The Great 100 Nurses in North Carolina honors the nursing profession by recognizing nurses around the state for their commitment to excellence. The recipients are distinguished for their outstanding professional ability as well as their contributions to improving health care services in their communities. This year, 19 ECU Health nurses were recognized as honorees, including Dennis Campbell, II, Myra Thomson, Alex Gilbert, Gina Coldwell and Lou Ann Proctor.
Dennis Campbell, II
Although he is now the president of ECU Health Beaufort Hospital and the interim president at ECU Health North Hospital, Dennis Campbell, II began his career in 2004 as a nurse in the medical/surgical intensive care unit. Over time, he spent his early career in the emergency department, the burn center and the telemetry floor, and he was a staff nurse educator and a clinical educator for local nursing schools in his home state of Indiana.

However, a job opportunity brought him to eastern North Carolina, and he’s since navigated his way into quality leadership, corporate compliance, behavioral health and nursing leadership.
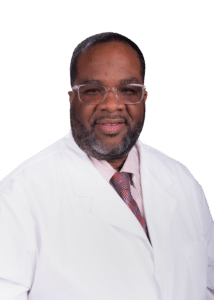 Dennis said finding his path to nursing was a winding road. “I was looking for something I could do that would provide a secure job,” he shared. “I shadowed a nurse in the local community as well as a respiratory therapist. What attracted me to nursing was how polished that nurse was. She was neatly dressed in white scrubs and a hat. The way she presented herself to her patients made me say, ‘I can do that.’” What kept Dennis coming back day after day was the difference he was making every day. “It’s the connection with people at the most vulnerable times of their lives,” he said. “I get to make the ordinary extraordinary, and if there’s something I can do to put a smile on your face, that also fills my cup.” That hasn’t changed since Dennis found his way into leadership roles. “It’s a platform that impacts healthcare and people in a larger way.”
Dennis said finding his path to nursing was a winding road. “I was looking for something I could do that would provide a secure job,” he shared. “I shadowed a nurse in the local community as well as a respiratory therapist. What attracted me to nursing was how polished that nurse was. She was neatly dressed in white scrubs and a hat. The way she presented herself to her patients made me say, ‘I can do that.’” What kept Dennis coming back day after day was the difference he was making every day. “It’s the connection with people at the most vulnerable times of their lives,” he said. “I get to make the ordinary extraordinary, and if there’s something I can do to put a smile on your face, that also fills my cup.” That hasn’t changed since Dennis found his way into leadership roles. “It’s a platform that impacts healthcare and people in a larger way.”
Still, Dennis was surprised that “little old me” was nominated for and selected as a Great 100 Nurse. “It says a lot about what my colleagues think about me, and I’m grateful,” he said. “And it’s good for all Great 100 nurses, because it’s often the case that we are the unsung heroes. It means people are taking notice and want to recognize those who give their heart and soul.” Dennis said the honor is also a legacy for his family. “They don’t get to go to work with me every day and see what I do, and my work is hard to quantify. To have that recognition is impactful to my family.”
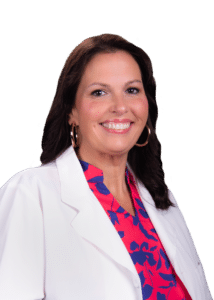
Myra Thomson
 Myra Thomson, a nurse manager in the Medical Intensive Care Unit (MICU) and the Continuous Renal Replacement Therapy program at ECU Health Medical Center, decided to be a nurse because her mother was a nurse. “It was all I knew; I was raised in a medical profession home. It fit me and my personality,” Myra said.
Myra Thomson, a nurse manager in the Medical Intensive Care Unit (MICU) and the Continuous Renal Replacement Therapy program at ECU Health Medical Center, decided to be a nurse because her mother was a nurse. “It was all I knew; I was raised in a medical profession home. It fit me and my personality,” Myra said.
