The Teachers of Quality Academy (TQA) at the Brody School of Medicine at East Carolina University and ECU Health officially welcomed its 9.0 cohort at its first learning session on Sept. 18.
For the newest group of multidisciplinary health care professionals in the program, the first lesson is perhaps the most important: system-wide quality improvement starts small before it can grow into something big.
“One of the hallmarks of this learning experience is that you have your small team and then it gets a little bit bigger over time,” said Dr. Jennifer Sutter, TQA physician director. “One of our speakers today talked about how the big system is only as good as the little systems. So, we have to achieve quality first at a microsystem level before it can make a big system much better. That theme is really the ideal way to kick-off what these participants will learn over the next year.”

Through the TQA 9.0 program, health care leaders will learn how to fundamentally change care delivery through a curriculum focused on building knowledge and skills in Health Systems Science which comprehensively explores how health care is delivered. Participants engage in advanced learning in quality improvement, patient safety and team leadership, develop improvement projects to apply these skills across the health system, teach others in their environment about these concepts, and evaluate the outcomes of improvement interventions. Leading by example, TQA participants promote a culture of quality and safety across the enterprise.
Dr. Andre Mancheno is a second-year resident in ECU Health’s Rural Family Medicine Residency program. His TQA project group includes two fellow residents in the Rural Family Medicine Residency program, all of whom are currently learning and serving in Duplin County. For Dr. Mancheno and his colleagues, the program provides them an opportunity to explore opportunities to improve on real-world scenarios they experience.
“We’re interested in doing something to improve our clinic,” Dr. Mancheno said. “Since our clinic is rural, there are limited resources, limited staffing. There are a lot of challenges to overcome, and this program can help us find solutions. The skills we apply to improving quality are also applicable to all things in health care.”
With 37 learners in TQA 9.0, participants spent their first learning session gaining invaluable knowledge about quality improvement, the role it plays in high-quality care and the impact it has on ECU Health’s mission to improve the health and well-being of eastern North Carolina. The newest cohort includes health care professionals from clinical, administrative, leadership and educational backgrounds, all of whom were selected from a highly competitive pool of applicants. And, for the first time ever, pastoral care team members are part of the program, underscoring how quality goes far beyond purely clinical experts.
The lessons also have the potential to extend directly into communities across eastern North Carolina. Dr. Kristina Simeonsson, associate professor in Pediatrics and Public Health and Hannah Dail-Barnett, research associate, help lead the Healthier Lives at School and Beyond initiative created by the Brody School of Medicine and ECU Health.
The program originally launched in 2018 to deliver interdisciplinary services virtually to rural school children, staff and faculty during the school day.
In response to COVID-19, the program continued to address health care needs for children and expanded access while students were learning remotely.
Since the fall of 2020, the program has used an ECU Transit bus to visit schools in Duplin, Jones and Sampson counties to provide high-quality health appointments. The retrofitted motorcoach has been used to provide screenings for hundreds of students.
Like Dr. Mancheno and his fellow rural residents, Dr. Simeonsson and Dail-Barnett appreciate the opportunity to apply quality lessons directly to the patients and students they serve.

“As a program evaluator for Healthier Lives at School and Beyond, we’re always considering how to achieve continuous quality improvement in our program,” said Dail-Barnett. “How can we improve our reach in these communities, help improve access to health care services and increase efficiency and timeliness of services to these students? We’re hoping to use TQA as a catalyst for further quality improvement to continue to expand our services and help reach these hard-to-reach populations.”
Dail-Barnett described the entire TQA group as having “lofty goals” and “really big dreams.” According to Dr. Simeonsson, therein lies the challenge of the day’s most important lesson.
“That’s going to be the challenge – keeping it small to begin with,” Dr. Simeonsson said. “We’re all coming in here with ideas and a lot of passion and our instructors are reminding us to tap the brakes. The best thing from today was the reminder that we’re here to learn the process. Let’s learn the process and then continue to build as we go forward. And we know that can have a big impact because there are so many alumni that come back and tell us how their projects are going three years later.”
Roanoke Rapids, NC – ECU Health is proud to recognize Hubert Allen as the first patient to complete 60 hyperbaric oxygen treatments at the ECU Health Wound Healing Center in Roanoke Rapids. His journey represents a powerful testament to the importance of having high-quality care close to home, particularly for those needing advanced wound care.
Allen arrived at the center on May 1, 2025, facing life-altering complications from a radiation injury. He was wheelchair-bound, frequently hospitalized, disoriented and unable to drive—his independence and quality of life severely impacted. But with the expert care of medical director Dr. Jamie Udwadia, nurse practitioner Ashley Duke, manager of Patient Care Services Jennifer Millius, and the entire Wound Healing Center team, Allen’s condition began to improve dramatically.
“Hyperbaric oxygen therapy restores at the cellular level,” said Dr. Udwadia. “Hubert’s radiation injury was slowing his healing, but today, his recovery is a testament to the power of modern medicine and personal resilience. The fact that he could receive this level of care close to home underscores how vital it is to make advanced therapies accessible close to home for our own communities.”

Allen underwent 60 hyperbaric oxygen treatments, which is a specialized treatment that enhances the body’s natural healing processes by delivering high concentrations of oxygen in a pressurized environment. It is particularly effective for patients with chronic wounds, radiation injuries, and other complex conditions. Over the course of his treatments, Allen experienced a remarkable transformation. Today, he is walking, driving, and reconnecting with the life he once knew.
“The ECU Health Wound Healing Center team was extremely compassionate and supportive during my treatments,” said Allen.
