ECU Health nurses from every area of expertise across the health system gathered on June 20 at the East Carolina Heart Institute for the 10th annual ECU Health Nursing Summit where they shared best practices and innovations that will help chart the future of nursing in eastern North Carolina.
Titled “Connecting with: Minds, Hearts and Purpose,” nursing leaders at ECU Health designed the summit to acknowledge what nurses have experienced over the last three years, including what the COVID pandemic taught them as professional nurses, what they have lost and what it will take to move nursing forward together, according to Trish Baise, ECU Health chief nursing executive.
“With the ever-changing health care environment, it is important for ECU Health nurses to hear from state and national colleagues,” said Baise. “We are proud to welcome experts who are making a positive difference in the field by advocating and influencing policy, as well as nurturing innovations that address the workforce, the nurse practice environment and the health and wellness of nurses.”

In total, more than 178 nurses attended the summit, which was held face-to-face for the first time since 2019. Topics included policy advocacy, building positive environments, communicating across generations, self-care and wellness. The summit featured presenters from both ECU Health team members and experts from other areas, including North Carolina State Senator Gale Adcock and keynote speaker Katie Boston-Leary, director of nursing programs for the American Nurses Association.
“The Nursing Summit gave me ideas, things to research and refreshed my mind to help navigate this different health care world that we live in,” said Paula Bush, MIU manager at ECU Health Edgecombe Hospital.
The summit also served as an opportunity for ECU Health nurses across various levels of expertise and experience to connect directly with health system leadership, fostering a sense of community among health system nurses.
“Sharing best practices from both within and outside the health system helps spark a culture of innovation within nursing,” said Daphne Brewington, ECU Health system vice president of nursing excellence. “When we harness the expertise of our nurses, we can lead improvements and create environments where nurses thrive here at ECU Health.”
The Maynard Children’s Hospital at ECU Health Medical Center is celebrating its 10th year of offering high-quality, compassionate care in a soothing environment for patients and families in eastern North Carolina.
Dr. Matthew Ledoux, pediatrician in chief at Maynard Children’s Hospital, said the children’s hospital has immensely benefited the youngest patients in the East and made for more seamless care.
“The children’s hospital itself has given us the opportunity to grow services – we started an ECMO program, we’ve started and developed a dedicated Children’s Transport Team that flies all over the region and picks up kids and brings them back here,” Dr. Ledoux said. “The fact that we have all the subspecialty care, we have all the surgical care and generalized pediatric care here makes all the difference. It’s really a shining light in the East.”

Over the past 10 years, countless improvements have been made that have positively impacted the lives of many children and their families in eastern North Carolina. Other key expansions included the Pediatric Day Medical Unit, Pediatric Radiology Unit, and Pediatric Pharmacy among several other additions.
 Kim Crickmore, PhD, RN, senior vice president for Women’s and Children’s Hospital and Community Health Programs, said the Maynard Children’s Hospital is an integral part of health care in eastern North Carolina today. Over the last 10 years, the children’s hospital has delivered more than 37,000 babies, with more 61,000 inpatient admissions, 216,000 emergency cases, 223,000 outpatient cases and an additional 700,000 pediatric outpatient visits through the ECU pediatric outpatient center.
Kim Crickmore, PhD, RN, senior vice president for Women’s and Children’s Hospital and Community Health Programs, said the Maynard Children’s Hospital is an integral part of health care in eastern North Carolina today. Over the last 10 years, the children’s hospital has delivered more than 37,000 babies, with more 61,000 inpatient admissions, 216,000 emergency cases, 223,000 outpatient cases and an additional 700,000 pediatric outpatient visits through the ECU pediatric outpatient center.
“When we consider the impact to the region over the last 10 years, it’s really unbelievable,” Crickmore said. “It means so much to us here at the hospital that we’ve been able to provide care, primarily under one roof and unite all the services and to be the destination in eastern North Carolina for children who are sick or injured and need the specialty care we provide.”
Crickmore and Dr. Ledoux both said one of the services they are most proud of is the Children’s Transport team. The team consists of intensive-care trained nurses and respiratory therapists skilled in providing the specialty care many children need from the onset of transport to arrival at Maynard Children’s Hospital. Crickmore said it has been an intentional focus to build the program over the last five years and the program has seen many successes.
The Space
The amenities offered in the under-the-sea-themed Maynard Children’s Hospital are designed with patients and families in mind. Soothing young patients in a health care setting is no small task, but the children’s hospital is uniquely equipped to handle the challenge.
Dr. Ledoux said the community has stepped up time and again to provide resources and make donations that make a real difference for patients and families.
When thinking about his favorite area of the Maynard Children’s Hospital, Dr. Ledoux came back to the light tower, which can be seen when driving past the hospital. He said it’s a reminder of why he, and every children’s hospital team member, shows up to work every morning – to take care of the youngest patients in eastern North Carolina. He said he’s often asked what the colors on the light tower mean when people drive by at night.
“The reason is, we’re generally celebrating a child, we’re celebrating the end of a treatment, they’ve finished chemotherapy, or maybe they’ve been in the NICU for two or three months and they’re getting to go home,” Dr. Ledoux said. “We really try to make sure that the families and children get to pick the color and the time, but any time you see the color change anything different from our usual light blue, we’re celebrating a child and a family so it’s pretty exciting.”