The East Carolina University graduate began her career with ECU Health right after graduation. During her clinical rotation on the medical intermediate unit, she had the opportunity to shadow in the MICU. This confirmed Myra’s conviction to work with the critically ill patient population. “I love that there’s a complexity, with more than one thing to treat,” Myra said. She also enjoys the MICU team. “It’s the place to be,” she said. “I love my team at work and outside of work. They call me if they need something, and I check in on them. They’re my people.”
Myra said it was amazing to find out she was named a Great 100 Nurse. “It’s an honor for me that the people I work with think enough of me to say what they did about me. It shows they’re exactly why I do what I do.” It’s also special that so many ECU Health nurses are recognized this year. “The nurses here work very hard across the system, and they deserve to be recognized. It makes you proud to work at ECU Health,” Myra said.
Alex Gilbert
 Alex Gilbert, a staff nurse III in the surgical intensive care unit (SICU), calls himself a “second generation nurse,” because both of his parents were also nurses. “Mom works in the ECU Health Cancer Center,” Alex said. “Dad was a flight nurse with EastCare. That’s how my parents met.”
Alex Gilbert, a staff nurse III in the surgical intensive care unit (SICU), calls himself a “second generation nurse,” because both of his parents were also nurses. “Mom works in the ECU Health Cancer Center,” Alex said. “Dad was a flight nurse with EastCare. That’s how my parents met.”
Alex used to watch his father on the helipad and wait for him to get off work, which sparked his own interest in a health care profession. That spark was reignited when his grandmother got sick during his senior year of high school. “That renewed my interest and showed me I could care for people. I knew I had a calling.”
After graduating from East Carolina University with his BSN, Alex split his time between the SICU and the ECU Health EastCare Transport Team as a flight RN. He also serves as an EMT-B in the community. Alex said he was surprised when he discovered he was a Great 100 Nurse honoree. “I can think of so many others who deserve this award,” he said. “We don’t do the job for recognition; we do what we do to care for people.” Alex did cite his passion for his work as a key factor in his success, as well as the support from his family and his co-workers. “It’s not just a nine to five job; it’s someone’s life. It’s an honor and a pleasure to care for someone. But I can’t take all the credit. My faith, my family and my co-workers all play a part. I’d put my team up against any in the country, and I wouldn’t be getting this award if not for them. I’m just a piece of the puzzle.”
ECU Health’s representation in the Great 100 Nurses is a testament to the care our nurses provide, and the education and support ECU Health provides its nurses, Alex said. “We’re the biggest level one trauma center East of I-95,” he said. “Our patients are the sickest of the sick, and our nurses are on the top of their game.”
Gina Coldwell
 A Newport News, Virginia, native, Gina Coldwell knew she had an interest in nursing early-on, but she couldn’t go to school while caring for her four small children. “I was a stay-at-home mom for 15 years,” she said. “But then I got divorced and was working two minimum-wage jobs and I wanted to do something I enjoyed.” That’s when Gina went back to school and received her associate degree in nursing from Edgecombe Community College in 2019. “I started working at ECU Health that following summer,” Gina said. She began on the Neuroscience Intermediate Unit, but she also continued her education to complete her BSN from East Carolina University in 2021, followed by enrolling in a master’s program at Carson Newman University, with plans to graduate in 2025.
A Newport News, Virginia, native, Gina Coldwell knew she had an interest in nursing early-on, but she couldn’t go to school while caring for her four small children. “I was a stay-at-home mom for 15 years,” she said. “But then I got divorced and was working two minimum-wage jobs and I wanted to do something I enjoyed.” That’s when Gina went back to school and received her associate degree in nursing from Edgecombe Community College in 2019. “I started working at ECU Health that following summer,” Gina said. She began on the Neuroscience Intermediate Unit, but she also continued her education to complete her BSN from East Carolina University in 2021, followed by enrolling in a master’s program at Carson Newman University, with plans to graduate in 2025.