Allen’s recovery not only marks a personal milestone but also underscores ECU Health North’s commitment to providing innovative, patient-centered care to communities across eastern North Carolina. His story serves as an inspiration to others facing similar challenges and a reminder of the profound impact compassionate care can have on a patient’s journey.
Greenville, N.C. – The American Heart Association/American Stroke Association has awarded all nine ECU Health hospitals Get With The Guidelines ® achievement awards for demonstrating commitment to following up-to-date, research-based guidelines for the treatment of heart disease, stroke and diabetes, ultimately leading to more lives saved, shorter recovery times and fewer readmissions to the hospital.
“At ECU Health, delivering high-quality, life-saving rural health care is central to our mission of improving the health and well-being of eastern North Carolina,” said Brian Floyd, chief operating officer, ECU Health. “Our team members represent that mission in action and we could not be prouder that all nine ECU Health hospitals have once again earned national recognition in improving outcomes for patients facing stroke, heart disease and diabetes–conditions that deeply impact our region. This achievement reinforces ECU Health’s commitment to ensuring high-quality health care is available in our rural region.”

Heart disease and stroke remain among the deadliest health threats in the United States, ranking first and fifth, respectively, according to the American Heart Association 2025 Statistical Update. Every 40 seconds, someone in the U.S. suffers a stroke, adding up to nearly 795,000 new or recurrent cases each year. Tragically, stroke claims about 140,000 lives annually. Eastern North Carolina bears an even heavier burden, with stroke mortality rates exceeding national averages. The region also grapples with disproportionately high rates of diabetes and cardiovascular disease, highlighting the importance of targeted prevention and timely intervention.
“In eastern North Carolina, where stroke, diabetes and heart disease rates are disproportionately high, delivering high-quality care close to home is not just important – it’s vital,” said Dr. Niti Armistead, chief quality officer and chief clinical officer, ECU Health. “By adopting evidence-based practices and programs like Get With The Guidelines, our teams deliver consistent, highly reliable care that improves recovery and health outcomes. These recognitions affirm our steadfast commitment to clinical excellence and continuous improvement in all that we do.”
Evidence shows that patients fare significantly better when health care providers follow established treatment protocols, such as those outlined in the Get With The Guidelines program. Consistent adherence to these evidence-based practices leads to improved recovery outcomes and can help reduce the devastating impact of stroke and heart disease.
“These awards show ECU Health’s commitment to caring for those in their community who need care,” said Donald Lloyd-Jones, past volunteer president of the American Heart Association and current volunteer chair of the Association’s Quality Oversight Committee. “By following the American Heart Association’s quality improvement protocols, ECU Health can help realize our shared vision of improved patient outcomes, fewer readmissions and lower mortality rates — a win for health care systems, families and communities.”
ECU Health recognitions include:
ECU Health Beaufort Hospital – A Campus of ECU Health Medical Center
- Get With The Guidelines – Stroke Gold Plus with Target: Type 2 Diabetes Honor Roll
- Get With The Guidelines – Rural Stroke Gold
- Get With The Guidelines – Coronary Artery Disease STEMI Referring Center Bronze
- Get With The Guidelines – Resuscitation Bronze
- Get With The Guidelines – Rural Coronary Artery Disease STEMI Gold
ECU Health Bertie Hospital
- Get With The Guidelines – Coronary Artery Disease STEMI Referring Center Bronze
- Get With The Guidelines – Rural Stroke Silver
- Get With The Guidelines – Stroke Silver Plus
- Get With The Guidelines – Rural Coronary Artery Disease STEMI Silver
ECU Health Chowan Hospital
- Get With The Guidelines – Coronary Artery Disease STEMI Referring Center Bronze
- Get With The Guidelines – Rural Stroke Silver
- Get With The Guidelines – Stroke Silver Plus with Target: Stroke Honor Roll and Type 2 Diabetes Honor Roll
- Get With The Guidelines – Rural Coronary Artery Disease STEMI Gold
ECU Health Duplin Hospital
- Get With The Guidelines – Rural Coronary Artery Disease STEMI Gold
- Get With The Guidelines – Stroke Gold Plus with Target: Type 2 Diabetes Honor Roll and Stroke Honor Roll
- Get With The Guidelines – Stroke Rural Gold
ECU Health Edgecombe Hospital
- Get With The Guidelines – Rural Coronary Artery Disease STEMI Silver
- Get With The Guidelines – Rural Stroke Silver
- Get With The Guidelines – Stroke Gold Plus with Target: Type 2 Diabetes Honor Roll and Stroke Honor Roll
- Get With The Guidelines – Coronary Artery Disease STEMI Referring Center Silver
ECU Health Medical Center
- American Heart Association Commitment to Quality Award
- Get With The Guidelines – Resuscitation Adult Bronze
- Get With The Guidelines – Resuscitation Pediatric Gold
- Get With The Guidelines – Resuscitation Neonate/Infant Gold
- Get With The Guidelines – Resuscitation Newly Born Bronze
- Get With The Guidelines – Stroke Gold Plus with Target: Stroke Honor Roll
- Elite Plus, Stroke Advanced Therapy and Type 2 Diabetes Honor Roll
- Get With The Guidelines – Coronary Artery Disease STEMI Receiving Center Gold with Target: Type 2 Diabetes Honor Roll
- Get With The Guidelines – Coronary Artery Disease NSTEMI Gold with Target: Type 2 Diabetes Honor Roll
ECU Health North Hospital
- Get With The Guidelines – Rural Stroke Silver
- Get With The Guidelines – Stroke Bronze
- Get With The Guidelines – Coronary Artery Disease STEMI Referring Center Silver
- Get With The Guidelines – Rural Coronary Artery Disease STEMI Gold
ECU Health Roanoke-Chowan Hospital
- Get With The Guidelines – Coronary Artery Disease STEMI Referring Center Bronze
- Get With The Guidelines – Rural Stroke Gold
- Get With The Guidelines – Rural Coronary Artery Disease STEMI Gold
Outer Banks Health Hospital
- Get With The Guidelines – Stroke Gold Plus with Target: Type 2 Diabetes Honor Roll
- Get With The Guidelines – Rural Stroke Gold
- Get With The Guidelines – Coronary Artery Disease STEMI Referring Center Silver Plus
- Get With The Guidelines – Rural Coronary Artery Disease STEMI Silver
NAGS HEAD, N.C. — September 19, 2025 — Outer Banks Health announces it has been recognized as a top performer in the 2025 Bernard A. Birnbaum, MD, Quality Leadership Ranking by Vizient, Inc. Outer Banks Health (OBH) placed tenth amongst 1,400 Vizient provider clients in the critical access cohort and was recognized for demonstrating excellence in delivering high-quality care based on the Vizient Quality and Accountability Study, conducted annually since 2005.