Into the Future
Crickmore and Dr. Ledoux both said the next 10 years are something they’re looking forward to with the Maynard Children’s Hospital. They hope to continue expanding services and looking more to the region to bring specialty care closer to home for patients and families.
Dr. Ledoux said he and other physicians in the system have enjoyed their time spent in the region and the ability to help patients and bring key services closer to home for patients makes it special.
“I think the biggest thing is the distance that people have to travel,” Dr. Ledoux said. “We know that it’s a very underserved population and there’s a lot of poverty. People have challenges paying for gas or even having a car. The closer we can be to them to provide those services, the better.”
Another upcoming project that will impact pediatric patients in the East is the behavioral health hospital, slated to open in Greenville in 2025. ECU Health is partnering with Acadia Healthcare to build the state-of-the-art facility that will feature 24 inpatient beds specifically for children and adolescents with mental health needs. These beds will be the first of their kind in ECU Health’s 29-county service area and the only child and adolescent beds within 75 miles of Greenville, North Carolina.
Join us in celebrating the Maynard Children’s Hospital and all of its team members for the last 10 years of service to eastern North Carolina.
“I was really apprehensive about it because I’ve always been at one little hospital,” said Suzanne Foster, a travel nurse with ECU Health, “so it was a little intimidating coming to a larger hospital.”
Suzanne Foster isn’t the only nurse who found herself looking for new and different opportunities in the wake of the COVID-19 pandemic.
“I wanted to try travel, nursing and experience other facilities,” said Foster, “but I have a husband and a son that I dearly love and do not want to be away from. The fact that I can drive home at night is huge.”
She can do both thanks to the ECU Health Travel Staffing program. It’s an innovative approach to recruiting driven by the ever-changing health care industry and the need to meet nurses where they are.
“For an organization of our size to develop its own staffing agency is significant in the innovation of nursing care and staffing hospitals,” said Dennis Campbell, ECU Health Beaufort Hospital, a campus of ECU Health Medical Center interim president. “It’s no secret that there is a nationwide shortage of staff nurses and nurses are more mobile today than they have ever been.”
“I was getting a little bit burnt out in my current role, which frankly after COVID, I think a lot of us needed just a change of scenery,” Foster said.
“The travel staffing program mimics any other staffing agency. The difference is it’s ours,” said Campbell.
Since the start of the program, the system has hired more than 500 clinical team members. Of those, 89% have opted to extend their assignments.
“The team, everybody that you encounter is extremely considerate and thankful to have you on board,” Foster said. “Working at ECU Health has been wonderful.”
To learn more about the ECU Health Travel Staffing Program visit: https://careers.ecuhealth.org/pages/vidant-health-travel-staffing-program.
At ECU Health, the support team members provide to each other makes a difference – not only to those team members but also to the patients we serve across eastern North Carolina.
Recently, three ECU Health nurses were inducted into the East Carolina University (ECU) College of Nursing Hall of Fame while another earned a scholarship as she pursues her doctorate in nursing. These four ECU Health nurses each said the support of fellow nurses has uplifted them throughout their careers and the scholarship and inductions into the Hall of Fame is a reflection of that support.
Learn more about the honorees below.
Amy Campbell
Amy Campbell, quality nurse specialist at ECU Health, has been with the system for about 18 years over two separate stops.

 Campbell started at ECU Health Medical Center as an associate degree nurse in pediatrics and said she was quickly encouraged and supported by fellow nurses and leaders to join the HomeGrown program, which helps team members go back to school and balance their work and school responsibilities, and she received her bachelor’s degree from ECU in 2001. Campbell left ECU Health to teach at Pitt Community College and ultimately returned to the health system with a master’s degree. During her second stop at ECU Health, she said she was once again supported to further her education and pursue a doctorate degree, which she completed in 2020.
Campbell started at ECU Health Medical Center as an associate degree nurse in pediatrics and said she was quickly encouraged and supported by fellow nurses and leaders to join the HomeGrown program, which helps team members go back to school and balance their work and school responsibilities, and she received her bachelor’s degree from ECU in 2001. Campbell left ECU Health to teach at Pitt Community College and ultimately returned to the health system with a master’s degree. During her second stop at ECU Health, she said she was once again supported to further her education and pursue a doctorate degree, which she completed in 2020.
“A lot of executives were so encouraging for me to get my Ph.D. and I was HomeGrown and I was able to do my research here so they really were supportive all along,” Campbell said. “I also went through the Ph.D. program with a lot of my colleagues here so that was really great, too. I couldn’t have done it if people hadn’t given me time to do my research and to go to school.”
Campbell is a Williamston native and she said the rural aspect of the care ECU Health provides for the region is close to her heart.
The close-knit communities of eastern North Carolina transfer over to the hospital setting where Campbell said it’s a family atmosphere for team members and the patients they serve.
“I believe that at ECU Health we really do rise by lifting others and people really try to make sure others get time in the spotlight, even though, if you ask any of the four of us, we really don’t like this spotlight,” Campbell said. “But for me, I’m able to embrace it because I want all those people who supported me to have their moment with me. I’m a single mom, I’ve been a single mom for 19 years, but I’ve had a wonderful family here. Everyone has always been so good and supportive of school or whatever I was going through to help me be successful.”
Angela Still
 Angela Still, senior administrator of Women’s Services at ECU Health Medical Center, said she was humbled to join her colleagues who have been inducted into the ECU College of Nursing Hall of Fame as part of the Class of 2023.
Angela Still, senior administrator of Women’s Services at ECU Health Medical Center, said she was humbled to join her colleagues who have been inducted into the ECU College of Nursing Hall of Fame as part of the Class of 2023.
Still has been with the health system for 36 years and is a 1986 graduate of ECU. As a Greenville native, Still said the opportunity to care for and support women in eastern North Carolina is special to her.
“The needs of the patients and families in our region, the disparities, and the social determinants of health are so different from what the rest of the state deals with every day,” Still said. “Our 29 counties are comparable to the size of some states but it’s rural. Access to care, access to healthy food, these are unique needs. At this point in my career I am not impacting the individual patient and family, I’m working to impact the region. It’s a population of mothers and babies that we want to be healthier because they are our future in the region.”
Still said that during her time at ECU Health, she’s been the beneficiary of great leadership and mentors and she’s been happy to give that back to the next generation of nurses as they rise through the system and across the state.
She said it’s crucial to invest time and energy into mentorship as it will make a difference for the individual, those they mentor in the future and the patients they serve.
“The opportunity to mentor people through my career has been just really amazing. I have people across the state I mentored that are not with the system anymore and they still call me to ask questions or just look for guidance,” Still said. “So just being able to make an impact on the people that are going to care for others is very special to me. We’re all eventually going to retire, so being able to mentor and guide folks that are going to be here long after I’ve left and are going to continue to carry that torch and make a difference for our communities, it’s a big deal.”
Georgia Perry
 Georgia Perry is the nurse manager on 2 North Medicine and 2 North Progressive Care at ECU Health Medical Center and was also inducted into the ECU College of Nursing Hall of Fame this year.
Georgia Perry is the nurse manager on 2 North Medicine and 2 North Progressive Care at ECU Health Medical Center and was also inducted into the ECU College of Nursing Hall of Fame this year.
Perry said the night of the induction into the Hall of Fame was special for her as she had a chance to look into the crowd gathered and see mentors, some of whom nominated Perry for the recognition.
Perry earned her bachelor’s degree from ECU in 2010 and began working at ECU Health as part of the very first New Grad Nurse Residency Program class. She started working on 2 South, became an assistant nurse manager, and eventually became the nurse manager on her current unit. She received her master’s degree in 2015 and said the backing of fellow nurses and leaders alike made going back to school a manageable task.
“I tell people all the time, if you can dream it, you can do it here,” Perry said. “I truly feel like the support system is really what makes it easy to go back to school to be able to juggle it all. There’s a wealth of mentors here, you can pick up the phone and call anybody and it doesn’t matter if it’s across service lines.”
Perry is a Newton Grove native and said working in rural medicine is important to her because she grew up in a rural area.
“I think it’s wonderful that we have such great access to really all specialties right down the road,” Perry said. “My family actually will travel and get to ECU Health Duplin Hospital and then have access to the tertiary center, so we live it. I’m really grateful for what we have here at ECU Health and I’m glad to be a piece of the impact we have on this region.”
She added that the team around her keeps her going while the patients they serve inspire her to bring her best each day.
Lauren Nichols
 Inductees into the Hall of Fame help fund a scholarship for ECU College of Nursing students. Lauren Nichols, a staff nurse on the Cardiac Intermediate Unit at ECU Health Medical Center, earned a scholarship from the fund for this year.
Inductees into the Hall of Fame help fund a scholarship for ECU College of Nursing students. Lauren Nichols, a staff nurse on the Cardiac Intermediate Unit at ECU Health Medical Center, earned a scholarship from the fund for this year.
Nichols, who has been working at ECU Health for seven years, is pursuing a doctorate in nursing with a family nurse practitioner specialty at ECU.
Nichols is from Edgecombe County and said she chose to work at ECU Health and continue her education at ECU because of the health system’s commitment to rural health care and eastern North Carolina.
“ECU Health’s mission really resonates with me,” Nichols said. “Growing up in such a rural community makes me want to do my part to help improve the health of the people of eastern North Carolina.”
She said she never doubted her decision to go back to school because of the support she has received, especially from nursing leadership.
Join the Team
ECU Health nurses make an incredible impact every day across eastern North Carolina. Learn more about opportunities to work alongside these amazing nurses and so many others here.
When Lauren Moore, a fourth-year student at the Brody School of Medicine at East Carolina University, begins her residency training at ECU Health Medical Center in July it will mark the beginning of a new chapter in her deeply personal family medicine journey. With a love for health care passed down from her parents, including her late mother, Moore’s next step is another toward her ultimate goal: making a difference in the lives of countless eastern North Carolina community members.
Moore’s experience with health care goes far beyond her medical school training. Her father is a physician’s assistant and she was naturally drawn to the connections he made in the community. Growing up in Farmville and attending school in Greenville, she recalls countless instances where he was stopped in places like the grocery store, catching up with a long-time patient or offering helpful advice.
“Growing up, people would come up to us and be like, ‘Mr. Eddie, how are you doing?’ I’d ask, ‘Dad, who is that?’ He’d say, ‘Oh, a patient that I’ve had for ten years now.’ I would think, ‘That is amazing,’” Moore said. “And even recently, ever since I’ve matched at ECU Health, just within the past few weeks, I’ve had several people from my Bible study at my church that have said, ‘You know, I’ve been needing to get a primary care doctor.’ And I’m like, ‘I’m your person!’ It just feels good that they trust me enough to one day be their doctor and to have those personal connections and be able to serve them to make sure their health is taken care of.”

