When Ricky Blount, a supply chain professional, joined what was then Pitt County Memorial Hospital, now ECU Health Medical Center, he was fresh out of high school.
“I graduated from D.H. Conley High School in 1979 and started working here not long after,” Ricky said. “I was supposed to join the military, but my mother had open heart surgery, and she needed someone to be home with her while she recuperated. I started work at the hospital thinking I’d just be here a year.”
That year turned into 45, and during that time he’s mostly worked in one department: radiology.
“I started in patient transport, but after six months I moved to vascular interventional radiology (VIR). I learned on the job and enjoyed it. From there, I became a technical assistant in VIR,” Ricky said.
Recently, he made a change to working in Supply Chain, but he still supports the radiology department.

“VIR wanted someone who was familiar with radiology to do the supplies for the whole department, and my manager wanted to give me more challenging things to do.” To learn the skills related to his new role, Ricky said his team sent him to Maryland for a week of training. “I learned how to do different reports, inventory and manager supplies in the Pyxis machines,” he explained.
Over the years, Ricky said the hospital has changed a great deal.
“It’s much larger, and radiology has grown bigger and bigger. I’ve seen a lot of growth and people come and go,” he said. “Paychecks have grown a lot too. I started at $2.65 an hour, but that was pretty good pay in 1979.”
Through it all, Ricky said he’s worked with great people. “I have a good relationship with the physicians, and they trust my judgement,” he said. “Radiology has also been very supportive. I’ve had great managers and co-workers. They’re family-oriented and work with you when things come up.”
As for his future plans, Ricky said that he hopes to retire soon. “I turned 65 on June 12, but it’s a little scary to think about not working,” he said. “My wife will have projects around the house for me to do and I might find some part time work. I’ll also do some volunteer work at my church.”
Ricky said he has no regrets about staying with ECU Health beyond that first year. “It’s a great place to work. I like helping people and I enjoy what I’m doing. If I had it to do over again, I wouldn’t change anything.”
Greenville, N.C. – Project SEARCH, an educational program offered at ECU Health Medical Center, is proud to announce six students recently graduated from the program: Keon Cox, Nasir Gardner, Kalasiah Forbes-Paige, Cameron McKenna, Daniel Sparrow and Johntevius Walker-Aytch. Project SEARCH is a one-year internship program for students with developmental and intellectual disabilities during their last year of high school with the goal of providing real-world practical skills and increasing the chances of competitive employment.
“At ECU Health, we are proud to support Project SEARCH and help students gain essential career skills that empower them and prepare them for their future,” said Doris Hill, Project SEARCH coordinator at ECU Health. “This program not only equips students with hands-on experience but also strengthens our workforce and community. Witnessing their growth and success is truly inspiring, and we look forward to seeing them thrive in their careers.”

The Project SEARCH program at ECU Health Medical Center began in 2015 through partnerships with Pitt County Schools, RHA Health Services and Employment and Independence for People with Disabilities. Students complete internships in various departments at the hospital, including the ECHO Lab, Gastrointestinal Lab, Central Services, hospital cafeterias, Hospitality, Shipping and Receiving and the Neuroscience Intermediate Unit.
This year’s students who participated in the program are enrolled at various Pitt County high schools including Farmville Central High School, Ayden Grifton High School, North Pitt High School and South Central High School.
“Project SEARCH empowers students with the skills and confidence they need to transition successfully into the workforce,” said Lyndsey Joyner, Project SEARCH instructor. “Watching them grow, gain independence and achieve their goals is incredibly rewarding. I have no doubt that these graduates will make valuable contributions to their communities, and I can’t wait to see what they accomplish next.”
The employment rate for youth with disabilities is about 60 to 70 percent less than youth without disabilities, according to the Office of Disability Employment Policy. Project SEARCH has proven results with a 65 percent employment and 90 percent retention rate nationally. The Project SEARCH program began in 1996 at Cincinnati Children’s Hospital Medical Center (CCHMC) and was developed as a means to meet entry-level employment needs at CCHMC, support their diversity initiative and partner with schools and community services agencies. Project SEARCH is now an international program with over 716 program sites in 48 states and 11 countries.



Chris Norman, PA-C and medical director of ECU Health’s Transfer Center, said he always knew he wanted to work in health care. “My family had a lot of health issues when I was growing up, and I thought I’d be a doctor,” he shared. “Then as an undergraduate, I was introduced to the physician assistant (PA) role. What really drew me in was the idea of doing what I wanted without being in school for so long, and the flexibility to swap specialties.”
