Greenville, N.C. – Coastal Plains Network improved care for more than 27,000 Medicare beneficiaries in eastern North Carolina and saved Medicare $13,220,162 by meeting quality and cost goals in 2022, according to recently released performance data from The Centers for Medicare & Medicaid Services (CMS). Coastal Plains Network consisted of ECU Health clinics and hospitals as well as Rural Health Group during the performance period.
As a Shared Savings Program Accountable Care Organization (ACO), the Coastal Plains Network – a company founded by ECU Health – reached a record number of savings and earnings in 2022. ACOs are groups of doctors, hospitals, and other health care providers who decide to collaborate and provide coordinated, high-quality care to people with Medicare. Under this collaboration, patients are less likely to need repeat medical tests or unnecessary medical services, have extra help managing chronic diseases, more preventative health services, additional recovery support when coming home from the hospital and care in more convenient ways such as home-based care or telehealth services.

When an ACO succeeds in both delivering high-quality care and spending health care dollars more wisely, the ACO may be eligible to share in the savings it achieves for the Medicare program, also known as performance payments. The Coastal Plains Network received more than $5 million from CMS to invest in improving patient care and outcomes.
“ECU Health and the Coastal Plains Network are proud of the providers who helped bring record savings to the Shared Savings Program, which improves the quality of care, care coordination, accessibility and lowers health care costs for Medicare recipients,” said Todd Hickey, chief strategy officer, ECU Health. “With the savings, ECU Health plans to reinvest in population health efforts aligned with our mission to improve the health and well-being of eastern North Carolina.”
Patients enrolled in the Medicare Shared Savings Program see lower out-of-pocket spending on avoidable health care utilization like emergency department visits because the ACO has better coordinated their care.
“The Medicare Shared Savings Program helps millions of people with Medicare experience coordinated health care while also reducing costs for the Medicare program,” said CMS Administrator Chiquita Brooks-LaSure. “CMS will continue to improve the program, and it is exciting to see that Accountable Care Organizations are continuing to be successful in delivering coordinated, high-quality, affordable, equitable, person-centered care.”
The Medicare Shared Savings Program saved Medicare $1.8 billion in 2022 compared to spending targets for the year. This marks the sixth consecutive year the program has generated overall savings and high-quality performance results. This represents the second-highest annual savings accrued for Medicare since the program’s inception more than ten years ago.
“We are encouraged and inspired by six consecutive years of savings and high-quality care, with 2022 being one of the strongest years of performance to date,” said Meena Seshamani, MD, PhD, CMS Deputy Administrator and Director of the Center for Medicare. “The Shared Savings Program is Medicare’s permanent, flagship Accountable Care Program, and we look forward to continually improving and growing the program, expanding the reach of participating ACOs, and addressing critical health disparities across the country.”
Lung cancer is the leading cause of cancer-related death in the United States and is the second most common cancer in both men and women. In eastern North Carolina, where risk factors for the disease are higher than most other areas in the country, screenings are helping save lives.
“We’ve known since the 1990s that using CT scans at a very low dose can actually save lives,” Dr. Mark Bowling, a pulmonologist at ECU Health Medical Center, said. “Now you can do low dose lung cancer screenings once a year if you meet certain criteria.”
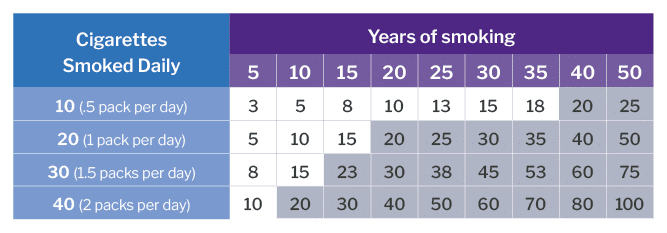
The criteria includes: being between the ages of 50 and 80, having a 20-pack smoking year history – which equals a pack a day for 20 years or two packs a day for 10 years – and having no signs or symptoms of lung cancer.
While low dose CT scans are always available across the system for the insured, a grant program allows ECU Health to offer a once-a-month clinic in Greenville for the uninsured who meet the criteria and have received a referral from their provider.
Jennifer Lewis, Cancer Center outreach coordinator at ECU Health Medical Center, helps run the clinic. She said raising awareness for lung cancer screenings is crucial and can lead to early detection.

“We’re all aware of mammograms for breast cancer screening and colonoscopies for colon cancer, but not a lot of people realize that there’s a screening for lung cancer,” Lewis said. “If we do find something abnormal, we want to find it in its early stages when the outcomes are better, when there are more options for treatment. With lung cancer being a leading cause of cancer-related death, by the time someone starts manifesting lung cancer symptoms, it’s typically very advanced at that time. You have fewer options and your outcomes aren’t positive so our goal is to find cancer before someone begins to have symptoms.”
Lung cancer symptoms are often non-specific, including shortness of breath, coughing up blood, chest pain and inability to move arms among others.
Lewis said she is also passionate about advocating for patients and helping to eliminate stigmas around any cancer, particularly lung cancer.
“We’re here to let people know, if you smoked, if you still smoke, that doesn’t define who you are as a person. We just want to get you screened,” Lewis said. “We’re not here to judge whether or not you smoke. We’re not here to berate you. We will ask if you’ve been educated about smoking cessation, but that’s not why you’re here. We try to make people feel comfortable and feel valued. Your family still loves you and they still want you around so let’s get you screened and make sure you don’t have anything going on that we need to worry about before it becomes a problem.”
Courtney Johnson, Thoracic Oncology Program coordinator at ECU Health Medical Center, has been with the system for 10 years. First, she worked as an inpatient cancer care nurse in the Eddie and Jo Allison Smith Tower at ECU Health Medical Center for about four years and she said it was a rewarding and special time for her.
That led her to her current role in which she helps track and manage at-risk patients through the screening process. She said the best part of her current job is playing a part in early detection.
Recently, she said her team caught cancer in a patient they’d been taking through screenings for about five years. The screenings showed a change in known nodules for the patient and they were sent to surgery to have the cancer removed. Since it was caught in the extremely early stages, the patient did not have any need for chemotherapy and they’ll just have to follow up with future scans for the patient.
“That’s the greatest thing in this position –I can’t prevent everything, I cannot predict outcomes, I can’t prevent what could be the inevitable, but I have a hand in hopefully early intervention,” Johnson said. “I enjoy spending more time with the preventative side of medicine and hopefully allowing our patients to stay out of the hospital. Instead, they come in and we can be proactive with this rather than having to scramble when the patient is in an advanced stage.”
Johnson also shared that radon exposure is a risk factor for lung cancer. She said radon testing kits are available through North Carolina Department of Health and Human Services.
Resources
GREENVILLE, N.C. (November 1, 2023) – ECU Health and Acadia Healthcare held a ceremony today to celebrate the start of construction on its previously announced state-of-the-art, 144-bed behavioral health hospital in Greenville, North Carolina. The event occurred on the site of the new hospital – located at 2820 MacGregor Downs Road, Greenville, North Carolina 27834 – and celebrated the joint venture partnership between ECU Health and Acadia Healthcare, which will own and operate the new hospital together.