She also experienced the health care profession from the patient perspective through her mother’s cancer journey. When Moore was seven years old, her mother was diagnosed with breast cancer for the first time and was declared cancer free after about a year of treatment.
Then, six years later, she was re-diagnosed with metastatic breast cancer, which spread to her liver and brain. Moore’s mother passed in June of 2010. She reflected on the care her mom received and how the care teams went above and beyond for patients and families alike. Moore learned what it meant to be a compassionate care giver and she said she’s prepared to bring that same compassion to her future patients.

“Seeing her go through that and seeing the way that her physicians were able to play such a vital role in not only her life, but also my family’s life and making sure that we were OK even after the fact,” Moore said. “If my dad was walking through the hospital, my mom’s physicians would check in on him and ask how he was doing and if he needed anything. So it wasn’t that they were just taking care of my mom as a patient, but they were also taking care of the rest of her life, too. That had such a tremendous impact on me. My goal is not only to care for my patients the same way my dad does, but also to make the families feel the same way that those physicians made me feel.”
Brody Matches
Moore is one of 77 Brody medical students poised to begin their residency at hospitals across the country, following an emotional Match Day ceremony in March and commencement in May. For Moore, who wants to practice family medicine in the region in which she grew up, matching to ECU Health Medical Center was always the goal.
“Being a medical student at Brody and seeing the patient population that we have here, I think that’s really what drew me to ECU Health,” said Moore. “The fact that it serves patients throughout the 29 counties in eastern North Carolina who otherwise wouldn’t have a primary care provider or a Level I trauma center if it wasn’t for us. I was drawn to the educational opportunities given the uniqueness of our patients and everybody in the residency program is just so welcoming and nice. I know it’s family medicine, but it is also like a family there.”