After working elsewhere, Norman found his way to ECU Health through the recommendation of a colleague. “She made the switch from our former employer to ECU Health, and she recruited me with her talk about the growth she made as a provider, the team cohesiveness and the overall way PAs are treated,” he said. That professional support has kept Norman in eastern North Carolina for 20 years and has offered pathways to advance his profession, which now include Norman’s work with the NCAPA as president.

The North Carolina Academy of Physician Assistants (NCAPA) aims to, “strengthen the PA profession in North Carolina through advocacy, education and support to improve healthcare for all patients.” Norman helped write that mission statement, something he’s proud of. “If PAs want to advance our profession and help our patients, we have to advocate for ourselves,” he said. “The NCAPA is the only organization solely dedicated to the advancement of the PA profession in North Carolina, and our mission statement resonates with my personal values. We all have one goal for our efforts; our ‘why’ is singular, and that’s my life’s work.”
While Norman learned about the NCAPA in school, he said he didn’t fully appreciate the organization’s significance early on. “If you’re interested in your profession and leadership, you should get involved,” he said. “Once I stepped in, I was all in.”
Initially, Norman got involved by joining work groups and subcommittees, but when he wanted to do more, a colleague suggested he run for a board seat. “This is my fourth year on the Board of Directors, and from there I’ve continued to become more involved, including advocacy in the state legislature and the Leadership and Advocacy Summit with the American Academy of PAs – that is a national conference and you go to Congress. This has been my third year of doing that.” Because of his service and hard work, Norman was then approached about running for president of the NCAPA, a three-year commitment; he is now in his second year of service in that role.
In March, Norman participated in the state Lobby Day, where he, along with many PAs from across the state, advocated for bills that remove obstacles for the PA profession in the state and improve access to care, especially for the rural areas in eastern North Carolina.
“I enjoy my work in Raleigh,” he said. “I get to talk to and advocate with the legislators to have an impact on our mission. And if we keep having these conversations, we will impact the profession.” It’s important that PAs get involved because, he said, “no one tells your story better than you, and no one else understands your needs and concerns.”
Getting bills passed and increasing PA participation in the process have been Norman’s major goals. “Last year we had over 150 PAs and PA students participate in Lobby Day,” he shared. “This year, we had more than 200. A lot of the students came from East Carolina University’s PA program.”
Making this type of difference wouldn’t be easy without the support of ECU Health. “I have a deep-seated drive to learn and tackle new challenges,” Norman said. “ECU Health provides opportunities and encourages my desire to learn and contribute in new ways. Paired with being laser-focused on our mission and values, I love getting up and coming in to work every day, knowing we’re all focusing on the same mission.”
Norman also wants other PAs to get involved. “We need someone to do the work,” he said. “Getting involved with the NCAPA shows a passion that your profession should be the best it can be. Use your own voice, because you are a part of the solution. If you’re a PA and interested in furthering your profession, your first step is to become a member.”
To learn more about the NCAPA, visit their site here.
Each day in hospitals, clinics and other clinical settings across ECU Health, nurses take on roles beyond the medical care they provide – they’re a support person, a patient advocate, offer a hand for food services and help keep rooms clean all while bringing high-quality, compassionate care to patients in eastern North Carolina.
On May 6, to mark the start of National Nurses Week, ECU Health nurses invited board members, executives and other leaders to take part in “Walk-a-Mile with Nursing” to offer the opportunity to shadow a nurse and experience all the different roles that nurses play each and every day at ECU Health hospitals.
“Many of us have experienced the hospital setting through the eyes of a patient or a loved one, but today we got a chance to experience it through the eyes of the people who make high-quality, compassionate care possible at ECU Health: our nurses,” said Chief Nursing Executive Dr. Trish Baise during the roundtable discussion immediately following the three-hour shadowing session at ECU Health Medical Center. “I hope this experience to walk alongside nurses across our hospitals provides an even deeper appreciation for the work they do and the incredible difference it makes in the lives of so many.”

Bob Greczyn, chair of the ECU Health Board of Directors, was one of the guests on the hospital floor during “Walk-a-Mile” and he shadowed nurses on the Cardiac Intensive Care Unit at ECU Health Medical Center.
He said taking part in the event gave him the best morning he’s had in a long time. He was most impressed with the way teams – doctors, nurses, dieticians, pharmacists and more – worked together to care for patients on the unit.
“I’ve heard about doing rounds on patients and how the teams work together, but I’ve never actually been able to see it happen. Now I know what happens, and I know they didn’t just do it for my benefit,” Greczyn said. “I want to thank all the nurses who choose to work here for what you do, because it’s really important.”
Walk-a-Mile with Nursing was also held at community hospitals across ECU Health, where participants captured a glimpse of the community-centered care that makes rural hospitals unique. There, they witnessed team members treating neighbors, family and friends – a testament to the power of hands-on nursing in rural communities.