Gina said she didn’t know what specialty she wanted after initially graduating from nursing school. For her, the team on 3 North drew her to the neuroscience unit. It was a challenging first year, but Gina said she has grown to love the challenge. “It’s hard to not take the work home with me,” she said. “But it’s so fascinating. You get such a diverse group of people, from someone who fell and broke their back to someone who had a stroke. It’s not an easy fix, but you have the benefit of seeing the fruits of your labor and how your patients improve. It’s so rewarding and fulfilling.”
That passion is one reason Gina was nominated for and recognized as a Great 100 Nurse. “I was shocked when I found out,” Gina said. “I was proud because I still consider myself a baby nurse. And we have amazing nurses at ECU Health. We’re a Level I Trauma hospital, and everything we deal with is big. You must have your heart in it, and you must have good leadership that recognizes that heart.” Gina also works with new graduates and new hires. “I love to teach and train,” she said. “And if I don’t know something, I ask someone who does. We’ll find out the answer together.”
Lou Ann Proctor
 Lou Ann Proctor, a staff nurse IV in the pediatric intensive care unit (PICU), calls herself a legacy Great 100 Nurse. “My mother, Janice Proctor, was in the first group selected to be a Great 100 Nurse in 1989, the year I graduated from nursing school at ECU,” Lou Ann said. “My Aunt Lucy Weaver and Aunt Becky Lewis were also chosen in 1994 and 1993. Sadly, I just lost my mother last year, and she would have loved this.”
Lou Ann Proctor, a staff nurse IV in the pediatric intensive care unit (PICU), calls herself a legacy Great 100 Nurse. “My mother, Janice Proctor, was in the first group selected to be a Great 100 Nurse in 1989, the year I graduated from nursing school at ECU,” Lou Ann said. “My Aunt Lucy Weaver and Aunt Becky Lewis were also chosen in 1994 and 1993. Sadly, I just lost my mother last year, and she would have loved this.”
It was her mother’s work that inspired Lou Ann to become a nurse in the first place. “My father was a farmer, so when I turned 15, I wanted to get out of the tobacco fields and I went to work with my mother at Edgecombe General Hospital in Tarboro. I got to work beside her and see how amazing she was at her job,” she said.
Lou Ann has continued that legacy by being nominated as a Great 100 Nurse several times before being an honoree this year, although she remains humble about the work she does every day. “I’ve been a bedside nurse for 35 years and have been involved in Nurse Congress, Quality/EBP Council and my unit council, but there are so many nurses I would nominate for this award. That recognition is overdue and well deserved for them.” When she found out she has won the award this year, the moment was bittersweet. “My co-workers nominated me this time and I was both thrilled and heartbroken to be selected,” she said. “It would have meant so much if my mother was still here. But my Aunt Lucy and family plan to attend the Gala with me and that will make it special.”
The recipients will be honored at a statewide gala in September, to be held in Concord.
Greenville, N.C. – The Eastern Carolina Injury Prevention Program (ECIPP) at ECU Health Medical Center was awarded the Safe States Injury and Violence Prevention Achievement Award at the Safe States 2024 Injury and Violence Prevention (IVP) Professionals Annual Conference in Portland, Oregon on Aug. 20-22. Safe States recognizes the outstanding achievements of members and partners annually through peer-nominated awards.
“We are incredibly proud of the recognition ECIPP’s initiatives have received,” said Sue Anne Pilgreen, manager, ECIPP, ECU Health. “This award highlights our team’s leadership and expertise in injury prevention and advancing safety practices locally and nationally. While this recognition is encouraging, what truly motivates the ECIPP team is getting to see the impact that this work has on the members of our community as we remain dedicated to promoting safety, encouraging healthy behaviors and reducing injuries.”