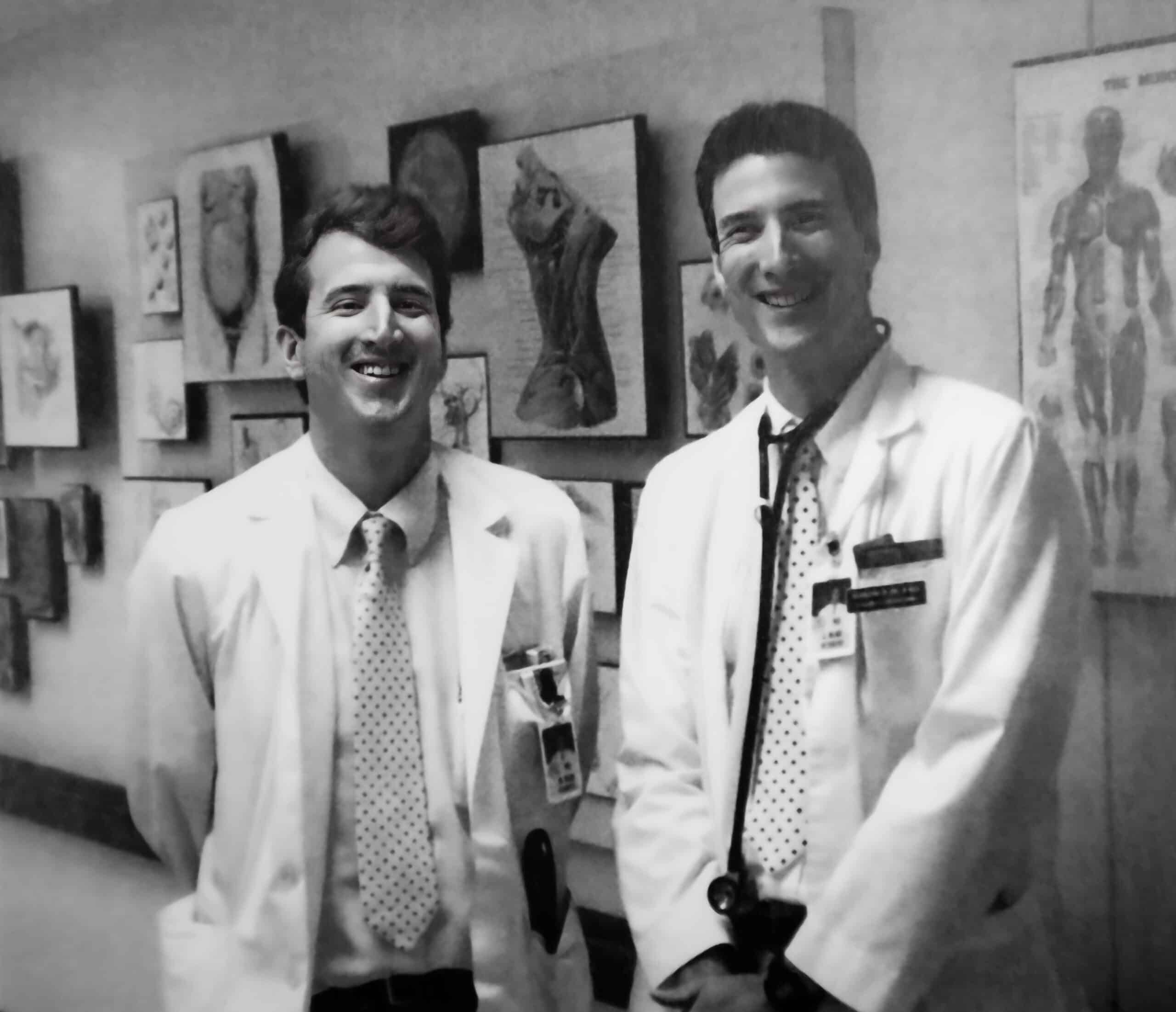
Photo Courtesy of ECU News Services
Match Day at Brody marked a milestone for the Class of 2023, whose medical school journey included the historic events of learning through the COVID-19 pandemic and the integration of Brody and then-Vidant Health, which became ECU Health in 2022.
Match Day is arguably the pinnacle of medical school, when students discover where they will train during their residency, surrounded by friends, family and Brody faculty and staff who have guided them over the years.
The Class of 2023 is a snapshot of Brody’s mission to serve the state. The 77 members of the graduating class represent more than 25 North Carolina counties, from Buncombe in the west to Pasquotank in the northeast.
ECU Health Medical Center had an excellent Match Day, according to Dr. Herb Garrison, associate dean for Graduate Medical Education, with 98 medical students matching into the 12 main residency programs. Twenty-six of the students, or 27%, will graduate from North Carolina medical schools, including 16 students from ECU’s Brody School of Medicine. Brody’s most recent class features the most medical students who will begin their residency at ECU Health Medical Center in July.
“We’re thrilled for this class to start their residencies across the country and we’re especially excited about how many will be staying with us at ECU Health Medical Center,” Dr. Garrison said. “This group had their first year of medical school disrupted by the start of COVID and I’m so proud of the way they supported each other through that experience. I’m just excited, as I am every year, to see these skilled and highly trained students start their careers and share everything they’ve learned here with the rest of the world.”
A Rural Legacy
Dr. Mott Blair’s journey to his post as a physician at ECU Health Family Medicine – Wallace is not totally unlike Moore’s. Dr. Blair’s father was a doctor in Duplin County beginning in 1949.
Dr. Blair shared that his father was a primary care physician who also took up obstetrics and did home deliveries for many families. Seeing his father’s connection with patients and families in his home town lead him directly to his own career in medicine.
He attended the Brody School of Medicine – then called ECU School of Medicine – and graduated in 1987, alongside his brother. He matched with ECU Health Medical Center – then called Pitt County Memorial Hospital – and began practicing in Wallace after his three-year residency. He said his decisions to attend Brody, make Greenville his first choice for residency, establish a practice in his rural hometown and eventually partner with the ECU Health system have all been rewarding for himself and beneficial for the patients he serves.
“I feel like the mission of the medical school was a mission that I wanted to take on and I think I’ve been successful in doing that,” Dr. Blair said. “I think the credit in being able to do that goes to the medical school and now the medical center as well. I really think that what we’re doing now, particularly as we support practices across the eastern region of the state, is a crucial thing to put in place, because health care in rural North Carolina is so difficult and we need to have true rural primary care.”
Dr. Blair said that he knows his time at Brody prepared him well for the challenges of residency and he has seen the same for other Brody graduates whom he’s connected with as residents.
For first year residents, he said it’s a new kind of challenge and learning curve, just like those experienced in the first year of medical school and the first year of rotations, but sticking to the same habits that got residents where they are will make all the difference.
“Work hard, study hard. Getting through residency the first year is a lot of hard work,” Dr. Blair said. “So enjoy it and it will go by fast and it will seem like a distant memory pretty quickly. Coming out of Brody, you’ll be well prepared. I found the preparation for me was excellent. You have to be patient with the pace in medicine. It changes rapidly and has really changed a lot since I’ve been in practice and continues to do so.”
In line with the Brody School of Medicine’s mission to increase the number of primary care physicians who serve North Carolina, 52% of the 2023 Brody class matched into primary care residencies — including obstetrics and gynecology — and 44% matched to residency programs in North Carolina.
Moore and Dr. Blair are just two examples of the importance of the Brody School of Medicine and ECU Health connection. Developing high-quality, compassionate physicians for a region in need helps meet the organizations’ combined mission to improve the health and well-being of eastern North Carolina.
“Developing great primary care providers for rural areas is at the core of what we do at Brody and within ECU Health” said Dr. Michael Waldrum, CEO of ECU Health and dean of Brody. “Working as rural health care professionals is hard but we’re working together to train doctors that will care for the whole patient, their physical and emotional health, and I think we’ve been successful in doing that. We have students, professors, residents and doctors that really understand that side of health care and their work in that space leaves a legacy that we can all be proud of.”
Greenville, N.C. – ECU Health is pleased to announce Dr. Richard Medford, MD, FAMIA, FRCP(C), as ECU Health’s first Chief Medical Informatics and Digital Health Officer (CMIDHO) following an extensive national search and interview process with stakeholders from across the organization. Dr. Medford officially joined the health system on May 1, 2023.
 “Over the past several years, we have seen the importance and value of telehealth and other technology in patient care, and we recognize the need to be nimble to work within the digital evolutions and innovations we are seeing in and around the health care industry,” said Dr. Michael Waldrum, ECU Health CEO and dean of the Brody School of Medicine at East Carolina University. “I am pleased to welcome Dr. Medford to ECU Health and feel strongly that his background in health care technology innovation will serve our patients and the region well. As we continue to define the future of ECU Health, Dr. Medford’s collaborative and evidence-based approach will be assets in helping us to realize our vision for those we proudly serve.”
“Over the past several years, we have seen the importance and value of telehealth and other technology in patient care, and we recognize the need to be nimble to work within the digital evolutions and innovations we are seeing in and around the health care industry,” said Dr. Michael Waldrum, ECU Health CEO and dean of the Brody School of Medicine at East Carolina University. “I am pleased to welcome Dr. Medford to ECU Health and feel strongly that his background in health care technology innovation will serve our patients and the region well. As we continue to define the future of ECU Health, Dr. Medford’s collaborative and evidence-based approach will be assets in helping us to realize our vision for those we proudly serve.”
In this newly-expanded role, Dr. Medford will collaborate with executive and clinical leaders to develop and execute strategies to optimize and transform care delivery models and the clinician-patient experience through the strategic use of the electronic health record (EHR), digital tools, advanced technologies, services and processes.
As part of his work at ECU Health, Dr. Medford will continue to practice medicine, allowing him to more fully understand and relate to the challenges and opportunities in the digital environments and frameworks our clinicians provide care within. He has also received a faculty appointment within the Brody School of Medicine with a continued focus on research where he will help serve as a bridge between the academic, medical, information systems and research arenas.
“I am grateful for the opportunity to join ECU Health and to collaborate with the teams here to bring innovations that improve the health status of the patients we proudly serve,” said Dr. Medford. “The unique challenges we face in this vast rural environment require unique, cutting-edge solutions. I look forward to serving on behalf of the people of eastern North Carolina.”
Originally from Toronto, Ontario, Canada, Dr. Medford received his MD from Jefferson Medical College in Philadelphia. He completed an internal medicine residency at Queens University in Kingston, Ontario, and fellowships in infectious diseases from the University of Ottawa and clinical informatics from Stanford University School of Medicine.
Dr. Medford is triple board certified and the recipient of numerous honors, awards and grants. He has proven to be a transformational and strategic leader who understands the importance of leveraging digital technologies and the EHR to drive health system success, enhance patient safety and quality, improve provider efficiency, decrease provider burnout and augment research endeavors.
For more than 25 years, the Pediatric Asthma Program at the Maynard Children’s Hospital at ECU Health Medical Center has worked to help patients and families living with asthma lead healthy lives.
Jeanine Sharpe, social work care manager for the Pediatric Asthma Program, said the goal of the program has always been to decrease emergency department visits, reduce school absences due to asthma, provide education and improve quality of life for patients and families.
“Currently, there are about 5.1 million children under the age of 18 that have asthma in the U.S. and it’s the leading chronic disease for children,” Sharpe said. “Just for our service area last year, we had 1,687 pediatric asthma patient referrals. It’s the number one reason for school absences and the number two reason for hospital admissions for children. But we know that asthma is a controllable disease. What we find is that a lot of times the missing piece is just education.”
Sharpe said the program has touched many families over the years, whether it’s just one interaction or years of working on a family’s case. One family that has seen the impact of the program recently is the Carr family.
Dalton Carr III was diagnosed with asthma three years ago and struggled with wheezing, coughing and attacks in the years since.