Gary Stanley, ECU Health Chowan Hospital Development Council Board Member and Lead Chaplain for ECU Health Bertie and Chowan, reflected on his experience with the Walk-a-Mile with Nursing event.
“It was truly an incredible experience,” Stanley said. “Nurse Konner Mims exemplified attentiveness, compassion, and respect, fully embracing the ECU Health model of patient- and family-centered care. This experience was profoundly impactful—I am a different chaplain because of it.”
Dr. Michael Waldrum, ECU Health chief executive officer and Dean of the Brody School of Medicine at East Carolina University, and Donette Herring, ECU Health’s chief information officer, both had the opportunity to return to their clinical roots prior to their leadership roles.
Dr. Waldrum shadowed Carolina Pena, staff nurse III, on the Medical Intensive Care Unit at ECU Health Medical Center. As an intensivist for many years, he said it was great experience to be back at his “home.” He was grateful for the opportunity to shadow Pena and see the heart of ECU Health nursing on display with care, compassion and excellence.

Herring visited the Surgical Intensive Care Unit at the Medical Center. It was a fitting return for her as she said the intensive care unit was her last unit in a clinical role before she transitioned to leadership. She said she wasn’t sure what to expect for the day, but she was grateful to be welcomed in by the unit and have open, honest conversations with the team. She said her biggest takeaway from the day was the importance of taking time to listen to the experiences of nurses and understand their needs.
Pena said she felt this event was important to connect nurses with leadership and non-nursing team members to have their voices heard.
“This was so important to have, because as a nursing staff we go through a lot with patients, doctors, family members and everyone. We never really know if anyone is going to hear our concerns,” Pena said. “I know Dr. Waldrum has been an intensivist before, he knows what happens in our unit, but just having him there, hearing our concerns, seeing our patients, asking questions, it really gives us a sense that we’re being listened to and that we matter. I think that’s very important for our nurses.”
Overall, the event served as the perfect way to kick off National Nurses Week. Other events focused on celebrating nurses and their contributions to high-quality care unfolded throughout the week, and the Walk-a-Mile experience provided a first-hand understanding of just how powerful nurses are in a patient’s life.
“Today has far exceeded my expectations in terms of turnout and the genuine desire to connect, understand and walk a mile with nursing team members,” Baise said. “I’ve done this in previous roles, and there is more enthusiasm today than I’ve seen before, and I think it speaks to the authentic nature of everyone in this system. I’m so grateful for the nurses and units who hosted everyone today and sharing their work with everyone here.”
Photo Gallery
Click the images below to enlarge.
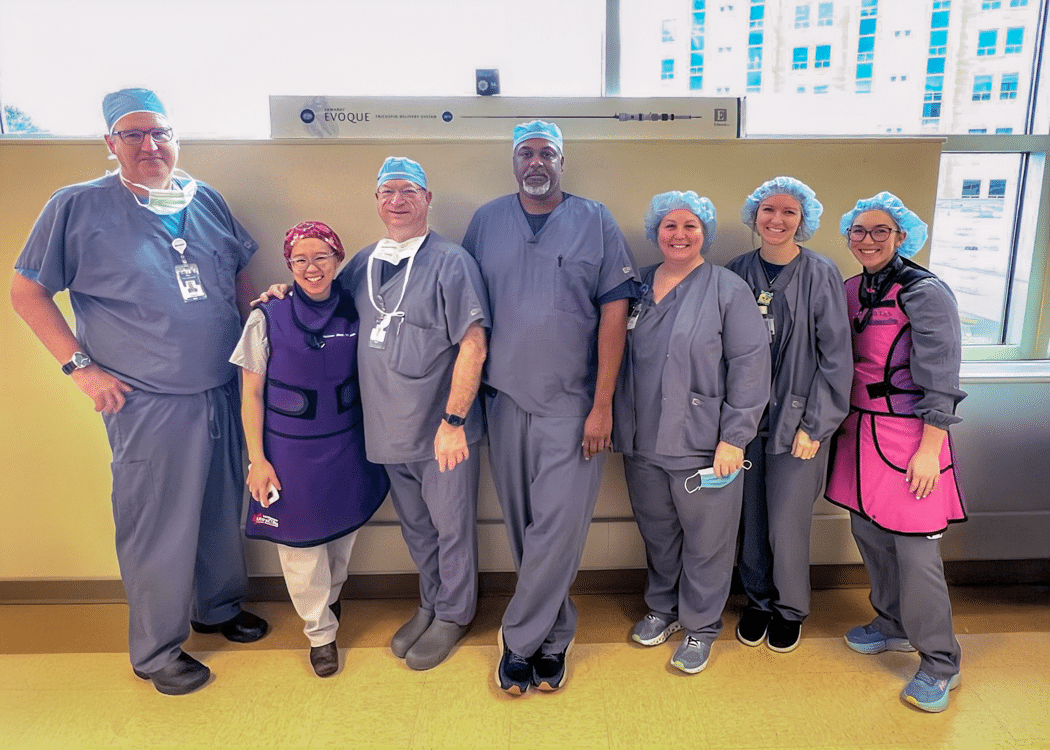
Greenville, N.C. – ECU Health Medical Center is expanding advanced heart care with two new, state-of-the-art technologies for transcatheter tricuspid valve replacement. The new technologies – EVOQUE™, a first-of-its-kind transcatheter tricuspid valve replacement, and TriClip G4™, a minimally invasive clip procedure designed to reduce tricuspid valve leakage – offer new hope for patients previously ineligible for surgery, providing significant symptom relief and improved quality of life.