Slated to open in Spring 2025, the hospital will be a center of excellence situated less than a mile from ECU Health Medical Center. It will offer comprehensive inpatient and intensive outpatient treatment for adults, seniors, children and adolescents who struggle with acute symptoms of mental health such as anxiety, depression, bipolar disorder, post-traumatic stress disorder (PTSD), as well as treatment for co-occurring disorders. Thomas Construction Group is the general contractor, and Stengel Hill Architecture is the architect for the project.

“Too many people, including children, in North Carolina get stuck in emergency departments when they urgently need short-term and high-quality behavioral health care,” said North Carolina Department of Health and Human Services Sec. Kody H. Kinsley. “This new hospital will create lasting change in this region by making behavioral health services easier to access when and where they are needed.”
The new hospital will also serve as a teaching hospital for psychiatry, social work, nursing and other behavioral health professionals. This will address the shortage of clinical behavioral healthcare professionals in the area, training students and residents from the Brody School of Medicine at East Carolina University, many of whom will go on to practice in eastern North Carolina and carry forth ECU Health’s mission to improve the health and well-being of the region.
The hospital will include 24 inpatient beds specifically for children and adolescents with behavioral health needs. These beds will be the first of their kind in ECU Health’s 29-county service area and the only child and adolescent beds within 75 miles of Greenville, North Carolina.
“The shortage of mental health resources is a critical challenge in North Carolina,” said Dr. Michael Waldrum, chief executive officer of ECU Health and dean of the Brody School of Medicine. “We are pleased construction is underway for our new behavioral health hospital, and this moment marks another milestone in our effort to improve access to behavioral health care for the region. It will provide the hope and healing residents of Greenville and the surrounding communities need when dealing with complex behavioral health issues.”
Prior to the pandemic, nearly one in five North Carolinians were experiencing a mental, behavioral or emotional disorder, according to a report from the North Carolina Institute of Medicine’s Task Force on Mental Health and Substance Use. In the past three years, national data indicates a growing trend of depression and anxiety symptoms. This partnership demonstrates a commitment to addressing mental illnesses and substance use disorders, normalizing and treating them with the latest science and medicine in appropriate care settings.
“This new hospital will provide North Carolinians with expanded access to quality behavioral health services and treatment from specialized clinical teams in a carefully designed environment,” said Chris Hunter, chief executive officer of Acadia Healthcare. “We are so proud to be affiliated with ECU Health, working together to address the strong need in this area and building upon their legacy and commitment to behavioral health services. This hospital will be a strong member of the Greenville community, collaborating with all organizations, hospitals and first responders. It will be a beacon of hope for patients and families in eastern North Carolina.”
To learn more about the partnership between ECU Health and Acadia Healthcare, visit ENCBehavioralHealth.org.
Each Halloween, patients, families and team members at Maynard Children’s Hospital at ECU Health Medical Center get a chance to break away and enjoy the holiday.
Parade floats from team members and community groups flowed by the Children’s Hospital on Halloween afternoon, giving the children a chance to see some of their favorite characters, like Barbie and Ken, Minions, and floats from Toy Story, Trolls and Encanto. Even the Mystery Machine, a Jeep full of sharks and a pirate ship appeared – all to help make the day a little brighter for the youngest patients at ECU Health Medical Center.
Amanda Jones, a child life specialist at Maynard Children’s Hospital, said there is always a lot of planning that goes into the event, but it’s worth it each year to give the children something to look forward to during the holiday.
“This is a really fun event where they can still celebrate Halloween even while they’re here at the hospital,” Jones said. “It allows kids to be kinds while they’re in the hospital. It’s something that they would normally be doing if they weren’t in the hospital so it kind of brings a little bit of that holiday spirit to the event here.”

For parents, it can also bring a source of comfort. Angela Blanton’s 8-year-old son, Chance, is a patient at the Maynard Children’s Hospital and has a rare condition called Walker-Warburg Syndrome. Blanton said Chance could not be outside for the event, but she still wanted to celebrate Halloween – her son’s favorite holiday – while at the hospital.
She shared photos of past Halloween costume contests he had won and reflected on what this event meant for her. She wore an inflatable chicken costume, worn earlier this month at a Halloween party with her son dressed as Colonel Sanders.
“He would love to be down here, but he can’t be. So I think it’s amazing for the all the children that can be here,” Blanton said. “Seeing them light up, and even me, in this silly costume. Some of the kids wanted to take a picture with me, and I thought that was awesome. To see the smiles from the kids and parents and know how important it is for everyone. Not just the children, but the moms who have been there by the bedside.”
She shared that these events mean a great deal to the patients and families looking for a piece of normalcy in a challenging time.
Patients across the hospital receive goodie bags with art supplies and toys after the event, whether or not they could come. Jones said the event is important for team members
“This is a great event for team members that participate in the parade and for those that come out and watch it,” Jones said. “It’s enjoyable to be able to step away from the bedside and spend time with patients on events like this. I think it’s really uplifting for everyone.”
Ahoskie, N.C. – ECU Health Roanoke-Chowan Hospital hosted a community celebration Tuesday to proudly commemorate 75 years of dedicated service to eastern North Carolina.
Established in 1948, the hospital is dedicated to providing exceptional health care services to its community and has expanded and evolved to meet the changing health care needs of the region.
“We are immensely proud to celebrate 75 years of serving our community,” said Brian Harvill, president, ECU Health Roanoke-Chowan. “Throughout the years, we have strived to provide high-quality health care services with a patient-centered approach. Our commitment to excellence and compassionate care for our community has been the driving force behind our success and continues to positively impact those we are proud to serve.”

Situated in Ahoskie, this 114-bed hospital has been a cornerstone of health care, offering comprehensive services to nearly 40,000 residents spanning Hertford, Bertie, Northampton, and Gates counties. ECU Health Roanoke-Chowan Hospital offers a number of specialty services, including behavioral health, cancer care, pain management, wound healing, sleep services, pediatric asthma management and an ECU Health Wellness Center location in Ahoskie. The pediatric asthma program at ECU Health Roanoke-Chowan Hospital helps children in Hertford and Northampton counties miss fewer days of school, participate more fully in physical activities and look forward to a brighter future.
“Over the past 75 years, ECU Health Roanoke-Chowan has been dedicated to providing exceptional health care services, and this milestone marks a testament to its unwavering commitment to the well-being of the community it serves,” said Jay Briley, president of ECU Health Community Hospitals. “These achievements reflect the hospital’s dedication to improving the overall health and well-being of the community. Today is a day to celebrate the contributions of our current team members and those that came before them to help build a legacy of quality, compassionate care.”
Since its founding in 1948, ECU Health Roanoke-Chowan Hospital has continuously evolved to meet the changing health care needs of the community. On Oct. 24, 1948, the original 40-bed hospital celebrated with a community open house, officially welcoming patients on Nov. 1, 1948. ECU Health Roanoke-Chowan Hospital holds the distinction of being the first hospital licensed by the Medical Care Commission, still bearing license number 1, marking it as the first hospital in the nation constructed using federal funds provided by the Hill-Burton Act. In 1952, the facility expanded with the addition of its first wing, accommodating 25 additional beds, followed by another 34-bed expansion. By 1975, an extra 50 beds, 10 intensive care units and a third floor were added. In response to the growing community’s needs, the original structure was replaced, culminating in the dedication of the present-day hospital in 1992.