“We are tremendously proud of our entire team for their exceptional commitment to safe, effective and compassionate patient care for our community. OBH is honored to be recognized for these efforts,” said Ronnie Sloan, president of OBH. “Special recognition goes to Devereux Grindle, vice president of clinical operations and former director of clinical quality management, for establishing and building a strong quality department, as well as to Stefanie McMahon, director of clinical quality management, for her outstanding leadership today.”
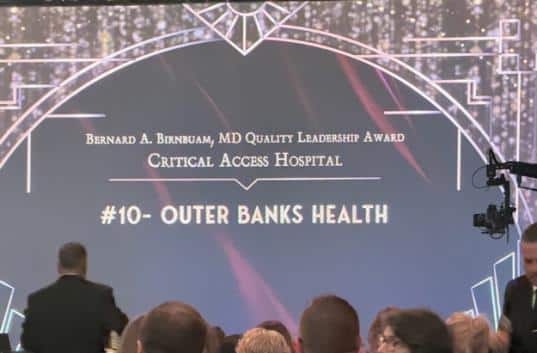
This year, 1,220 participating hospitals were segmented into seven cohorts for the Vizient Quality and Accountability Study. The study measures performance on the quality of patient care in six domains: safety, mortality, effectiveness, efficiency, patient centeredness and variation in care. The study factors in measures from the Vizient Clinical Data Base and includes performance data from the Hospital Consumer Assessment of Healthcare Providers and Systems survey and the CDC’s National Healthcare Safety Network.
The Vizient Quality and Accountability Study helps participating hospitals and health systems understand their performance against their peers and identifies structures and processes associated with high performance in quality and safety across a broad spectrum of patient care activity. The recognition period is for work spanning July 1, 2024 through June 30, 2025.
“We extend our sincere congratulations to this year’s top-performing hospitals recognized in the Vizient Quality and Accountability Study,” said David Levine, chief medical officer, Vizient. “These organizations have demonstrated an exceptional commitment to delivering safe, effective, and patient-centered care. Their performance reflects the highest standards in clinical quality and operational excellence, and we are proud to honor their achievements.”
To be a health care provider is to answer a calling. For some, the journey to health care is a straight line; for others, the road is winding. This series features stories from ECU Health team members who took the winding road, but found the destination to be worth the effort.
Karen Bolen, the director of inpatient clinical applications in the IS department of ECU Health, knew in high school that she wanted to be a nurse. After graduation, the West Virginia native worked as a bedside nurse and charge nurse in the emergency departments (ED) of several hospitals in West Virgina and Kentucky, and she also served as the manager of an ED. In early 2000, however, she had the opportunity to beta test an electronic health record (EHR) platform specific for the ED. That experience, which she thought was “really cool,” led Karen from the bedside to the world of health care information technology.
Seven years after that initial beta test, Karen’s organization announced their plans to adopt their own EHR. Her earlier experience with the software inspired her to inquire about transitioning from the bedside to working with the platform. “I was intrigued by the EHR, and as a new mom, working nights and on weekends didn’t do well for me. I asked about it, and I moved over to my new role in 2007,” she said. “I quickly realized this is where I wanted to be.”
Making this transition allowed Karen to leverage her education and extensive knowledge of the ED with building an effective and efficient EHR platform. “They were looking for nurses to build this EHR, which was Epic. I have a bachelor’s degree in nursing, and I use that every single day with what I do,” she said. “Because I had worked for many, many years in the ED, they chose me to build out the platform for the department.”
Working within electronic health records also merged Karen’s skillset as a nurse with her overarching desire to do good for the most people. “It was great because I could not only impact patients at the bedside, but I also impacted all the clinicians taking care of the patients, all of the ancillary departments and the community as well,” she explained. “I put my stethoscope down and picked up a laptop, but I didn’t lose anything by doing that. I still care for patients, and this enhances what I went to school for and what my passion is. I just do it in a different way.”
That training as a nurse was vital to creating the platform, but she also had to take classes specific to the EHR. “I knew how to save a life, I knew how to give medications and I knew how to provide education, but I didn’t know how to build an electronic health record. To do that, I took training classes, completed a project and passed a test. I also had to be certified in several different areas to complement my role as an application analyst,” she explained.