“These new procedures represent a major advancement in the treatment of tricuspid valve regurgitation, offering hope to patients who previously had limited options,” said Dr. Paul Mahoney, section chief, interventional cardiology, director, Cardiac Catheterization Lab, East Carolina Heart Institute. “With the EVOQUE valve replacement and the TriClip G4, we can now provide effective, minimally invasive solutions that reduce symptoms and improve heart function without the need for open-heart surgery. This is a significant step forward in improving outcomes and quality of life for patients with TR.”
Tricuspid valve regurgitation affects more than 1.5 million people in the U.S. and occurs when the tricuspid valve fails to close properly, allowing blood to flow backward. This condition forces the heart to work harder, potentially leading to heart failure. Risk factors include heart disease, atrial fibrillation (AFib), pulmonary hypertension, prior chest radiation therapy and structural valve damage. Symptoms can range from fatigue and shortness of breath to swelling in the abdomen, legs or neck veins.
Traditionally, treatment options were limited to diuretics for symptom management, with surgical intervention reserved for only the healthiest patients or those already undergoing left-sided valve surgery. However, with recent advancements, including the FDA-approved TriClip G4 and EVOQUE valve replacement, patients now have access to innovative, minimally invasive options that can significantly improve heart function and overall well-being.
“It is critical that patients in eastern North Carolina have access to the latest innovations in heart care close to home, so they do not have to travel far for cutting-edge treatment options,” said Dr. John Catanzaro, John “Jack” Rose Distinguished Professor and chief of the Division of Cardiology at the Brody School of Medicine at East Carolina University, and director of the East Carolina Heart Institute at ECU Health Medical Center. “Our commitment to bringing the most advanced cardiac treatments to this region ensures that patients receive high-quality, life-changing care without unnecessary delays or burdens. I am proud of our heart and vascular care teams who continue to advocate for patients in our region and ensure they receive world-class treatment right here at ECU Health.”
ECU Health team members who participated in these groundbreaking procedures include Dr. Mahoney, Dr. Catanzaro, Dr. Melissa Moey, Dr. Wiley Nifong, Dr. Michael Bates and Dr. Brian Cabarrus. To learn more about ECU Health Heart & Vascular Care, please visit ECUHealth.org/Heart.
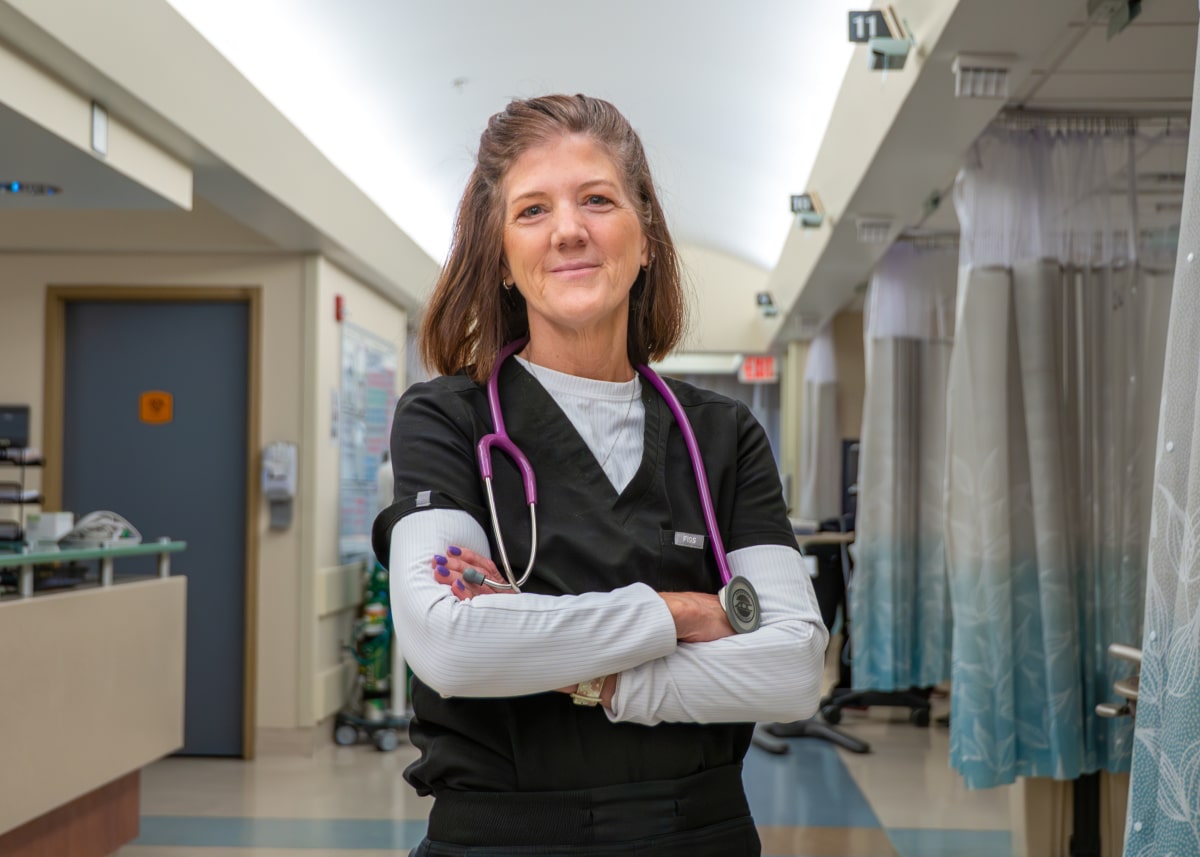
Rebecca Zelnar, a staff nurse III in the post anesthesia care unit (PACU), loved being a travel nurse, and after working for a Florida health system for nearly 20 years, she thought she’d never find a staff position that was as fulfilling. That all changed when she came to ECU Health Medical Center, where she now feels at home.