“As we celebrate 75 years of service, our hospital’s commitment to clinical excellence remains unwavering,” said Dr. David Lingle, chief of staff, surgeon, ECU Health Roanoke-Chowan. “Our legacy is built on a foundation of dedicated health care professionals who continuously strive to reach the highest standards of care, ensuring that every patient receives the best possible treatment, and making each year better than the last. It is an honor to serve alongside such a great team of professionals.”
ECU Health Roanoke-Chowan has achieved numerous milestones throughout its journey, including recertification as a primary stroke center by The Joint Commission and the American Heart Association/American Stroke Association, Get with the Guidelines – Stroke Gold Plus with Target: Type 2 Diabetes Honor Roll and earning accreditation by the American College of Surgeons Commission on Cancer as a Community Cancer Program.


Students from the Brody School of Medicine, ECU College of Nursing, and Department of Physician Assistant Studies participated in the Interprofessional Triage and Emergency Assessment and Management (ITEAM) Day mass casualty training event hosted by the Brody School of Medicine’s Emergency Medicine Interest Group Saturday, Oct. 14. The training provides a unique opportunity for students from different health care disciplines to collaborate and gain hands-on experience in managing emergency events.
Experts from the ECU College of Nursing, Brody School of Medicine, Department of Physician Assistant Studies and ECU Health EastCare gave students interactive instruction in procedural skills, such as basic airway management, hemorrhage control and triage techniques. Students then applied these skills during a mass casualty simulation at the Interprofessional Clinical Simulation Center at the Brody School of Medicine.

“ITEAM Day was beneficial to promote collaboration and interprofessionalism among different health care providers,” said Stephiya Sabu, first year Brody School of Medicine student. “Doing this in the setting of a mass casualty event was important as they can be very stressful, and having this experience beforehand will help in the future if we are ever in that situation.”
This year’s simulation was a mass shooting incident. The Office of Clinical Skills Assessment and Education provided simulated patients, portraying symptoms and behaviors consistent with injuries sustained in a mass shooting, including confusion and panic.
Adding an extra layer of realism to the exercise, the ECU School of Theatre and Dance lent its expertise in moulage and makeup to create lifelike wounds on the simulated patients. The ECU Student Government Association provided funding for food and materials.

Students participating in the simulation were coached by a multi-disciplinary team of experts who provided feedback throughout the training. Chuck Strickland, outreach coordinator with EastCare, served as an instructor and provided invaluable insights into the role Emergency Medical Services (EMS) plays in a mass casualty incident. Students were educated on EMS’s initial response, patient management and treatment strategies.
“It is important for students to know the role EMS plays in initial patient triage and how we would request resources and determine patient destinations,” said Strickland. “EMS identifies the volume of patients and their acuity levels, then gets nurses, physicians and physician assistants to do on-scene care for high acuity patients. Students also learned the role of critical care transport and how those professionals would be engaged.”
Nursing students, medical students and physician assistant students shared their respective expertise while working together to promptly triage and treat patients. Both students and instructors underscored the significance of applying classroom learning to simulated real-life scenarios, highlighting the practical value of such experiences.
“Recent events in our community emphasize the unpredictability of mass casualties and just how terrifying they are,” said Lachlan Younce, first year Brody School of Medicine student. “As a medical student, I seek to understand my role as a medical professional in those situations. Participating in this mass casualty exercise exposed me to vital skills like patient triage, resource-efficient care and the importance of teamwork when working alongside my health care colleagues, including PAs and nurses. I am thankful for how this ITEAM training experience helped me develop my readiness as a medical professional.”
Greenville, N.C. – ECU Health is pleased to announce Jenny Markham as Chief Legal Officer for the ECU Health enterprise. Markham officially began her new role serving both ECU Health and the Brody School of Medicine at East Carolina University on Monday, Oct. 16, 2023.

Jenny Markham
“Jenny Markham’s appointment as our Chief Legal Officer is a transformative moment for ECU Health and Brody,” said Dr. Michael Waldrum, CEO of ECU Health and dean of the Brody School of Medicine. “Her experience navigating complex health care transformation will bring tremendous value as we continue to build ECU Health and work toward our mission of improving the health and well-being of the region. We look forward to her expertise, leadership and partnership in achieving our collective vision of becoming a national academic model for rural health care.”
As Chief Legal Officer, Markham is responsible for overseeing the ECU Health Office of General Counsel and all matters within the framework of the joint operating agreement between ECU Health and the Brody School of Medicine, including the health system and Brody. She will report directly to Dr. Waldrum in his dual role as CEO and dean.
Markham brings a wealth of health care legal experience to her new role, having previously served as system vice president and deputy general counsel at UNC Health. Markham earned her J.D. at University of Richmond School of Law, and has experience working as a health law associate for a large North Carolina law firm. Her deep understanding of the intricacies of health care transformation will undoubtedly add significant value to ECU Health as it continues to evolve and strives to enhance the health and well-being of the region.
“It is an honor to join ECU Health as the chief legal officer,” said Markham. “It is immediately clear to me during my brief time here that ECU Health is rooted in service to a mission that has profound impacts on a rural communities across the region. I look forward to contributing to the collaboration between rural health care and academic medicine as we work together to make a meaningful difference in the health and well-being of our community.”
Doctors, nurses and support teams in the ECU Health Medical Center emergency department understand the importance of being prepared for any scenario. That is why the Medical Center ED and Trauma Department teams took part in a mass casualty disaster drill Sept. 7 in an effort to test and improve knowledge of triaging, EPIC documentation, response roles and more as part of the American College of Surgeons accreditation process.
“The more prepared we are now, the more lives we can save,” said exercise director Dr. David Trisler, critical care surgeon at ECU Health Medical Center and clinical assistant professor of trauma and surgical critical care at the Brody School of Medicine at East Carolina University. “Our community depends on us to be there for them during the most difficult circumstances. These types of exercises ensure we will be able to meet that need.”
Mass casualty situations can be difficult to imagine, especially ones that happen here in our local community.