Karen relocated to ECU Health in 2017, where she joined a team that feels like a perfect fit. “They are the most amazing team ever,” she said. “I can wholeheartedly say that. They serve anything that falls within the halls of the hospital. We support not only the electronic health record, but also all the technologies that integrate with Epic, including fetal monitoring and the handheld rover application for on-the-go documentation. We have the most talented application analysts on our team.”
Karen is also responsible for supporting the ED, OR, anesthesia, pharmacy and ambulatory surgery. “I have an amazing team and great managers who supports those areas,” she said. “They teach me something new every single day. That’s one of the fun things about this role.”
That enthusiasm makes it easy for Karen to recommend a role in health care – whether it’s at the bedside or at the computer – to anyone. “When I was a beside nurse in the ED, I told people I had the coolest job ever. Now that I work in IS, I still have the coolest job ever,” Karen said. She also emphasized that anyone can work in the technology space. “We have people with a variety of backgrounds in our department. We have pharmacists, engineers, nurses and respiratory therapists. That diversity really complements those with information technology degrees and allows us to collaborate and share different perspectives and experiences to do something great. IT is in everything, and everything we do makes an impact.”

The Great 100 Nurses in North Carolina honors nurses around the state for their commitment to excellence. The recipients are distinguished for their outstanding professional ability and contributions to improving health care services in their communities. This year, 25 ECU Health nurses were honored, including Anne Chadwick, Robin Lanier, Sharon Watford, Gloria Waters, Lindsey Woodlief, April Bracy and Claire McFadyen.
Anne Chadwick

Anne Chadwick, a staff nurse IV in the medical step down unit, joined what was then Pitt County Memorial Hospital in 1982 after graduating with her degree in nursing. She didn’t know if nursing would be a good fit, but despite a retirement in 2013, she came back to work at the bedside, and she’s also an adjunct nursing instructor at Pitt Community College. “I have had absolutely no regrets – I love it!”
Anne joined ECU Health after completing her degree at ECU, but proximity wasn’t the only reason. “I like working here,” she said. “I’m proud of our facility. I’ve worked in different roles, and I’ve never felt stagnant or burnt out.”
Despite her passion, Anne was still surprised when she found out she was a Great 100 Nurse. “I was thrilled and appreciative that they wanted to nominate me,” she said. “I’ve known others who were nominated and didn’t get it, so I thought there was no way I’d get it.”
As for why she was nominated, Anne said, “I don’t really know,” but she recalled taking more than one student when a student needed a preceptor, and she once comforted a patient’s husband in the hallway after he made a difficult health care decision for his wife. “He grabbed me and I just hugged him and let him cry,” she recalled. “I don’t know if it’s that, but I try to have compassion for our patients.”
Robin Lanier (Ellis)
 Robin Lanier, an assistant manager of nursing in the medical unit at ECU Health Edgecombe Hospital, was born and raised in Tarboro, and it was her mother and a teacher at Tarboro High School who gave Robin the idea to become a nurse.
Robin Lanier, an assistant manager of nursing in the medical unit at ECU Health Edgecombe Hospital, was born and raised in Tarboro, and it was her mother and a teacher at Tarboro High School who gave Robin the idea to become a nurse.
“From my mom’s perspective, nursing offered stability. I’d never have to worry about finding a job,” Robin said. “Ms. Wainwright taught medical terminology in high school and she was my favorite teacher. Being in her class really made me choose the nursing path.”
Robin joined ECU Health in 2013, and although she chose Edgecombe Hospital because it was close to home, she stays because it feels like home. “The friendships I’ve made, the support I’ve received – it’s nice to be seen and get to know people on a personal level. You get close and support each other when life happens,” she said.
Funny enough, Robin nominated one of her colleagues as a Great 100 Nurse, so when she got the letter in the mail, she thought it was about the nominee winning the award. “I was so excited for her, and then I saw it was me who had won,” she said. “I was happy for me, but I really wanted her to win. There are so many who really deserve to be recognized.”
Winning was a surprise, but Robin said she hopes it’s a sign of her desire to help others. “I try to take the time to make people feel special, because they are,” she said. “If there’s something I can do that will make someone’s day better, I try to do it. It’s important to me that people are taken care of – our patients and our team members.”
Sharon Watford
 Sharon Watford joined what was then Pitt County Memorial Hospital in 1988, and she has worked in several departments over the last 36 years, including the medical surgical unit and the operating room. She currently serves as a staff nurse IV in a pain management outpatient clinic.
Sharon Watford joined what was then Pitt County Memorial Hospital in 1988, and she has worked in several departments over the last 36 years, including the medical surgical unit and the operating room. She currently serves as a staff nurse IV in a pain management outpatient clinic.
While Sharon said she landed on nursing as a career somewhat accidentally, during nursing school, her mother was diagnosed with kidney failure secondary to lupus, and she spent a lot of time with her mother in the hospital. “That solidified that I was doing what I was supposed to do,” she said.
She was “floored” when she discovered she was a Great 100 Nurse this year. “That’s the ultimate of nursing honors,” she said. “I have admired those who received it, and I didn’t think I’d ever get it.”
Still, Sharon shared that she aims to make a connection with each of her patients. “Our clinic is fast paced, and I try to maximize my time with patients so they don’t feel like they’re in a drive through,” she said. “I’m committed to this profession and to ECU Health, and I love my work.”
It’s special that 25 nurses from ECU Health are being recognized this year, something Sharon said represents the dedication of our nurses. “Our people go above and beyond; that’s what we’re called to do,” she said. “We care for the whole patient and meet their needs.”
Gloria Waters
 Gloria Waters knew from an early age she wanted to be a nurse. “My mom made me a nurse’s cap out of notebook paper, a black crayon to draw the stripe across the top and a bobby pin to secure it to my head,” Gloria recalled. “She’d put a sweater over my shoulders and I’d pretend to be a nurse.”