Dalton III’s mother, Shanika said she was scared when her son was first diagnosed and she wasn’t sure how to handle certain situations. This past December, Dalton had an incident and was seen in the emergency department for his asthma.
“That’s when I met Ms. Sharpe,” Shanika said. “I was confused at the time, but ever since I met Ms. Sharpe, it’s been easier to learn things. I was confused with the things different doctors were telling me and I really didn’t understand how serious it was.”
Dalton III’s father, Dalton Jr., said it has been a great experience working with Sharpe and the Pediatric Asthma Program team.
He said the education and support offered have helped their son be confident and join in the everyday activities of other children his age. While he used to struggle, today he does not wheeze, cough or have flare ups from his asthma. Dalton Jr. credited the work with the Pediatric Asthma Program for this turnaround.
“She got us in a good routine for him. Ever since we’ve gotten Dalton on a consistent routine, he hasn’t had any problems,” Dalton Jr. said. “It’s even to the point where he can tell us when he needs his pump. He might say, ‘Mom or dad, I need my pump’ or ‘I’m good.’ He plays football and he’s running and tackling and it’s a lot but with Ms. Sharpe being in our lives these last few months, it’s just helped a lot.”
Dalton Jr. encouraged families to reach out for help and to learn what might work best for their child’s asthma.
Malorie Whitaker, respiratory care manager at ECU Health Medical Center, said the program is designed to help patients from one to 18 years of age feel more comfortable while they manage their asthma and participate in normal childhood activities.
She also said the program is set up to meet children where they are and eliminate barriers to care.
“Sometimes they’ll come into our office to do different testing or do some education, but usually we meet them,” Whitaker said. “So we’ll get into the homes, we’ll go into the schools, into the clinic, wherever they are. Some of these kids that we see don’t have transportation or transportation is difficult for them, so that’s why we like to go into the school or into the homes to help them.”
To learn more, or to speak with someone close to you, visit the Pediatric Asthma page or call one of the ECU Health locations offering pediatric asthma services.
- ECU Health Bertie Hospital: 252-833-2861
- ECU Health Chowan Hospital: 252-833-2861
- ECU Health Edgecombe Hospital: 252-641-7382
- ECU Health Medical Center: 252-847-6835
- ECU Health Roanoke-Chowan Hospital: 252-209-3117
Wildwood Park in Greenville served as the perfect setting for “Emergency Medicine Wilderness Day” as ECU Health emergency medicine residents practiced assessing and treating a variety of common outdoor ailments including altitude sickness, lightning strikes, falls from trees and more.
On March 29, approximately 20 emergency medicine residents attended training and worked in small groups to run through simulated injury scenarios with real people. From knowing how to stabilize an injured person, to assessing injuries and helping get them to safety, emergency residents worked together to treat the injuries under the watchful eye of experienced faculty members from the Brody School of Medicine at East Carolina University. Residents received real-time instruction and feedback from faculty as they worked through their training.
Standardized patients from Brody’s Office of Clinical Skills Assessment and Education acted as the patients in each scenario. Standardized patients are trained to mimic real patients so that students can learn. Their role is to help prepare future health care professionals for a variety of patient interfaces.