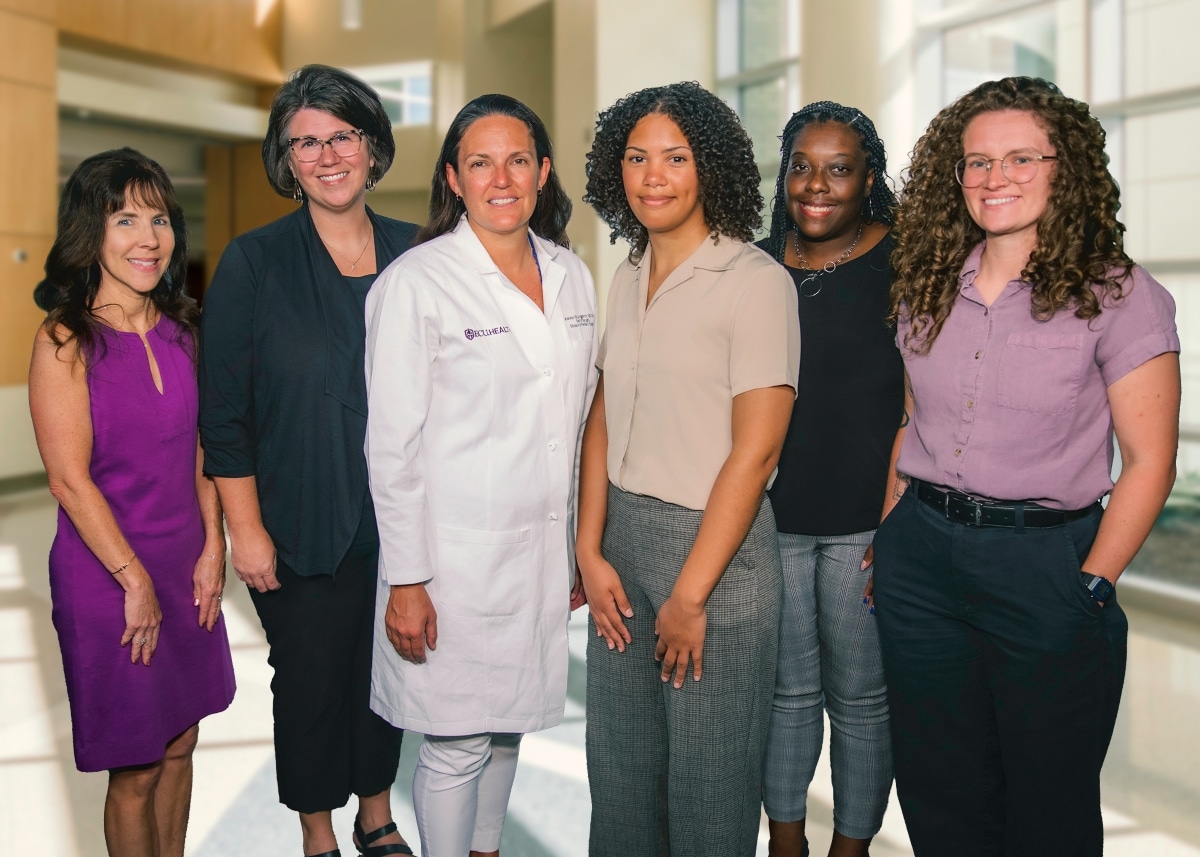
Established in 1995, ECIPP is a collaborative prevention focused health program at ECU Health Medical Center. Partnering with the ECU Health Trauma Center, the James and Connie Maynard Children’s Hospital and the Brody School of Medicine‘s Department of Emergency Medicine, ECIPP is dedicated to improving the health of eastern North Carolina by reducing the incidence and impact of injuries. The American College of Surgeons noted the value of ECIPP’s work in the verification of Maynard Children’s Hospital as a Level I Pediatric Trauma Center.