The Gainesville, Florida native knew early on she wanted to be a nurse.
“I was a candy striper, and in high school I knew I wanted to be a nurse; but then things happened in my family to where I couldn’t go to college right out of high school,” she said. “I got a job and got married, had kids. I worked in the legal field. But nursing nagged at me. In my mid-to-late-twenties, I went back to school. I worked a paper route and as a CNA to pay for school, and I graduated top of my class 24 years ago. I just knew that was what I wanted to be. I went right into the ICU and never looked back.”
She worked at the University of Florida Shands Hospital in the trauma unit for 18 years. “I love critical care. I worked in the surgical trauma ICU at UF and loved it. I love that patient population, and I loved being a part of making science at a teaching hospital,” she said.
Then the pandemic happened, and Zelnar said she saw that as an opportunity to make a change. “My husband and I bought a camper and moved into that, with plans to travel at some point, but then the pandemic came and there was an opportunity for nurses to go to New York City and help,” Zelnar explained. “I asked the Lord if that’s what He wanted me to do. Twenty hours later, I was a Covid nurse in New York.”
Her experience in New York was challenging, but her previous experience in critical care and her work in the ICU float pool prepared her for working in different settings. “There was a lot of fear [in New York]; it was terrible times. I saw how weary those nurses were, and I wanted to be a relief to them. It taught me to rely on my skills in the moment.”
After her time in New York, Zelnar traveled to Texas and worked as a travel nurse in El Paso, Corpus Christi, San Antonio and McAllen before coming to ECU Health in 2021. Her daughter lives in Rocky Mount, and Zelnar said it was nice being closer to her. “I worked in central staffing for the ICU, and I thought I’d just continue traveling when my contract was up,” she said. “But as that time approached, I realized I couldn’t bear leaving this family I’d come to know. It brought me to tears to think about leaving.”
Zelnar said she talked with her husband and she prayed about it, and after talking with the manager of patient care services in the PACU, Amy Sawyer, she decided she wanted to stay. “Amy had a PACU position open, and I accepted the job immediately,” Zelnar said.
“Rebecca brought the knowledge she had gained from working in multiple PACUs,” Sawyer said. “Shared knowledge is so valuable because we always aspire to learn and grow in the nursing profession. Rebecca is compassionate and her patient care is extraordinary. She always advocates for the best possible care for her patients, and she’s been an amazing addition to our family.”