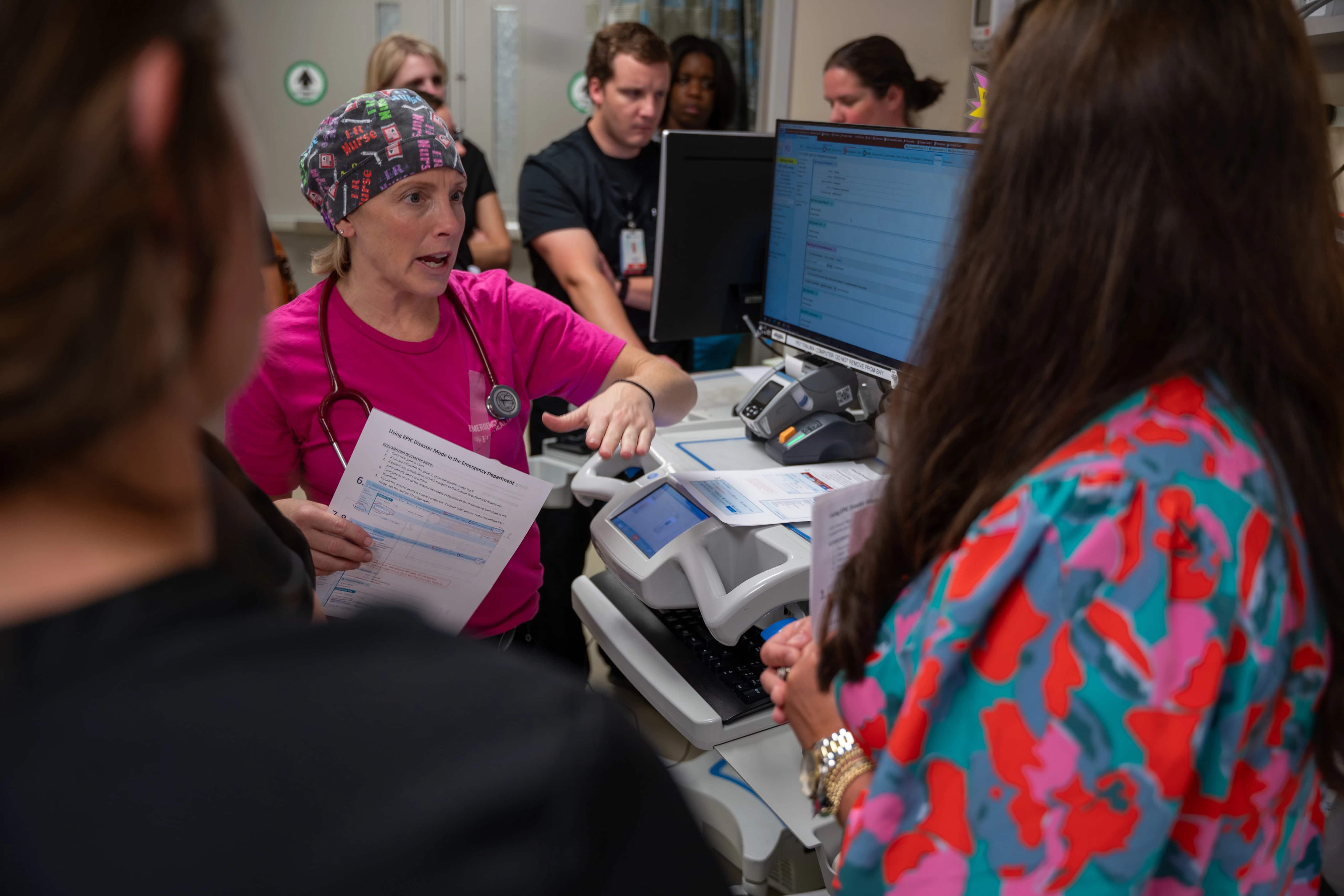
With the use of inflatable mannequins representing the both children and adult patients, the disaster drill consisted of 30-40 casualties brought to the ED following a simulated mass shooting at a local event. Drill participants worked through triaging the patients based on their medical status and moving them through the emergency care and surgical process, using real-time information like numbers of ORs and beds in use during the time of the drill.
For Dr. Eric Toschlog, chief of trauma and acute care surgery for ECU Health Medical Center and Brody and the rest of the emergency department team, preparing for those situations comes with the territory of working at the only Level I Trauma Center in eastern North Carolina.
“The ECU Health Medical Center emergency department serves as a hub for 1.4 million people who live across the region, which highlights the importance of being prepared for any circumstance imaginable,” said Dr. Toschlog. “The more we work to improve our process and understanding, the better prepared we will be to save lives.”
Those involved met immediately following the drill to debrief on the exercise, closely examining strengths and weakness, as well as plans for improvements, all in an effort to ensure the Medical Center emergency department team is well-positioned to provide high-quality care to the community during a time of dire need. The common thread throughout the event and debrief was the direct correlation between preparation and lives that could be saved.
“This was a great opportunity for us to test our knowledge and we certainly learned a lot of valuable lessons that will serve us well,” said Dr. Trisler. “I could not be more proud of the entire ED team for taking the time to participate in this disaster drill.”
Greenville, N.C. – Members of the U.S. House Committee on Ways and Means visited Beaufort and Pitt counties Monday, Oct. 16, 2023, to engage with the community, tour ECU Health Beaufort Hospital and ECU Health Medical Center, hear from community care leaders and discuss the challenges facing rural health care in America. The committee visit consisted of Rep. Greg Murphy, Chairman Jason Smith, and Reps. Adrian Smith, Kevin Hern, and Claudia Tenney.
“Whether it’s in my home state of Missouri or eastern North Carolina, rural communities are facing a health care crisis,” Chairman Smith said. “Today we heard from health care providers and local leaders about the struggles their communities face ranging from patients traveling long distances to receive emergency care to health facilities finding and keeping a quality health care workforce with the scarce resources available. On our current path, access to health care for a huge portion of America will continue to erode, putting the health of millions more rural Americans at risk. The Ways and Means Committee will take what we learned today from patients and doctors on the frontlines of this crisis and use it to inform the best way to expand access to health care in rural communities.”

Committee members and county leaders started the day by visiting Belhaven before touring ECU Health Beaufort Hospital, built in 1957 under the Hill-Burton Act that provided federal funding to support rural hospitals. There, committee members joined a roundtable conversation with ECU Health leaders and Beaufort County community leaders about the importance of finding collaborative solutions to the complex rural health care challenge.
The day concluded with committee members visiting ECU Health Medical Center in Greenville, a state-of-the-art academic facility that delivers high-level care to residents of eastern North Carolina. ECU Health Medical Center is the only Level I trauma center east of Raleigh, showcasing ECU Health’s unique system of care that serves as a national model for providing high-quality rural health care.
“Chairman Smith has been gracious enough to organize field hearings in the country this year on various issues,” said Rep. Murphy. “I am glad to have him and other members of the Ways and Means Committee spend time in eastern North Carolina to look at rural health care. We had the opportunity to witness firsthand the efforts of clinicians striving for quality in medicine while ensuring access to care for all.”
Throughout the tours, lawmakers walked through the emergency departments, intensive care units and labor and delivery units and engaged in conversations with clinicians regarding the challenges faced by rural health care, the aging infrastructure and the difficulties associated with sustaining essential services. Leaders discussed the importance of preserving services such as labor and delivery units within ECU Health, which are a lifeline for expectant mothers, providing essential access to safe and skilled maternity care, often in regions where other health care options are limited. Maintaining units like these ensures that rural families do not have to endure the significant burden of traveling long distances to access critical services.
“ECU Health has long advocated for solutions at the state and national level to combat the intensifying rural health care crisis facing America,” said Dr. Michael Waldrum, ECU Health CEO and dean of the Brody School of Medicine at East Carolina University. “We are pleased legislators not only recognize the need to explore solutions to maintain rural health care, but also recognize ECU Health as a leading voice on this important topic. The visit to Beaufort County and Greenville gave us an opportunity to show our mission in action, and we are deeply appreciative of the committee for spending time with us discussing rural health care.”