“There are a number of practical applications for this type of training, especially for our medical residents who get to test their knowledge in the field,” said Dr. Jennifer Bennett, an emergency medicine physician at ECU Health and clinical assistant professor of emergency medicine at Brody. “These scenarios are the types of things that we, as emergency medicine physicians, address somewhat commonly. We can apply the knowledge and skills learned out here to patient care.”
The day was a success, according to Dr. Bennett, who helped create the simulation Emergency Medicine Wilderness Day training event last year alongside Dr. Jennifer Parker-Cote, assistant professor of emergency medicine at Brody. Both doctors helped organize the Wilderness Day, coming up with unique patient scenarios, including the altitude sickness training station which featured a standardized patient acting as a distressed hiker. The residents removed a fake snake from the area, asked the patient questions about their medications and medical history, moved the patient to a lower area and helped get them to further medical care.
“It’s always nice to get outdoors instead of sitting in a lecture hall,” said emergency medicine resident Tyler Ruchti, DO. “When you’re in the hospital, you have all of your tools and all of your equipment and know where it is, and when we come out here and do things like this it’s a change of scenery. You have to think outside the box.”
The training is another example of the valued partnership between ECU Health and Brody. Residents at an academic health system like ECU Health have support and resources for continued education from faculty and the Interprofessional Clinical Simulation Program at Brody, enriching their clinical training experience. Residents are able to participate in trainings like this to prepare for real situations with real patients both behind the walls of the hospital and out in the community.
“This training was partially about simulating complex medical issues that you may encounter in the wilderness as well as providing a little wellness for our residents,” said Dr. Parker-Cote. “This is a fun way to test knowledge and work together as a team. When it comes to education, there are different modalities for teaching. Learning in this type of environment provides us another way of reinforcing the knowledge they have learned throughout their residency, and it prepares them to help their fellow community members no matter the situation.”
Resources

Patient-centered care is a term often used in health care to describe a collaborative relationship between care teams, patients and families. It is the goal of many health care providers, the type of relationship that occurs only when trust is fully developed.
For medical students learning the trade, there are right and wrong answers to most of the questions they encounter. These symptoms match that disorder, or this medication cannot be given to that type of patient. While there is much to learn about the science of medicine from the pages of a textbook or within the walls of the classroom, it is hard to replicate the hands-on experience gained during direct patient care. Often times, the best lessons come from long days and nights spent compassionately caring for patients, listening to feedback, patiently answering questions and validating the feelings of those they care for.
“It’s one of those things that you’re taught in medical school to listen to patients and their families because it really is shared decision making,” said third-year Brody School of Medicine at East Carolina University student Jennifer McMains. “But then when you get in the moment, there’s so much going on and it’s very easy to think that you know medically what’s best. But that’s not the way we practice medicine. If the family feels strongly, then listen because they’re with their loved one every single day, every minute.”
McMains learned firsthand the importance of patient-centered care when she met Carnie and Melody Hedgepeth in June 2022 during one of the most difficult periods of their lives.
Carnie, who serves as the director of emergency services for Beaufort County and as a pastor at Arthur Christian Church, was out for a summer ride on his motorcycle when he was involved in a serious accident. He was hit by an oncoming driver and thrown from his bike, eventually landing on the roof of the car. Despite wearing a helmet, the accident left him with multiple facial injuries and a brain bleed that resulted in a traumatic brain injury. With Melody by his side, Carnie spent more than a month in ECU Health Medical Center where they quickly found an expansive support system.
“A lot of people in the (emergency room) know him and people surrounded us with love and prayers,” said Melody. “We got through that first night thanks to everyone in the ER.”
It was in the ER during her surgery rotation where McMains would first meet the Hedgepeths.
“We would go in as a team of doctors to check and provide updates on the plan,” McMains recalled. “Melody was constantly asking ‘Can we be doing anything more?’ or ‘Are there better ways for us to position his feet?’ Things like that seem small but she was always looking at the six-months, one-year outcome and always believing that he would recover. That showed me a lot because I would go into the next person’s room and there wouldn’t be a person to advocate.”
For the Hedgepeths, the attention and care they received left a lasting impression.
“From my standpoint, that’s the most important thing, knowing that the person who is calling the shots cares,” said Carnie. “It means so much when you know that the person cares.”
Carnie, Melody and McMains were reunited April 6 at the Hilton in Greenville during the Legacy Teachers Celebration, a tradition presented by Brody and ECU Health that gives students a chance to honor a patient they met during third-year rotations who taught lessons about care, compassion and communication they will take with them into their careers as physicians.

