Vidant Health has appointments available for anyone eligible to receive the vaccine. Visit www.VidantHealth.com/vaccinate and schedule yours today.