![§êÌ4 VYz½5Ñkã$¿òq³'Ô[¢veÐÆï¤DB³§ÍÐW28ø`Ò1ñMçÚíäuÓ@£CND£1-æ!^ÆÞkÝõW_N1´c§¨kO½Fa îÒú4¶
æÒÉöµTñÕx|9d!ÞÊ"Q¸m^ÚNmtx9* ô" NÙ$ßáÝ£MG*ðn@Ò|NÎ9*º··¿e´Jy¿#@ÁAb+ïLÇÕ
Q2¼×Íú3AtÆÅY-áªÛíäøåXynÇ4wÙ :üñÆ©RGFVé_[á¡ÿÖU¿.`tæ0ñ_ã,KÏ|ýes§kQiz|+Ís=NåØòýe$M'KÐN5YÒ;pL¬~Ñ¥@Rx|Ãåv9;(ãl£ÈúGÔ4·´îK V«/"U·§ÚæX.¼H¶ÑóRêYAøØ(B3Õ¸DÈÈö¦Y×$nåXøÅs&V(±)SRkkdI¤M*H
Y~t#¶S>lâU~¦é**Àl<r²È1åó74ëK{(áµAgÉÞI#äKP¨¯*{e' %Ø)æõK3ë[Å2TW&Ë!H¥Ó¦Iã¡Ûy?æºÍ¯ssÉé7²¸åô×12`â2ý.F<ÕQ®lf/0k¯ª=^2Æ1â(ÁJyoϦðÀ7|C³ H_ILE׿ßùæ®bÛwK¢ó&¿q¨Maos@HqÀµ7© wË#K)ÄsD¿4-ÊÅqºìyãZmCL£µn±%½²9-ÌOõÈXM"ó(Ì8üPTøä±â]"cÓv/uí[ñ¡ã¦Ï(wjPWímøµä¹³Ý¥^ZEÁÓþ59dy|ÃmF=9d/ á@Ì:åpÕBÏÙ.ÒîmfÄûàZC-ÅØ°4?:ò²L)ÛÉþ!¢ãÐõÉHòoÅV:°??*VNÎÐ+w5¦dc<L3a1×µ{ÚÎÚ^ÚÔBÑÆܨ§L8¨nQÕOÿ×}ªß}pZâQ³ÇǹíPs:ZQÍ×EkÚJùÙ3z(0Iô
M[5ú%#¨èÊL6s#[м¤Íyk4ìÆBÒ¸æv¨SÄ~2áË+>l
lW¾Q -õ86)Z£ü¬¤@ÓÂq£ ]>":¬¯O dOÔËøS¨£BMk½r¹óH^a^2²Ì0^ÿêZúÁY7§"§ÃžéBzµÓÆC·Ãb°´
!»D v éDP§]2L(¥d.ôÅ:b~bÚÂöWìT3#Eĸ5^FbæêÛêkß-i1ÝÁYçXÌãÈ19D£éG¥dN¹M6Çt8y¾ýiMäýiXóý!Óº°%'â|ÎÁ¢Ã&´F< ñú¢ÇµKÍBö[Û빺ÕåsSOࣲ¯Â¹¶§TM¥RÆÖ¬~d%ij'ùÒÎÅô ¾e·6!Uû@þñsW³±cþ:çÃ_¿ø¤ÃT×5mPúß¹Cö6áÑÛ½ßÿÐù×ÍóhÓ[gPyË)ÐúÍL<l[ϯ/äÔ¦ÊUfÚGU new)é~MÊÚ¬m7Z!ÏÕy]ÆXzwâ5ªÊëýâ·üy@â!»e9̼bº|iäãõÐÊyDÛmºäLX6HÛdU%~½Ì~¬ZäiØ-{M'êÈ©ð§l²/~¹ sHyGæuÓWz=
ÙÚ0#ýÐÉãñÿkíxdKt");ü°o0i×Zl³Q¬]f?ÅDí·óWøå"¨R¢l$×þqÔtZîæ-FHÄ=O#BKMò¹nYOMò®uÝ'N¼Bfæ[yÈ'º'¦Ôʧµ2wég]°´°_?¥tÍHÿëLÇÏȳÃõ=Ç×t8S¬Tñôù-GÏ*#Ò@ÛÚÿ¤ÇQ±9PíìÁou]#Í׳TG$íâ+ñ7WîËñs,rdÐOÝÔsÄA¢R¬;G5]¶lEÉìáÍ¥²^^ê6²AÊÆÖ{¾U$ÙÄdÿ¨9¾ÿðþ|ÞvV qKù¡ÂÖd1vðÌ¿6y£Ì`êºMª´è#û*йR9þÏÚ9N ¾g_¡ùßTÒì¿@ÉtÇC¸9&½ í$uû ûÅû-ö¾×Ú®Pú¬"Ãmæ©5·ú«pEÎ0 !¤PXÐ|&µ4Z¸GL¤G¿Ódñý êÞe·]fÓHk«K{%#-ÁûM²9NÑâ þ&P÷2þkÐuÏ?ÛùGË$EgÕf-´/Ñ@3IàgöÛáÍîÜéòß5y_[ÛëËÉîòåÜ]ÊwbRÿ*Ï4nÓÏ&ù¿UÓR[b7¸²°lĸ|~8öÿegJ% zd£/úªzæ&³®ÌI_®?ÝEö#E²*ñí¶npÆPu9 <ÒöÔç/kX×õÈi'®VY
rTÔ¬²O4]JVs m¨¯b3(mÆ_ÿÑåk¹kú3o¬Ê½Ê/à¹3r%¢á1ëPûäJSXG)=;0MÞÇ¢Î2169«ùkÏ6÷¢ÂjÆöÞVäÔGï,2/òÇ!@ÿ³pÊ"AÿU¿)<@sú¿£'¡¸øÌ°ÃrJëjAgb''¹sePyfho&UÒåNcýzdIl«j]§ þ¤ò?v¦U(KFëÆ´È Ý_1ëz§¯æI§äY¥jíË érFÛ3ïÉ]yí<ÙqjÌU.m%§J£ÐýcæÃ''j¼qÉ3ÊJÈ*»Ðnj2¶W³Ù¿ 59[OôxîZdcÝÌ,¦Ô^°¼P¼Rº?kß+¶MÄyÿµ}?êÚ6U ©âMTÐ7NlÄ=a1E·¦1ÖËñȤ'øÊj«21ØR}dy<§Í0¥Ï%Inn¹óÓ ÔaRúC%7vZU·`ÖX+ƵÜBv&¯íG)#ÎRámÒKJG¢Où»æ?ðç,¼±jôÔu gÔåhÆw¿ñþ?ßIN,CDG(U)#üO~æå!v â³¹½K6ÀrM22KÖüÑ®7¼¥mgæB.,Èôû}£OòóAæsþO«úÓþÿÅ;èfü®aûÌÓÿþkÉ }BíaæÅ¥5RI ~ÓÖ¿ñ¶n¡Ø:9HgrÉ5/0ÞjS¸WÄ«yI(¿«2âE²m*FkÈ@·@ÝkC@©u±fåÍ!äyÂþÏß×.Ä:µä^¯Z3 4JH{o1TRyr¹3~¦ùYJe¤Üà«/&ÈsÿÒämhíµíGn6Þ»èd!,Ì DÓ îJUþ$G¾?²N¶ÐôÛ/£[¹Ü@2Àñ5ëÓ+ÈLbHæÛRòzoéÛh,Ù[E¼GuaÌF*9n¨JýVî¥Âù´ô#_ë×zÚö»h°ÔÓ-@!äã,ªßgû)Ù6åÑÕ@ ú²'ÝCõ ò1ã²w^JÈ´æÐõß=LçFF·ë¶ñ7ôã§Âð?Õ=2AÇ1=ÌfòfPú£±øO,³HÝñÈÖϵm{=] ¿S£hÜIý ¶ea¸#(É®©¯®å²óN¬CuFKi:·ÝÎÌsLÐX[Üë%Y-TÕ·:t+[>÷»þKy'_Ó§Z»·úµ¥Ýej£*üÕyW¦bd³0z/ãRñJÓ]²ËqX極½ÕêHÿ^¡PH*½ËNê;æ6|qÜõoÅVDÑB&Ï¡hã$vÙwýx"}!¢²qá