Gloria Waters knew from an early age she wanted to be a nurse. “My mom made me a nurse’s cap out of notebook paper, a black crayon to draw the stripe across the top and a bobby pin to secure it to my head,” Gloria recalled. “She’d put a sweater over my shoulders and I’d pretend to be a nurse.”
Gloria attended Lenoir Memorial Hospital School of Nursing right out of high school, and her parents encouraged her while she studied. “I remember them sitting at the table with me and helping me study. I told them about the cardiovascular system and how the heart has four chambers, and dad said, ‘just like a carburetor in a car!’ They were always there for me.”
Gloria came to ECU Health Medical Center because as a larger hospital, it offered the opportunity to grow in her profession. “I learned and practiced skills I’d never had a chance to do at my previous job,” she said. “I was given the opportunity to grow and get more experience.”
That, and the people she works with, has kept her here for 22 years. “The floor is like a family. Even with the growth of the hospital, the atmosphere is a good one. We have some pretty amazing people who work here.”
Of winning the award, Gloria said she was honored just to be nominated. “I’m appreciative someone thought I was deserving,” she said. “I do what I do because I love it. People ask when I plan to retire, and I don’t know. I have no plans to retire because I’ll miss the people and doing something I have always loved.”
Lindsey Woodlief
 From a nursing assistant to a doctor of nursing practice, Lindsey Woodlief has grown professionally and personally at ECU Health. She joined ECU Health Edgecombe Hospital in 2014, and through the HomeGrown Program, she graduated with her associate’s degree in nursing (ADN) in 2019. As a recent doctor of nursing practice (DNP) graduate, she will now serve as a family nurse practitioner at ECU Health Family Medicine in Pinetops, NC. “My journey reflects a deep commitment to lifelong learning, compassionate care and service to my community,” she said.
From a nursing assistant to a doctor of nursing practice, Lindsey Woodlief has grown professionally and personally at ECU Health. She joined ECU Health Edgecombe Hospital in 2014, and through the HomeGrown Program, she graduated with her associate’s degree in nursing (ADN) in 2019. As a recent doctor of nursing practice (DNP) graduate, she will now serve as a family nurse practitioner at ECU Health Family Medicine in Pinetops, NC. “My journey reflects a deep commitment to lifelong learning, compassionate care and service to my community,” she said.
From an early age, Lindsey witnessed her family emulate selflessness and compassion. Her mother taught students with special needs, and her grandmother, also a nurse, served as an inspiration. Her uncle became a quadriplegic after a hunting accident at 18, so Lindsey saw the importance of caring for others.
At ECU Health Edgecombe, Lindsey said she built her forever home and felt grounded in her community. That proximity, as well as the close-knit team she works with, has kept her here. “Working at a small community hospital has given me something special,” she said. “I’ve formed lasting friendships with co-workers and community members, and in our intensive care unit (ICU), we are more than a team; we’re a family.”
While there are other awards nurses can receive, the Great 100 Nurse award means more than clinical success. “This award reflects countless hours, effort, integrity and heart that nurses pour into their patients and communities every day. We are driven by the desire to make a meaningful difference,” she said.
It’s also no surprise to her that ECU Health represents a quarter of the Great 100 Nurses this year. “It’s a reflection of the culture and mission that drive everything we do,” she said. “At ECU Health, what sets us apart is how deeply our system lives out its values. We’re not just committed to delivering high-quality care; we are equally invested in the growth, education and well-being of our team members and the communities we serve.”
“You may have heard the saying, ‘not my monkey, not my circus,’” she continued. “But anyone who knows me knows I tend to make everything my monkey and circus.” Lindsey said she doesn’t seek praise, but she tries to show up with a full heart for her patients and her team. “I’m the nurse you can call on her day off and talk you through a task, the one who will show up at 2 a.m. to help the unit, bed hair and all, and the one who’s at every community event,” she said. “To me, being a nurse doesn’t end when I clock out.”
April Bracy
 April Bracy, an assistant manager in the cardiovascular intensive care unit (CVIU), has been an ECU Health team member for almost 16 years. She began working in the ED at ECU Health Roanoke-Chowan Hospital before moving to ECU Health Bertie’s ED and inpatient unit, followed by a transfer to the Medical Center where she worked in palliative care and now the CVIU.
April Bracy, an assistant manager in the cardiovascular intensive care unit (CVIU), has been an ECU Health team member for almost 16 years. She began working in the ED at ECU Health Roanoke-Chowan Hospital before moving to ECU Health Bertie’s ED and inpatient unit, followed by a transfer to the Medical Center where she worked in palliative care and now the CVIU.
April said she was inspired to work in health care by her family. They called her their “little nurse,” because she liked to help them when they were sick. While she had the initial desire to be a surgeon, her mother was the person who inspired her to pursue nursing. “She explained that there were numerous fields I could try until I found the specialty that fit and made me happy,” she said.
She joined ECU Health, despite other hospitals being closer to her home, because it offered more opportunities, especially the chance to grow and learn. Now, as a Great 100 Nurse, April said she is humbled and honored, and she is proud to be among so many exceptionally great nurses.
Claire McFadyen
 A third-generation nurse to serve eastern North Carolina, Claire McFadyen has worked at ECU Health for 17 years. Her grandmother was a CRNA at what was then Pitt County Memorial Hospital, and her mother retired as an operating room nurse at ECU Health Edgecombe. Now, Clair is continuing her family’s legacy as a staff nurse IV in ECU Health Edgecombe Hospital’s ICU.