In total, 20 third-year medical students shared their stories at the luncheon, which featured gift baskets, a photo station and remarks from ECU Health and Brody leaders. At the end, legacy teachers placed custom pins on the students’ white coats to commemorate the significance of the occasion and serve as a reminder of the lessons learned – lessons that they will carry with them through their medical careers.
“As physicians, these stories fuel our hearts and purpose for servant leadership in our pursuit of medicine,” said Dr. Christina Bowen, ECU Health chief well-being officer. “The connections we make with patients help us learn the art of practicing medicine. We’re here to honor these sacred relationships and celebrate our legacy teachers.”
Third-year Brody student Karen Semaan shared her experience with former patient Aidan Mummert and his grandparents. Semaan got to know them well while on the pediatric hematology-oncology rotation. At first, the care team was unsure of the cause of Mummert’s illness. They visited Mummert and his family often to ask more questions and run more tests. Despite the uncertainty, the family and care team developed a light-hearted and fun relationship. When doctors finally determined the cause of the infection, the care team celebrated with joy alongside the family during Mummert’s discharge.
Semaan said the relationship she developed with Mummert and his family was a reminder of her “why” as a future physician.
“Talking with Aidan and his grandmother reminded me, even though medicine and medical school is hard, even though you’re tired and your emotional reserves are low, you can get energy from people,” Semaan said. “You can get love and compassion from them that you can then give back and share with other patients that you see that day.”
The Legacy Teachers Celebration is an important partnership between ECU Health and Brody. The education that medical students receive at Brody, combined with the experiences gained within the ECU Health clinical setting, provides a full spectrum of knowledge that prepares them to deliver compassionate care to the patients they will serve.
“Today is one of the greatest days because we get to celebrate the relationship between our student doctors and their patients,” said Dr. Amanda Higginson, associate dean for student affairs at Brody. “Together, Brody and ECU Health have a shared responsibility to provide both healing and learning. Our legacy teachers help us do that in ways that go beyond just the classroom setting.”
Dr. David Eldridge, senior associate dean for academic affairs at Brody and Brian Floyd, chief operating office at ECU Health and president of ECU Health Medical Center, provided remarks at the event. Like the students, they shared their deeply personal stories of important lessons they learned as students. The speakers shared common themes, especially around the importance of positive, trusting relationships between patients and care teams.
“All across health care, and especially here at ECU Health, there incredible people gathered around others who are in-need of care,” said Floyd. “We’ve chosen this work because it is so meaningful. We are able to make a difference in the lives of so many because of the beautiful relationship between these students and these patients. Today is a reminder of why we do what we do.”
In a ceremony laced with excitement, anticipation and tradition, fourth-year medical students in the Brody School of Medicine at East Carolina University learned where they will spend the next three to seven years completing residency training.
The March 17 event marked a milestone for the Class of 2023, whose medical school journey included the historic events of learning through the COVID-19 pandemic and the integration of Brody and then-Vidant Health, which became ECU Health in 2022.
Match Day is arguably the pinnacle of medical school, when students discover their next destination surrounded by friends, family and Brody faculty and staff who have guided them over the years. Michael Waldrum, dean of the Brody School of Medicine and CEO of ECU Health, said that wherever the students are matched, they already have a reputation of being health care providers who put the individual patient at the center of their practice.

“Brody students come out of medical school knowing how to do hard work and take care of humans. It’s a very hands-on practical education. They learn how to take care of people which is what becoming a doctor is all about, and the experience they get here sets them apart,” Waldrum said.
The students were presented to the audience of family, friends and members of the Brody community with collages of photos along with music that each selected.
Kari Beasley, from Cary, wanted to use the song “Soulful Strut” from the movie “The Parent Trap” — but only if one of her mentors, Jason Higginson, agreed to learn the handshake from the movie and perform it on stage with her.
Beasley, who matched with Virginia Commonwealth University in Richmond to pursue an obstetrics and gynecology track, said that both Jason Higginson, the executive dean of Brody, and his wife Amanda Higginson, Brody’s interim associate dean for student affairs, were an important part of her medical school experience.
“Being the amazing dean that he is, he said, ‘Of course, absolutely, I’ll do the handshake with you.’ Today, we pulled it off,” Beasley said. “It made it more special that he and I got to do the handshake together because the Higginsons have been a great part of my experience here at Brody.”
While Higginson had seen the movie, he didn’t remember the handshake and dance until she showed him the clip.
“She asked me if I would do it with her and I said you’re really challenging an old man with no rhythm. We practiced it yesterday in my office and then I practiced it with my daughter all night last night,” Higginson said.
The relationships that he and fellow faculty members build with their students is unique because he didn’t have interactions with the administration when he was in medical school.
“This is probably one of the best days in the life of a medical school. This is the day where all of your dreams get realized,” Higginson said. “A lot of them are staying here, which is something we are proud of. Almost 50 percent of the class is staying in North Carolina and that’s fantastic. That’s our mission.”
The Class of 2023 is a snapshot of Brody’s mission to serve the state. The 77 members of the class represent more than 25 North Carolina counties, from Buncombe in the west to Pasquotank in the northeast.
With envelopes in hand that revealed their futures, the students took time to celebrate their accomplishments and reflect on what comes next.
‘What small change can I do?’

When there’s a problem, Merdi Lutete is busy seeking a solution.
Lutete, who was born and raised in Kinshasa, Democratic Republic of Congo, has the mindset of not standing by and expecting others to act — instead, she wants to know how she can help and how her skills and knowledge can lend to a long-term resolution.
“With a lot of issues we encounter, we see a problem and we say, ‘Well, someone else can do it,’” she said. “What’s helped me has been that mindset of, ‘Well, there’s a problem. What can I do about that? I’m probably not even going to get to the surface of the issue, but what small change can I do for this?’”
Lutete has used that formula throughout her life, including medical school. Lutete founded I Am First, an organization that partners first-generation medical students with mentors who can guide them through the medical school process.
“I think it will definitely contribute a lot,” she said. “I was able to apply it to school and I can put it to other areas too, and medicine as well.”
Lutete matched in adult neurology at Duke University Medical School in Durham. As she opened her Match Day envelope, she was surrounded by family and friends, some whose smiles shown through phone screens. Her hands shook as she revealed the folded paper printed with her next destination.
“I was nervous,” she said, laughing as those around her cheered, “but I feel good.”
Lutete studied neuroscience at ECU during her undergraduate years; she initially became interested in neurology in high school, when she took a psychology course and witnessed her father face a health challenge. His doctor was careful to include the family in medical conversations and make sure they understood the situation and options.
“That personal thing really touched me a lot,” she said. “I really wanted to do something like that with patients as well.”
Seeing her own family go through a health challenge and now having the perspective of a student doctor helped Lutete better understand the sacrifices her family and community have made to help her get where she is today. Her parents moved the family from Kinshasa to Raleigh in 2005 to pursue more opportunities. The Congolese community in Raleigh has also rallied behind Lutete and her success. Lutete worked with other students and Brody faculty and staff on an initiative to share information with the families of medical students so that they better understand the process their students will experience in the coming years. It was her way of acknowledging the village that it takes for students to succeed.
“It truly means a lot to them and a lot to me to see that,” she said of the support she’s received from those around her. “One thing about first generation that I really think is powerful is that you’re standing on the backs of many people’s sacrifices. You know that the successes you have you can’t attribute to yourself because you know every single person had a role in that. You’re literally standing on the backs of other people’s sacrifices.”
When Lutete thinks about community, she thinks about how Brody has prepared her for her next steps.
“Brody does a great job of teaching you how to care for the individual, how to care for the patient that you’re seeing in front of you,” she said. “I can give you a prescription for medication, but can you afford it? I can tell you to come back next week for an appointment, but can you afford to come back? Brody really teaches you how to think about the patient and how their story applies to the situation.”
Success found through love, teamwork