'¬ú^#öÑzÄóÎEÎ/.iÖ1$)ªjÖÑÜøu¬Z©,Q9D¿ÿH±Í2 Gó)ç¯5Mæ8_êåÕKzzvñ|1ö{ÉþÏ6½@ů¤hÚ-÷,?^ ¤2![[ÜyÒk&{ÆZs¢ÔììþÇ(ÕÈf>W§ênÓ@þêUæM[Qó6½uyRÝ "B)!öKÇo)Ãbn«Ps϶þÿ6*hvü»ßónfâ»U6¶y;ÌÄÉÛlº,/J·YaY@6ñ¸%HûmMþjË!#äÆR
Ô$+HòDýOðÌE«Çs°ñ$ÒÒµ½ÈuÛ%Ú%V,iQ÷ä¢Ç*,ÂÞ[åd²Ltuå3V{ääÙoÿÓåÿvù¥½9%¼ZtõQ¿98µF|DéË)Zw]ËdÂÓPT´¼©$knÿËûÀdéOµW%Å|ÑîDé÷$I$ÇÐiJ¡9ƽía[¤Ì}aç¼Ñæ·µyM±;"6<ùÄÒHåðû´ÿdßäãÆ@:Ä·äÆb"zLqEª@§P¸QÈ;(è;3×æË ÐèqDâ! õH^gþz?õÌÌdþqsÍ÷eMîé{NÌÛÈ^hòõç ±Ò¹ÓY-æâÄHÊUç@fõQþ3c$-F'@Éy×Ìi¬ù½(âT².!RuST¯Òî}>ÖdÝ$7_(9Bhm¢®«ûÔÜéQ±ÉÒ D¼L>Ì®>ãúÆ ¼cóÿZý©yX»ótîußh} vÿ*UÌ}Dµæ;%!XȽ=mðÛN/,í#´hï8þÔv?~eÄp¹HÜL!´¦¸zásA]éóÊçà ó§ïü·æy4[×æÐÃÄÒ£àOÿ¢ËP°$`ÙrUÙëÜ(¥®LÂÎùYdè*Û8#½øóݲ/ÿÔäs×#Öõ»R(M¼s¤Aab ^(î=Æg4F$ØܱñqEì+÷bè«JiÀñZÓ¬¿ËRÛêw:mêÒé²YÚÌ×/»TzËéDárR>>¹®Ê9JGéÙÂG68cV>/ô¿ÂõA>:Èéy%ÅÇr`hÔ°©'lÐë! HÏð»)"#ÃÉ'ó]ü¯} (T·/³ÛlÂÓâGúÎNrx¹çþOý";fë[ÁᯱÕi¼QvüÁ¹ºW+úZmØøåý,'úÍ*Ê?ªÁ^Y§y%K$ z£áOPñ^Göy6EÕݧ>Y§ÖôÛZFææy4`8F§_Ùm± E¦£O´t«H¬tûk(+hÒ$g5b¨(*E3Zåpm°¡á¿~m¸ÈË4ëéÙ^)üFbäæ¬DÐzÑ®nUA:Ð$ïL9QR¶Ôɧ#jýù2¤'"@êèp0ÿç!tÍOVóMÕcåm¤i]ÝÊkÅ¿*WùØGð®ei2ñçÑZþÕ>{æÀqÐ>lXH¬vNCY´=bÏC×µ©àhíÁdF^_"W°âE>#_ÙûY9ÇüN~r<RûW§þ%ÝÌW)ɨÿ¦ì;ì¤C$G%{¥»±3DI¡¹òYÇäVjx1»¶2;&zµåO©Z©ÝHÞ¹<»53/ʨ[éZÏîxÇueÊ8¥xÀ1Ú²}øÁ2$Û³ÒDQ=ÌG_×õ1jÒëz³î.(¾+Â5éð 9±Çºu*¢Ó¸ãï±1S»·¾<ÒwÀT4ªYÀI¦S&qe¤PD!or@Ìkm§ÿÕás3Mé§Pîݼ>YcZáCLiWðä¤c%£òÓK¿´óïjðúð³Bd]N%OLÑöQ,fñ;®ÎÅ(dõôþ§§Ä@yþqÿÐϽÊf¶+μüknz·~-gbÜëÐó=®}þhý*:^OË¿0_ºÊoC8ªG§HTl]å2o$ÿ7ýóÅB¿¥ùsgëù»AE&ò'úó?äô¢?Sëø[á_Í;l(ycµ¹óôn¼I¤©îadúË>¦4`íiv¸1²ÍÀ1âM:áD¥FÂÑ'Õ¥ÃÛjc1ljÂ|²y¤z"0e4øR85 %T¡å_ø.Y9©³.£®ôýYE5¼Ñ´¡KsP¿:Ó24Ó¾Y¡=jSóD7ÓiãI¸æÝÌ|3éµý-×ífôån´@Ý=3Eü²Ó,4M4kÞ¡kÎW?²¯+eÿ)TÚÌs+-£ÌÎ/ÊrýÚ_(Å1ëéûÿÅñ³æk(Ë]ÄÒRõíã'Svcæh CËô Æ×Ì·Ýbâ¤Ò´®ù Ù#`º+yáÛd²2¼áÒ, ¯×½3/Í¢ye úK^¦7Åuùx_sA7ï`0%¹lGHÄ(%a{Éô/ééd·ImÉHV@ݺ×ÍiW2ÔQó{HÞ@!?ݳ%¯bGÅ2Ë+ÙÉ8õJnü¹u<wRFn¥5=iO÷êÌØrMô[hÕj{dk#uÑùqCWÕð8miº@nÿÆÑH{Í.që+Ô+Jÿíeº©_¥§nc?t?KÑ ´º½=ÁäHOÊÓýÕÂYü<RÿsêvØ2pcâû¿CåéA©H¿³îµöW#7úÑAf·ÛxÌÁ Âäxûk_Ãa´.28uEAðømúï%<äú
$N.:2î§øØqVÅÄ«Ý¢@hõelÁMc©)ZSz|ò5Ñ<][1
ÆjOÉDéïéÎÓÇÄÄÈvo#¡äFÃáÐÿÿ×ä_òBbÕ?+}Ê¿Epê
ÀÓ¡ dæOé=ìïð BÈäxþ×NMKUAÄw`¨ I=®òX£t^ÞKYï,n-àhd'E%ÜËÖ¹Xª'ȳÈéGï{o=ózÀT¢÷¬?â+Ù+á«ó9Qí`½¶y²×z#<§ÍnüÏtõ·Ä¦µ@~ë4c}Ï/¬7WË~ÓþP¶xtØát1²ÆëÄYµþ®ÔúOOõGêÌ#ÉÊêÊ-Y~¯ÿ!VkÜ5ÜîÓL®L¢F±dQ·r0!¯¯ZýêÁR¸êv¬«
êº
¼ª«~À~ÉÓs-¹;q#½ì1&Ì[+EA_ǦdåjÇ+.)*þ#¸Ëþbk2ÜYÙØÀ4v9@Áòª8£)èËþ)ÚáiLåÅçý1ÿ|ùãÏ$Ú-õ¤ß¹Ô-EЮôríÈoþIL¾98÷ºøiÅ<s3TùCØ2!ml$«P|N<@Þ(³Í8±Dhçd)¦Êµ§ãiż¦÷©Æe#äs;/0ãcä[qD¨9gF´<jDORÈÒ[=0Q®LÂè¨Ç`EkáQyžÓé5;Ï)'Gaá[hÿÐàeÌ×@#/ð«ÕÛlÉ!eÌ!E¸UQ¹' s°ùÉÖÚ=º^^F²j;Aý÷þfÌlâ÷2ý¡2 3ö
GãJ,ÁI|ÍäHî¯4Y&;µ©7_