A third-generation nurse to serve eastern North Carolina, Claire McFadyen has worked at ECU Health for 17 years. Her grandmother was a CRNA at what was then Pitt County Memorial Hospital, and her mother retired as an operating room nurse at ECU Health Edgecombe. Now, Clair is continuing her family’s legacy as a staff nurse IV in ECU Health Edgecombe Hospital’s ICU.
Claire said she was drawn to ECU Health in part because of her family connection, but also because she wanted to serve where she lives. “I always maintain an active role in the local community, attending and hosting events for education and resources for adults and the younger population, as well as precepting new nursing entering the field of critical care,” she said.
It’s an honor to be recognized as a Great 100 Nurse, and Claire said she is grateful and humbled to be listed among her ECU Health team. She also hopes the award is a reflection of her persistent passion for nursing at the bedside. “The impact of bedside nursing on quality health care is sometimes understated,” she said. “I try to instill my love for the profession and critical care in every patient I treat and in every student or new graduate I encounter.”
The recipients will be honored at a statewide gala in October, to be held in Goldsboro, North Carolina.
A local initiative is helping residents rethink how they shop for food. The Penny Pinchers Health Grocery Store Tours, led by the Pitt Partners for Health Coalition, shows that healthy eating does not have to be expensive. Through hands-on grocery store tours and practical budgeting strategies, the program equips participants with the tools to make healthier choices without overspending.
Healthy eating is crucial to long-term well-being, helping to prevent chronic diseases like obesity, diabetes and heart conditions. While cost is often seen as a barrier, nutritious diets can be affordable with smart planning. According to the Pew Research Center, roughly 70 percent of Americans say the increased cost of healthy food in recent years has made it more difficult to eat healthy.
Despite rising food prices, making informed choices and cooking at home can dramatically reduce expenses while boosting health, according to Qua’Tavia White, community health improvement coordinator at ECU Health.

Founded through the long-standing Pitt Partners for Health Coalition, the Penny Pinchers Program is powered by a grant from The Duke Endowment’s “Healthy People, Healthy Carolinas” initiative. While ECU Health Medical Center is one of the coalition’s organizations, the program itself is community-led, with volunteers from across Pitt County driving its success.
“This is a coalition effort,” said White. “We have partners from all over the county helping lead it and we are grateful to our local Food Lions for allowing us to host this program at their stores.”
At the heart of Penny Pinchers is the $15 challenge, a hands-on grocery store tour designed to teach participants how to shop smart and eat healthily on a tight budget. Led by volunteers like De’Vette Thomas, a community health improvement manager at ECU Health, the tours take place at rotating Food Lion locations across Pitt County.
Each session begins with a brief orientation followed by a guided walk through the store. Participants learn how to use unit pricing to compare products, read nutrition labels, identify healthier options using Food Lion’s Guiding Stars system and understand the value of frozen, canned and fresh produce. After the educational portion, participants are given a $15 gift card and challenged to build a complete, healthy meal.
“The rules are to stay under budget and include at least three of four key components: a healthy protein, grain, fruit, dairy, and vegetable,” said Thomas. “Deli meats and processed items like bacon are off-limits for the challenge due to them not having any Guiding Stars and being high in sodium and fat. Participants are encouraged to eat from this food group less often. We want people to know they can eat healthily and still not spend a lot of money. It’s about teaching them how to get the most bang for their buck.”
Tours typically host 10-13 participants, with special sessions tailored for groups like public health students, senior clubs or the Diabetes Prevention Program at the Pitt County Health Dept. The program runs at least once a month, sometimes twice, depending on community demand.
Feedback has been overwhelmingly positive. Participants often share photos of their meals and complete pre and post surveys to help organizers measure impact. One participant, Lydia Best, described her experience as “fantastic.”
“I enjoyed meeting the other people who were there as well as all the information we were given,” said Best. “I had never noticed those stars at Food Lion for how to shop in a healthier fashion. We shared so much information between each other. It was fabulous.”
Best recalled the challenge of creating a balanced meal with the $15 gift card.
“I had chicken and broccoli, and I grilled it on top of the stove–nothing fried,” she said. “It was good, and my husband enjoyed it too.”
She emphasized the importance of programs like Penny Pinchers in helping people realize that healthy eating is possible on a budget.

“A lot of people feel that they cannot eat healthy on a budget, and this proves that they can,” Best said. “Just knowing how to choose the right foods and even getting ideas for preparation makes a difference. It’s important to take time to shop for nourishment, and people need to know they can do this and have fun doing it.”
Best praised the volunteers who led the tour, describing them as “knowledgeable and friendly,” and encouraged others to take part.
“I encourage anyone who has the opportunity to participate in Penny Pinchers to do so,” Best said. “It’s worthwhile. It will open your eyes and help you see that you can eat healthy on a budget.”
Both Thomas and White are passionate about debunking the myth that healthy eating is unaffordable.
“People say it’s expensive to be healthy,” White said. “But this program shows that’s not necessarily true.”
By combining education, empowerment and community support, Penny Pinchers is helping residents in eastern North Carolina rethink their relationship with food and proving that with the right tools, anyone can be a health-conscious shopper.
To register, contact De’Vette Thomas at 252-847-6497 or [email protected].
Greenville, N.C. – Twenty-five ECU Health nurses from five ECU Health hospitals have been named part of the Great 100 Nurses of North Carolina by the Great 100 Nurses of North Carolina Board of Directors, honoring their outstanding professional ability and contributions to improving health care services in their communities. This marks the highest number of ECU Health nurses honored as Great 100 Nurses in a single year.