Part of what enticed her to stay were the leadership and staff she worked with every day as a traveler. “I liked the overall friendliness of the staff towards travelers; they didn’t treat you differently. I liked how the nurses cared for each other. It’s a big family, and people are caring and compassionate. It made me want to be a part of their team.” That sentiment stuck with Sawyer. “Rebecca had been traveling for a while but missed the sense of belonging somewhere. She felt that she truly belonged here at ECU Health,” she said.
Rebecca also highlighted the skill set of her colleagues. “The talent of nurses in this unit is very high. It’s the best group of nurses I’ve worked with for long time. It’s the best management team I’ve ever worked with, and I love being a part of the PACU and all their initiatives.”
When asked if she’d recommend ECU Health as a permanent home for other travel nurses, she didn’t hesitate to answer. “I would definitely recommend ECU Health,” she said. “I’m actually recruiting my daughter-in-law, who is a nurse, and my son, to move here from Florida so she can work here. There is a lot to offer for nurses – professional councils, Magnet designation – it’s definitely a place to develop professionally.”
Zelnar said she’s settled in and plans to get her perioperative certification and serve on the unit council, something she hasn’t done in a long time due to being a traveler. “It just feels right,” she said. “I want to work at the bedside and take care of patients, and I love going to work. We moved the camper here and plan to eventually buy some land and maybe build a tiny home. I hope to spend many years at ECU Health.”
Greenville, N.C. – Radio listeners in eastern North Carolina have an opportunity to make a life-changing difference for hospitalized children during the 28th annual “Music for Miracles” radiothon. This two-day event will take place March 27-28 on 107.9 WNCT, along with Inner Banks Media’s other stations: Talk 96.3 and 103.7, Oldies 94.1 and 102.7, and 94.3 The Game. The funds raised through the radiothon will support the James and Connie Maynard Children’s Hospital at ECU Health Medical Center, which serves pediatric inpatient and outpatient needs across a 29-county region in eastern North Carolina.
“The Radiothon stands out as one of our most significant annual events, and we are incredibly thankful for the unwavering commitment of the team at 107.9 WNCT and Inner Banks Media,” said Elise Ironmonger, director of programs, ECU Health Foundation.
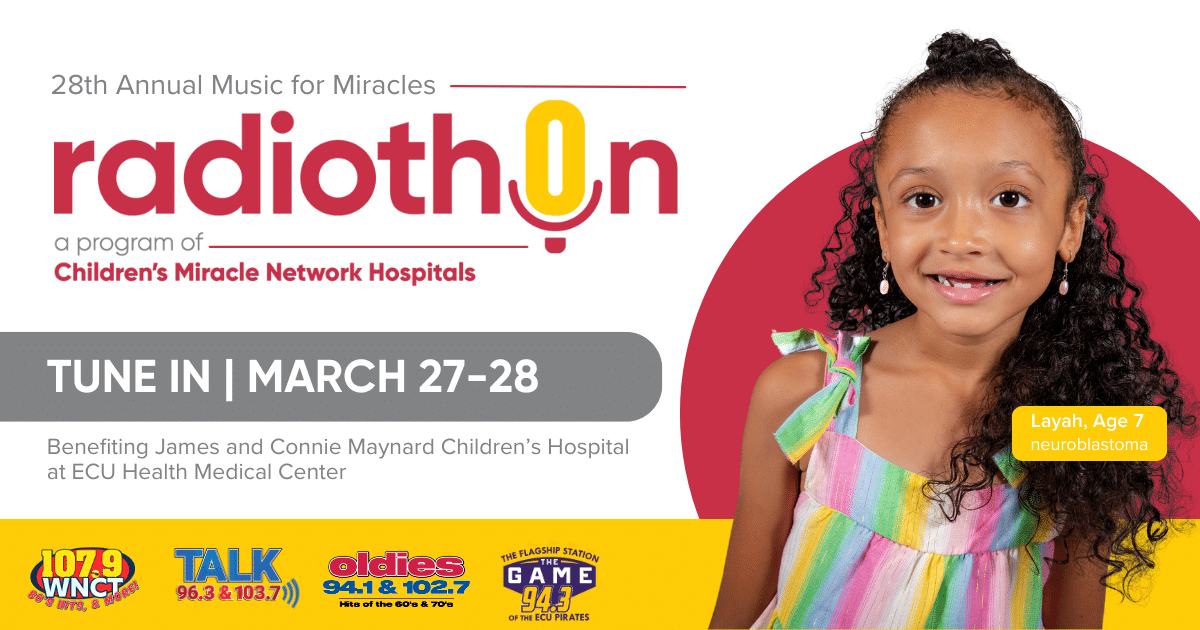
“Broadcasting live for 12 hours over two consecutive days is no small feat, and it’s supported by extensive preparation and behind-the-scenes efforts. This event wouldn’t be possible without the collaboration of hospital leaders, team members, and, most importantly, the brave miracle children and their families who share their heartfelt stories. We encourage everyone to tune in and be inspired by the incredible impact taking place every day at Maynard Children’s Hospital.”