½¾ÎRqǸ9ÔËaÇÊÚb4aI ®PrDtsÞ×GäË×qX[c]ã?ǬÓÌÚe¶ÜG¬1ÕArà³'&¦5N¯Úí´^ð/òY>«áàâfó¯Î0Çg£Ü¡·&ÝÜvG¯û(Êåzy¬ÏHy,¯J£¶e8Ìà:Tø+"ókQ·/Ëðbv/Bógí<µsi¦Ûô8eV5ç3ý¹píz77&'}H=ó7&î<wɳü«)Ûj; 4i,Ùr¹2%Ik*ê§1æ,6ÇGõPU¶ÌqoÏÿÑä^sò¾[Ö@(_N¸~vïA½Lu?áýOMN;ýIÍUÑ3ò·Zês`µjBC)ïþÀ~9~YíM@=J ëê[Nô 4òq±2G}tDEFöøZ@[J9mÝå5nl+íMPõ»ô"ÃÚÖ¿!Ôå4òÛëÞ[þÒn?0N©+ÖÀZ´k@)áQUäâ@ÎÞÁeujmô;ñ?Ó1ñE¶eåhߣ¼ós¯-½ºiaAeW£uç»W2É@Dêúmõµå¤wÕx¤è}ÆÄf)³u§i!à;`BâF0¬õ[Ýr*³Õ~ø¤ò·"+_U-Õg1+hǪþÓoòsc§¥ÃÊwGh5½+m#ÖGù·öfyqH+h upæI_âD5Øffè6_©çºL©?õiuÀTqßüÌé@õppg<`úKú^÷ª?:×B£9cõÎ6òO1ù_VÒP·1¯¦àG©V²XÏq9vHòÆ´?êô¦ß~7U¤dJB×sM².Imh.e.â5b(M7ö9i²1)K'ï)Ú+tÛÿÒçíPó ÂÐÁ(¹ü¸©{që×5}L!.nË>H ô4éZuµ
P1$SmËoüÇ6²$V[1'$S«sÂ?|¼lÍFÝ^Áf??isYwQPãeZíáÓ)rú'mÿ6
Ðh¸õýõ¿ßËx5ð´æ`HãJtÉD© g,xÈî:à[ÁH"¢$R¶À¨K¹ l0Rä)×|PWÚ
Aup±s¨N[VpR@'Õ|ÿ¢ÙÜ ^S?°ã1~Lüæ§mæ]:ÿPµ?ZN39!M?-FNgæËbáÃ÷¤jvþôíÀg$¤z¡®Zhë˲²×è9²Ä=!ÁÉvóémmc×nµ8'KÉ¡BÔ²AíÆ^|æQáîFGe9,H/Ôu[»2êÕËAâ¤uÌhósä<HÔ7ÍuLlmJ§
dt?ª¹Ld6}Qä@]ùwIºÿZÂ[æPWñÄìXôBùÛJêkdrDÁÖ#údL-/såZÇ-¸<ÅVQ³)ùÊy× 63}äM6 Kr;})fêÄbèË*A#¨fjç¦Z÷ýÆw*éZFês5©c¹ûÏL¥õBIù42::§eùü+ÿd°ÆíSTÂ82ÉVï×èï»M¿ÿÓ-óÜH°§#ñRiß-:lCCsä«)·/ 鶱(Smj¼Í7¬òû_ì²ÌâÌbl°JÐCSl(QbPåS;&«_M¶±
uWDÅk¿~¦È wX¶ãÌzXÜJHÿUBßÌÚh;sû¿®C?N+±àa³-ÑÑy¡Ù[~½*ÃøbT|Çv÷AD(µ=jNq'ë«Üð ñ ÃKn:¥Å*@ößêwŨ³;A!òíó9öär5²mr¬|$¨zFè`Ã$&Ò{+M¨/gàvxкË|AüØËùÅ»m?Nâa²ÝÐ"PoAÇP8¯©ëzÕÐku+|±>f¿ªÏ.q.CúÌÚÃJV,å¹5ù×-CFÔuM=-ìn.nc8ÝRÀëâïfó-8KFBÚXËeÒäÊZ&£ÉLs<ñ|=Agg¿àrX'ë!Ǥ¼þR]#éßñPòVQú³"|ÚC%ó!õ µ¸äø!"xVA¹C¿Ëý¬¸rAPÚ*z It`:`ºZ´-3-½½º¤<L´«Gìÿ.äiy:ÓL*F«ÉÇÙ}ÏóS&Cy·æ0â¦Z#7ùgàaËQ©Ö¡CXÿÔê°ù?È×zj¶öM2Eë¡ÝIB¼¾É4éGJEEy§@Òοqé¼½#¿¦´ü3UªÔçj1¸ÿ9ÎÓàÅ()z»ÔÒáCĶÚÆ.vû=ëCmfÚà
§|)2M4ß/ê÷ñLKG£HhHñËãEÇ¢1óoRòÆ£dD¬X þñ*h|¥FHã1a"·µ¸1;x|'+
RÇKÔ~°¯è=+âñÉVJ¤tXNÇÜP¨~²&É©âÀ~¬[ý§)Úß2OëÂoê*v1áðÝsè6¡xéÔk%X¦§ }^V2FÎ@â1d¶ü^þoÑïèÏ@«!@ûW²øl¾2y5zsy44]Oò]T°çé'¥®ýÐÉñqxãáqægÕ+òÛ_¸ZÜ-µÌ¼ÏûÄX@ê׿@ÊdòZwåõÝ
íôRgk¸f0Drjâøä6þl®#vÁ|4Yoä^«¾VÍim.dYS¸ÒEÿfT¤ÕLó_ô?`áÒÄs@HámÚ3Ñ·1ª¢è:|H¡*Ôí!mR! ;1¤¢¡2Ä8ZM¾À¹ÉIáÞhWó>¥ëyë¶þÔái"Ç KçÝSØæAAÿÕë¾ToWÉv15¨}S®fä;óh½Ø.½|_̺³ðÛ´éDDeFÒ_ÒrV©©ØüÆDPYËÇRNXÒKw<P<duSò'|ÇÍ:³lýt9L<ÁéVoëK·ØéñLÛ )½hÿNgipØâ.«5zBkÅhAÌÒ+GE8n~ã±È¤IÒZ,^îÑFbdÁÜåâÔt((õ^ÝFb¹vÅ#W«yÝð¡ -}CC¾*¤Õ¿Ómû}تÉ)Z{ãhPâÝE¾¥VO^ǪÁXAARK´ØpsݧL*ÄõÍ[pexÑ£ý6&¿êSL3QX` ^p(Q6¯~ äÁ¾¬àcÔ%:ÝÖ©$QXS'ð·*²Ût(Þ°ÓËK-y4õVK]AD+PÕ¬M¿^,J³Ì¸j£!G
G(ÙÕªRM.CÝ8ÄfXäáucdý¡¸ú2Ðæ}EØ8û²Â«¾PÜÀÅô øPäaÍ2;#n8â<æãaÓ®Jex÷æ% ÍLê(.-áò·Sÿpóc+óÌ¢ÒÿÖ](https://www.ecuhealth.org/wp-content/uploads/2023/10/12-Edit.jpg)
By North Carolina Health Care Association
North Carolina’s hospitals and health systems provide more than just healthcare services. They also blend medical know-how with community engagement and technology to help prevent and manage chronic conditions and to address factors affecting health like access to healthy food and transportation. Learn how health systems and hospitals work with local employers, schools, faith organizations and other partners to build healthier, vibrant communities.