“With over 4,000 nurses across our system, ECU Health is proud to celebrate the exceptional caregivers who embody our mission to improve the health and well-being of eastern North Carolina,” said Trish Baise, chief nursing executive, ECU Health. “Each nurse honored in the Great 100, and those recognized in years past, represents the skill, compassion and advocacy that define our nursing team. Their dedication is a powerful affirmation of the extraordinary care our communities receive every day.”
Since 1989, The North Carolina Great 100, Inc. has recognized and honored nurses around the state for their commitment to excellence and to promote a positive image of the nursing profession.
Each year, the Great 100 Nurses of North Carolina Board of Directors asks patients, health care workers, friends and family members to nominate an outstanding nurse practicing in North Carolina. Thousands of nominations are reviewed, and 100 nurses are selected and honored at a statewide gala.
“Every day, our nurses bring skill and unwavering dedication to our patients and families of eastern North Carolina,” said Pam Rudisill, vice president of Nursing Excellence, ECU Health. “Having 25 ECU Health nurses named among the 2025 Great 100 Nurses is a powerful testament to the exceptional care they provide and a meaningful reminder to our community that we are here to care for them.”
ECU Health has built a strong culture of nursing excellence which is the backbone of patient-centered care. Last year, ECU Health Medical Center earned Magnet® recognition for its third consecutive accrediting period, awarded every four years and represents the highest national honor for professional nursing practice. The American Nurses Credentialing Center’s Magnet Recognition Program® distinguishes health care organizations that meet rigorous standards for nursing excellence and is considered the gold standard for nursing excellence.
ECU Health will be rolling out stories highlighting each nurse in the coming weeks at ECUHealth.org/Newsroom. The ECU Health nurses chosen as Great 100 Nurses of North Carolina in
2025 are:
- Elizabeth Arnold, BSN, RN, CNOR(E)
- M. Dustin Bass, DNP, MHA, RN
- Britney Beeker, BSN, RN
- April Bracy, BSN, RN-BC
- Sheena Bunch, BSN, RN, VA-BC
- Allison Castelloe, RN, MSN
- Anne Chadwick RN, BSN
- Elaine L. Cudnik, DNP, CPNP-AC/PC
- Kathryn Freeman, RNC-OB
- Christy Harding, MSN, RN, MEDSURG-BC
- Robin Lanier BSN, RN
- Katherine Low, BSN, RN-BC
- Claire McFadyen, BSN, RN
- Connie R. Midgette RN, BSN
- Wendolyn Minton, BSN, RN, CEN
- Randy Mintz, ADN, RN, CEN
- Kaili Nixon, MSN, RN
- Victoria McIntosh Respess, MSN, ANP-BC
- Rebecca Simmons DNP, AGCNS-BC, APRN
- Stephanie Smith, BSN, RN
- Angela Still, MSN RN
- Megan Tripp, BSN, RN
- Gloria Waters, RN, RN-BC
- Sharon Watford, BSN, RN-BC
- Lindsey Woodlief, DNP, APRN, FNP-C
Tom Stanley, manager in Marketing and Communications, discovered the importance of advance care planning (ACP) one afternoon at swim practice.
“My parents were in town to visit the grandkids and dad’s heart suddenly stopped,” Tom shared. “It just so happened there were two physicians right there and they got CPR going immediately.”
Tom’s father, Bill, was transported to ECU Health Medical Center, where he was admitted for testing. During a stress test, his heart stopped for a second time.
“The doctors brought him back and declared him an official heart patient,” Tom said. “He ended up staying in the hospital for several weeks after needing a bypass surgery and a pacemaker.”
During this unexpected event, Tom discovered that his dad had already completed his advanced directives, a step that removed a great deal of worry for Tom and his family because his dad was able to communicate his preferences for care.
Advance care planning, which gives adults the opportunity to plan and record their health care choices in situations where they are unable to communicate what they want, can be a tricky topic to discuss, said Ellie Ward, advance care planning coordinator. As a patient-centered health care system, ECU Health supports informed and shared decision making for our patients and their families.
Two primary advance directive documents Ellie recommended that all adults complete are the
HCPOA and a living will, because the conversations surrounding a person’s wishes are key.
“There is so much nuance around understanding someone’s care preferences,” Ellie said. “Being able to ask clarifying questions is key. For example, if someone says, ‘I don’t want to be a burden to my family,’ do they mean a financial burden? An emotional burden? That’s why these conversations are the cornerstone to good advance care planning.”
“Dad had a stroke 10 years ago, and he put together his health care power of attorney and living will at that time,” Tom explained. “Having everything in place – and knowing what he wanted – allowed us to focus on what the doctors were saying, what he was saying and spending time together ahead of a serious surgery rather than completing these in the midst of all that was going on.”
“It’s not often that family members all agree on a course of treatment if there’s been no prior discussion,” Ellie said. “That can create friction in an already stressful situation. This paperwork, and the conversations around each person’s preferences, gives you and your family peace of mind. You are preparing others to represent your wishes, and it allows you to be the captain of your own ship.”
Witnessing his father’s situation helped Tom realize the importance of having these conversations and completing these documents before the unexpected.
“This turned on the lightbulb for me,” he said. “I realized that it’s necessary because, not only do you make your wishes known, but you also provide comfort and reduce stress for your family, so they don’t have to do this later without you.”
Tom contacted Ellie about how to complete his own HCPOA and living will documents, a task that ended up being seamless and easy after he accessed the ECU Health Advance Care Planning website. The site offers information and step-by-step instructions in the downloadable toolkit. The process is free, does not require an attorney, and can be uploaded to one’s electronic health record. Ellie also noted that people can reach out to her team for information.