Since its inception in 1998, the event has raised over $3.9 million, all of which goes directly to enhancing the programs and services of Maynard Children’s Hospital. These funds help purchase life-saving medical equipment, support patient and team member education, provide diversionary items to comfort children and normalize the hospital experience and contribute to building new state-of-the-art facilities.
“Once again, we are thrilled to have the radiothon on all our IBX Media stations to raise funds for James and Connie Maynard Children’s Hospital. It’s the highlight of our year to support the children’s hospital,” said Henry Hinton, president, Inner Banks Media. “I’ve personally had a grandson who needed care there, and it is a true blessing for all of eastern North Carolina to have it here. We’re looking forward to two exciting days and hope everyone will participate as they are able.”
Listeners can tune in to 107.9 WNCT to enjoy 12 hours of live broadcasts from 6 a.m. to 6 p.m. on both March 27 and 28, with additional segments airing intermittently across other Inner Banks Media stations. To support this vital cause, please call 1-800-673-5437 or visit www.GiveToCMN.com.
Resources
ECU Health is advancing pediatric surgical care in eastern North Carolina by introducing robotic-assisted surgery, a cutting-edge approach that enhances precision, improves outcomes and expands minimally invasive options for children in the region.
Dr. Courtney Harris, a pediatric surgeon at ECU Health, recently performed the health system’s first pediatric robotic-assisted cholecystectomy (gallbladder removal).
“Robotic surgery is still relatively new in pediatric care, and it offers significant advantages for both surgeons and patients,” said Dr. Harris. “The enhanced range of motion, improved precision and advanced imaging technology allow for a more refined approach, leading to better outcomes.”
Robotic-assisted procedures enhance precision with robotic arms that offer wrist-like movement. This technology provides greater dexterity, similar to open surgery, while preserving the benefits of a minimally invasive approach.

With extensive experience in robotic procedures, Dr. Harris has collaborated closely with Dr. Shannon Longshore, the division chief of pediatric surgery and medical director of the pediatric trauma program at ECU Health Medical Center, and the surgical team to bring this technique to ECU Health.
“Bringing this technology to ECU Health means we can offer our youngest patients the latest advancements in surgical care right here in eastern North Carolina,” said Dr. Longshore. “We’re excited about the possibilities this opens up for pediatric surgery and are committed to expanding access to these innovative procedures.”
Robotic-assisted surgery builds on the strengths of traditional laparoscopic techniques, offering enhanced precision and efficiency, with some procedures completed more quickly. The technology reduces physical strain on surgeons, supporting long-term physician wellness. Both techniques offer similar incision sizes and recovery times.
“The introduction of pediatric robotic surgery at ECU Health marks a significant step forward in expanding minimally invasive surgical options for children,” said Tara Stroud, vice president of Women’s and Children’s Services, James and Connie Maynard Children’s Hospital at ECU Health Medical Center. “ECU Health continues to drive innovation in pediatric surgical care, ensuring that children in the region have access to the highest quality treatments available.”
For Melissa and Jimmy Worrell, their love story started with a horse. Melissa, a horse trainer and riding instructor at the time, met Jimmy when he brought his horse to the barn where she worked. That chance encounter led to marriage in 1988, a move from New Jersey to North Carolina and a life filled with love, adventure and raising their quadruplets.
But in recent years, their journey took an unexpected turn. Jimmy was diagnosed with kidney disease and placed on the transplant waiting list. For nearly eight years, he waited, knowing that each passing day brought him closer to dialysis—a life-sustaining but time-consuming treatment that filters waste from the blood when the kidneys can no longer do so.
“Dialysis is a lifeline for many patients, but machines just cannot do the work of an organ that works automatically, 24/7,” said Dr. David Leeser, professor and chief of transplantation at ECU Health Medical Center. “We know that when a patient is transplanted, they gain a tremendous boost to their quality of life, and they will live longer as well. Transplantation is by far the best available renal replacement therapy available to patients with kidney failure.”
Throughout the process, doctors frequently asked if he had identified a potential donor. Jimmy never asked Melissa to consider donating, but she made the decision on her own.
“I knew I was O-negative, so I figured I’d at least get tested,” Melissa said. “I thought, well, I had to at least try.”

The couple was shocked to learn she was a perfect match.