When you start off down an arduous path, it’s good to have a friend by your side. When that friend ends up being the person you fall in love with and plan to keep walking life’s paths hand in hand, all the better.
The first week of classes at the Brody School of Medicine in the fall of 2019, Bethany Laden and Caleb Oakley were out with mutual friends working through the awkwardness of meeting the classmates you’ll share the next four years with. He bought her a drink, she told him her favorite book was The Great Gatsby (from which he quoted the last line — smooth) and Bethany said, “we’ve been together ever since.”
Laden was raised in an Air Force family and lived in England and Guam, but mostly in Harrisburg, near Charlotte. She studied biology at NC State and initially intended to apply for a physician assistant program but applied to Brody after graduation. She spent a year as a medical assistant and two years of conducting urology research in Durham. Witnessing a baby being delivered set her mind to being an obstetrician and gynecologist.
“I really like working with my hands — being in the operating room and doing surgery. When I was on my women’s health rotation that’s where I found my passion — working with women, empowering them through their pregnancies and the rest of their lives,” Laden said.
Oakley is from Roxboro and knew he wanted to be a doctor since high school. A teacher showed the movie “Chernobyl Heart,” which chronicled missionaries who fixed the cardiac conditions faced by children who were affected by the Chernobyl disaster. Oakley’s family was particularly religious and did missionary work along the east coast and the film inspired him to be the same kind of doctor who helped people who needed the most help.
He worked as a medical scribe in high school, and then again during his undergraduate education at ECU, where he double majored in biology and chemistry. His first application to medical school didn’t work out, so Oakley taught as a substitute, trained to be a paramedic, worked on food trucks across eastern North Carolina and even prepped alligator meat at a seafood company in Morehead City.
Oakley’s intended career path lies at the other end of the birthing process from Laden. As a doubled-board certified doctor working in internal medicine and pediatrics, he’ll be able to treat patients across the continuum of birth to death.
“They tell you when you start medical school that you’ll find your niche. I had a really good experience out at ECU Health-Duplin which confirmed it for me,” Oakley said.
Early in their relationship they agreed that school would come first and “I’m not going to let you distract me,” Laden remembered. But before long, when she finished studying at 11 p.m., she would try to track him down in the Brody building.
Their relationship took some work, because relationships on their own are difficult Oakley said. Layering the physical, mental and emotional challenges of training to be a doctor on top of creating a new life with another person makes things even more challenging, but with great challenges come great rewards.
“I don’t say this all the time, but she’s my rock. If I feel I need to lean on somebody, I’m going to her,” Oakley said.
Laden agreed. Having someone in her corner, someone who understands the specific challenges of medical school, has been invaluable.
“There’s so much that we go through that people don’t understand,” Laden said. “Not just the logistics of how medical training works, but the terminology and the emotional work that you have to do.”
Match Day is incredibly stressful for any medical student — will you get the hospital you want? Will it be on the other side of the country? For a soon-to-be-married couple, the stressors compound — would they be assigned to hospitals close together or separated by circumstance?
Laden and Oakley interviewed at more than a dozen of the same hospitals to find a place that could support both of their training paths. When they opened their envelopes, surrounded by their families, the learned their residency would take place at ECU Health Medical Center in Greenville.
“Both of our families live in North Carolina, so we don’t have to worry about moving and we’ve already set up a good sense of community,” Oakley said. “It feels like home.”
The art of emergency medicine
Andrés Gil had graduated from Winthrop University in South Carolina when he came upon an opportunity to be a medical interpreter at a hospital near Charlotte.
The talented violinist was preparing to audition for orchestras and embark on a classical music career when another type of art caught his eye. During his experience as an interpreter, he witnessed a baby being born.
“I remember I was interpreting, the lights were down in the room, it was the early shift so the sun was a nice orange glow lighting up the whole room, and everything was going well,” Gil said. “All of sudden you just hear this cry. It was like art. Watching life come into the world was amazing.”
Gil, who was born and raised in Colombia, made his way to the Brody School of Medicine from there, after selecting the school based on its small class size and its community focus. After realizing he was on the path of his purpose, he began to immerse himself in service and making a difference in others’ lives.
“I never pictured myself as a student doctor in eastern North Carolina,” he said. “It was just never on my radar.”

Gil has flourished, becoming close with his classmates and being inducted into the Gold Humanism Honor Society, a community of medical students, physicians, and other leaders who have been selected by their peers for their compassionate care. Gil was surprised to be named to the group but wants to continue on the path that earned him the recognition.
“The people I get to share that honor with are all beautiful human beings,” he said. “I like having that in my wheelhouse for others to know that this is an opportunity to highlight your career.”
Gil matched in emergency medicine at Carolinas Medical Center in Charlotte. When he opened his Match Day envelope, tears filled his eyes and he couldn’t speak. A tight circle of family members teared up as well, cheering when he was able to reveal his next stop.
“Charlotte?!” a colleague passing by exclaimed.
“Yes, yes!” Gil nodded, overcome by a fresh burst of tears.
Emergency medicine felt like the right fit for Gil, who has learned to temper his expectations as he went through medical school, hoping for the best but understanding that contingency plans are important to have in place. The specialty also drew him in because of his overwhelming passion for helping people and healing patients who seek him out for assistance.
“Anyone who comes through those doors is not at a great point in their life,” he said, “whether they have pain, addiction, substance abuse, a car accident or things aren’t great at home. These people humble themselves enough to come and seek our help. Knowing that I have an opportunity to somehow have an impact on their lives moves me to a degree that I really can’t describe.”
As Gil prepares to leave Greenville and head west for the next chapter in his story, he hopes that what he’s learned at Brody will help add vitality to his patients’ stories as well.
“An opportunity to give someone grace, to restore their dignity, is so important to me,” he said. “It makes all the scary things about emergency medicine go away. That moment gives you an impetus to work harder to restore this person, so when they leave, they can go back to their life and complete their narrative.”
Read more from ECU News Services.