Five rural healthcare leaders from across the state recently came together for a virtual town hall to discuss how their hospitals and health systems are creating healthier communities. This program is part of a series hosted by the North Carolina Healthcare Association.
Here are some key takeaways from the conversation.
Hospitals help support the livelihood of rural communities.
Hospitals are pillars in their communities and support economic development by providing education and employment opportunities that create stronger, more resilient citizens. “Our approach here at Northern Regional Hospital is to be engaged in all areas of community life. We recognize, like most hospitals, that we are the largest employer in the city of Mount Airy and one of the largest in the region,” said Chris Lumsden, President and CEO of Northern Regional Hospital. Lumsden emphasized that hospitals engage in a mutually beneficial relationship with the surrounding community. “If the hospital is healthy, the community [members] in a rural community will be healthy, and vice versa.”
Penney Burlingame Deal, President and CEO of Onslow Memorial Hospital, also touched on the relationship that hospitals share with their community. “In rural settings, hospitals play a part in community resilience,” expressed Burlingame Deal. Communities can support and sustain quality health and social services by attracting and retaining well trained healthcare professionals. This can then lead to a stronger economy, which in turn supports a stronger local healthcare system. “It’s recognition of that link between rural healthcare, economic strength, and overall vitality…it’s kind of this self-perpetuating feedback loop.”
John Green, President and CEO of Iredell Health System discussed how every hospital and health system is driven by a mission and vision statement, and while each is different, they all guide people towards optimal health. More importantly, this is not always done within the four walls of the hospital. Often times, hospitals are working outside of their brick-and-mortar establishments – directly in the communities they serve – to accomplish their goals. “We do that throughout the whole community, and we do it based on the needs of each part of that community,” said Green.
To that point, Annie Carpenter, Assistant Vice President of Community Engagement at Mission Health added, “We go beyond the hospital walls with our community approaches, and not just because we serve the community, but because we are the community.”
Hospitals invest in their communities to address the unique and diverse challenges they face.
Every community is unique, so it is important that hospitals listen to the needs of their community members when developing programs and initiatives. Patrick Woodie, President and CEO of the NC Rural Center, and the moderator of this conversation, shared a saying from his years of work in rural health, “when you’ve seen one rural community, you’ve seen one rural community.” This underscores that each community is characterized by its distinct array of challenges, and they must be addressed in their own unique ways.
Todd Hickey, Chief Strategy Officer of ECU Health mentioned how ECU Health is always assessing how they can invest back into the community. They do this by donating funds to support community partners, developing initiatives aimed at improving health, and through other avenues. “We see that as a role of a good steward of healthcare in a community, but also recognizing that it’s our partnerships that really connect our services to our patients, and if you will, our population,” said Hickey.
Hospitals also play a big role in strengthening the local workforce. Chris Lumsden noted that 85 percent of Northern Regional Hospital’s employees were raised and live within a 25-mile radius of the hospital. In addition, 85 percent of high school students that leave this area for work or college, do not return. “The message is, we have to grow our own. And that’s a theme that we have created through education assistance scholarship programs,” expressed Lumsden. To combat this, Northern Regional Hospital has stood up multiple programs that encourage students to not only pursue careers in healthcare, but to also stay and serve in their community.
Hospitals in rural communities use innovation to expand their reach and build more accessible health care.
Hospitals and health systems in rural communities are evolving with the changing landscape of health care. They are overcoming barriers to care and expanding access to care through innovative solutions, emphasizing a focus on maintaining good health for all.
Telehealth has blossomed as an accessible option to care, but internet connection can be sparse in some rural communities and hospitals are creating solutions to bridge the gap. “Working with our civic partners, counties and townships, trying to build out and create the funding through grants, through alignment of federal funding to help expand that [broadband] is a big deal,” said Todd Hickey. Hickey connects the availability to broadband with a greater opportunity for people in rural communities to get preventative care and early intervention for serious conditions.
Related to telehealth, Penney Burlingame-Deal said, “it is a great way of really thinking outside of the box and using innovation to make things happen that wouldn’t happen otherwise”. In addition, John Green touched on a need for stable internet access in all rural communities and technology training, especially for aging populations, highlighting the digital-based resources that will lead the future of health care.
Care options combatting opioid addiction are expanding and improving as well. Annie Carpenter mentioned a pilot program newly introduced to Blue Ridge Regional Hospital and Mission Hospital, where patients can receive medication-assisted treatment within the emergency department, an effective evidence-based practice to disrupt the addiction cycle. According to Carpenter, this care approach can impact the capacity and volume the health system while combatting the rise in opioid overdoses in the region.
“The community has been working together on responses at such a rapid rate to save lives. [The pilot] It’s something our partners in the community have been eager to see as well,” said Carpenter.
Launching more impactful programs that promote better health within rural communities often requires research and advocacy to accelerate the implementation of those programs. John Green mentioned at smaller rural hospitals, a detailed approach is necessary to implement new ideas in order to make the most of time and funding. It may be more difficult to find an effective solution using a trial-and-error approach. To advance new initiatives and programs, hospitals may glean successful ideas from other hospitals in areas with similar populations in communities with similar challenges, implementing what worked in the pilot program as a potential solution for their own community.
“I think research that allows us to see this is going to work, or we believe this should work is a huge difference to us,” said John Green.