Throughout the process, Melissa was supported by a donor advocate at ECU Health—someone who had been through the experience and could provide firsthand insight. She believes this kind of support is crucial for potential donors.
“When you’re thinking about doing this, it’s good to talk to someone who has been there,” Melissa said. “It’s reassuring to know that life goes on and that we’ll both live normal, healthy lives.”
Their transplant surgery was successfully completed Nov. 12, 2024. Melissa, now a recreational therapist and volunteer with Team River Runner in Wilmington, which provides veterans and active-duty military with healing opportunities on the water, specifically outrigger canoeing, kayaking, paddle boarding and rowing, took time off to recover. Jimmy returned to work earlier than expected, eager to get back to normal life. More importantly, the transplant has given them back their active lifestyle.
“Before, if I asked him to go for a walk, he’d say, ‘I can’t do that,’” Melissa said. “Now, we can do things together again. It’s a big change.”
The couple enjoys boating along the Intracoastal Waterway, dining out, going for walks and simply spending time together. Beyond her personal experience, Melissa hopes to raise awareness about living kidney donation.
“It’s amazing how something so small can make such a big difference in someone’s life,” she said. “People are often surprised when they hear what I did, like I was risking my own health. But the doctors wouldn’t have allowed it if I wasn’t okay. I think if more people heard these stories, they might consider donating. I especially want to thank the friendly and caring transplant team at ECU Health, who provided great pre and post care.”
For the Worrells, this journey has deepened their bond and given them a renewed appreciation for the simple joys of life. Now, with Jimmy’s health improved, they’re looking forward to many more years of adventure together.
Resources
In 1984, Jaimie Yahnker faced a decision: move to North Carolina with his parents or stay in Long Island, New York.
“Here I was fresh out of high school,” Jaimie recalled. “I went to a school for individuals with cerebral palsy, which incorporated physical therapy and the like into your education, so I graduated when I was 20. After graduation, I decided to move with my parents to North Carolina, which was the best decision I could have made.”
Jaimie was one of seven children, and three of his other siblings also lived in North Carolina. In November of that year, Jaimie was hired by ECU Health Medical Center, then Pitt County Memorial Hospital, and he’s never looked back.
Jaimie’s first job with the system was at the Information Desk, but when that didn’t work out, his connection to what was then called the Education Department through his sister, who also worked at the hospital, landed him a position putting together orientation packets for new team members on a part time basis.

“That went well, and I stayed in that role until I lived in North Carolina for a year and achieved my residency,” he said. At that point, Jaimie knew he wanted to go to school, so he attended Pitt Community College in the morning while working in the education department during the afternoons. “That’s how I got my degree in human services,” Jaimie said.
After graduation, Jaimie applied and interviewed for several different jobs. “No one was hiring,” he said. It was about that time, also, that the Americans with Disabilities Act (ADA) was signed into law, something ECU Health’s then human resources (HR) director Charles Fennessy and the hospital’s HR department knew about and supported.
“He [Charles] was determined to help me all he could,” Jaimie said. “He saw the fire in me. He knew I was trying hard to find work and not getting offers, so he found a full-time position in the Insurance Department under Financial Services, and I worked in that department for nine or 10 years.” During this time, Jaimie also went back to Pitt Community College to get his degree in human resources.
Jaimie enjoyed his work, but he didn’t enjoy being in a cubicle all day. “I’m a people person,” he said. At the same time, Jaimie tore both of his rotator cuffs after walking with forearm crutches for years, an injury that required surgery to repair the damage.
“I knew Dave McRae [the chief executive officer at the time], and I told him I wasn’t sure how my recuperation would go, but that if I could return to work, I didn’t want to be in a cubicle,” he said. After Jaimie’s surgery, McRae helped him find a clinical support position at the front desk in the Rehabilitation department, where he worked first under Martha Dixon, and later with Wanda Bennett.
“Later I worked in hospitality (now called experience) where I stayed for a few years and through COVID,” Jaimie said. “The new rehab director, Dr. Felicia Collins, asked me to come back to their department and I’ve been here ever since.”
While he’s served in several positions across the hospital, Jaimie said he likes his current role because, “I am a good role model for the patients and their family members. They see me do what I am doing, and they think they can also be successful.”
Jaimie also enjoys the people he works with. “They are a great team, very supportive,” he said. “I saw one of our recreational therapists here as a patient, when she had Guillain Barre, and just like me, she had therapy here and was inspired to come back and work. I’m very happy in rehab.”
While he gets asked from time to time when he plans to retire, he has no intentions to leave anytime soon. “Working gives me a reason to get out of bed. I have responsibilities, and I’m comfortable here. It’s the best for my personality.”