“I want people to know that they can request assistance or support, and our team will step up to help them,” Ellie said. “They can also come to any of the free community educational events across our 29 county service area to learn more.”
However, many people don’t recognize the value of the ACP process, or they don’t understand the difference between an HCPOA and a legal power of attorney, or a living will and a last will and testament.
“People think they don’t need to pay attention to advance care planning because they already have a will, or they don’t have a lot of property. But there’s a difference because an HCPOA and living will address health care needs and a POA and last will and testament handle property and money,” Ellie explained.
Specifically, an HCPOA identifies the person or people a patient wants to step in and represent their medical decisions to the health care team. Ellie was sure to clarify that the designated individuals represent the patient’s wishes, not making decisions for the patient.
A living will is a declaration of one’s desire for a natural death and is only in play if two physicians agree the patient is actively dying. The living will determines what care the patient does and does not want to receive at the end of life.
Providing education about ACP earlier in patients’ health care journeys is key, Ellie said, because it empowers our patients, promotes shared decision making and supports patient-centered care, which are essential to ensuring ECU Health’s mission.
“We want to host these conversations early on to make sure we’re aligning the care we provide to the goals of each person,” she said. “This is not just for acute incidents or the chronically ill – it’s for everyone.”
Tom’s father is in cardiac rehabilitation and doing well now, and Tom’s own HCPOA and living will paperwork is complete and on file. That, and the conversations he had with his family, have prepared them to honor his wishes for care.
“You never know what might happen,” he said. “We didn’t expect my dad’s heart to stop, or for him to be in the hospital, but knowing his wishes for medical care was so valuable. Now I’m an advocate for ACP.”
Greenville, N.C. – Dr. Sharona Johnson, PhD, APRN, FNP-BC, NE-C, FAANP the Executive Director of Advanced Clinical Practice for ECU Health, Family Nurse Practitioner at ECU Nephrology and Hypertension and adjunct faculty at ECU College of Nursing has been inducted as a 2025 Fellow of the American Association of Nurse Practitioners (FAANP). This distinguished honor recognizes Dr. Johnson’s significant contributions to the Nurse Practitioner (NP) profession and her dedication to advancing high-quality health care and nursing education.
 “I am honored to be selected as a 2025 Fellow of the American Association of Nurse Practitioners,” said Dr. Johnson. “This recognition affirms the significance of our work as nurse practitioners and the impact we can make in advancing health care. I look forward to contributing alongside an inspiring group of professionals as we strive to elevate the NP role and enhance patient care globally.”
“I am honored to be selected as a 2025 Fellow of the American Association of Nurse Practitioners,” said Dr. Johnson. “This recognition affirms the significance of our work as nurse practitioners and the impact we can make in advancing health care. I look forward to contributing alongside an inspiring group of professionals as we strive to elevate the NP role and enhance patient care globally.”
Dr. Johnson’s selection coincides with the 25th anniversary of the FAANP program, which was established in 2000 to honor nurse practitioners’ commitment to leadership, advocacy, and mentorship. As a FAANP fellow, Dr. Johnson will actively contribute her expertise through roles such as mentoring, committee involvement, journal contribution and global advancement of the NP. Dr. Johnson joins a distinguished cohort of accomplished NPs who have made a lasting impact on the profession and their communities.
“We are incredibly proud of Dr. Sharona Johnson for her well-deserved recognition as a 2025 Fellow of the American Association of Nurse Practitioners,” said Brian Floyd, chief operating officer, ECU Health. “Her dedication to research and patient care exemplifies the level of excellence we strive for at ECU Health. This honor not only reflects her individual achievements but also underscores the caliber of health care professionals within our organization. Dr. Johnson’s work is a shining example of our mission of improving the health and well-being of eastern North Carolina.”
Dr. Johnson brings nearly 35 years of nursing experience to her roles, having served nationally as a bedside nurse, flight nurse, and intensive care nurse. She holds a BSN from South Dakota State University and earned both her MSN and PhD in Nursing from East Carolina University. She is a passionate advocate for nurses, mentoring those pursuing advanced degrees and fostering professional growth across the field. She has a scholarship for nurses in her mother’s honor for graduate nursing students attending ECU College of Nursing. Her professional affiliations include the American Nurses Association, North Carolina Nurses Association, American Association of Nurse Practitioners, American Nephrology Nurses Association, and the National Organization of Nurse Practitioner Faculties. She also serves on the Executive Committee of the North Carolina Medical Board, chairs the Joint Subcommittee of the North Carolina Board of Nursing and is a member of the ECU Board of Visitors. She is past chair of the Center for Family Violence Prevention in Greenville.
Dr. Johnson teaches part time at ECU’s College of Nursing and was sponsored in the FAANP process by Dr. Michelle Skipper, the director of the CON’s Doctor of Nursing Practice Program and Adult Gerontology Primary Care NP and Family NP specialties, and Dr. Bim Akintade, dean of the College of Nursing.
“Michelle and I both suggested that Sharona undertake the process for this honor because she is an important part of the faculty and her dedication to Pirate Nursing, and our shared profession, is unwavering,” Akintade said. “We helped shepherd her through the nomination process and were there in San Diego to welcome her at the induction ceremony as a FAANP.”
The FAANP program honors outstanding leaders in the NP profession who have made a global impact. Through volunteering, mentoring, and advancing the NP role, FAANP members support the AANP’s mission of developing future NP leaders and advancing high-quality health care. For more information about the FAANP program, visit here.