ECIPP has been instrumental in the development, implementation and interdisciplinary adoption of injury prevention practices for children and adults across eastern North Carolina. ECIPP offers a wide range of prevention programs aimed at addressing the most pressing injury concerns in the region. These programs include education on child safety, teen safe driving, hot car safety, firearm safety, suicide prevention, traffic safety and poison prevention. ECIPP also partners with Greenville Police Department on the Greenville Traffic Safety Task Force, which earned a national achievement award in 2023.
By building innovative partnerships, ECIPP has successfully promoted the adoption of injury prevention practices across various industries. For instance, the firearm safety program collaborates with wildlife organizations and pawn shops to provide education and gunlocks, while partnerships with Community Health Workers help deliver bike safety education and helmets. ECIPP also created an LGBTQ+ youth suicide prevention documentary that has been integrated into college curricula and hospital onboarding processes. From 2020 to 2023, ECIPP reached 86,333 individuals, distributing 2,405 gun locks, 256 medication lock boxes, 3,204 bike helmets and 259 child car seats.
“ECIPP’s strategies and partnerships have been crucial in expanding education and resource access in rural eastern North Carolina communities,” said Catherine Nelson, senior administrator of Community Health Programs, ECU Health. “This award is a testament to our commitment to injury prevention and the positive impact we’ve made for children and families across the region. By collaborating with local organizations and leveraging innovative approaches, we’ve been able to address critical issues, ultimately advancing the health and safety of our communities.”
To learn more about ECIPP, visit the webpage.
ECU Health Medical Center is excited to welcome the newest class of Project SEARCH students. The one-year internship program is designed for high school students with developmental and intellectual disabilities in their final year of their high school education. Through Project SEARCH, these students gain valuable real-world skills, enhancing their employability, confidence and independence.
The Project SEARCH Class of 2024 includes: Cameron McKenna, Daniel Sparrow, Keon Cox, Mariah Locklear, Kalasiah Forbes-Paige, Kenny Lucas, John Walker-Aytch and Nasir Gardner.
“We’re honored that ECU Health Medical Center continues to host Project SEARCH expanding educational opportunities for our students,” said Doris Hill, workforce development coordinator at ECU Health. “This program empowers students with essential job skills they can carry into their careers, while also enhancing diversity within our organization and the local workforce. We’re eager to witness the growth and new experiences our incoming students will gain throughout their journey with us.”

During the program, students participate in internships across various departments at ECU Health Medical Center, including in hospitality, cafeterias, housekeeping and some clinical spaces. These hands-on experiences help students transition from classroom learning to professional environments, bridging the gap between education and the workplace.
The employment rate for youth with disabilities is about 60 to 70 percent less than youth without disabilities, according to the Office of Disability Employment Policy. Project SEARCH has proven results with a 65 percent employment and 90 percent retention rate nationally. Students who participate in the program are enrolled at various Pitt County high schools.
The Project SEARCH program at ECU Health Medical Center began in 2015 through partnerships with Pitt County Schools, RHA Health Services and the North Carolina Division of Employment and Independence for People with Disabilities. The program has become a beacon of hope and opportunity for the students while also making significant contributions to the local community. Project SEARCH is instrumental in cultivating our ECU Health community into one that embraces diversity, inclusivity and shared success.
ECU Health serves a vast rural region and understands the critical need for accessible health care in these communities. The demand for health services is exceptionally high, and many residents face significant barriers to receiving the care they need. ECU Health launched the Health Hub initiative in May 2023 as a strategic effort to bridge these gaps and help meet patients where they are. These Health Hubs are designed to improve access to vital health care and community resources, specifically targeting underserved areas.
“These hubs are strategically placed based on data indicating regions of high social vulnerability,” said Kasey Perkins, community health engagement coordinator, ECU Health. “Oftentimes, these areas have limited access to primary care services and individuals have difficulty seeing a doctor for those unexpected acute illnesses we all get.”
Health Hubs are currently located in four counties: Pitt, Martin, Edgecombe and Beaufort.
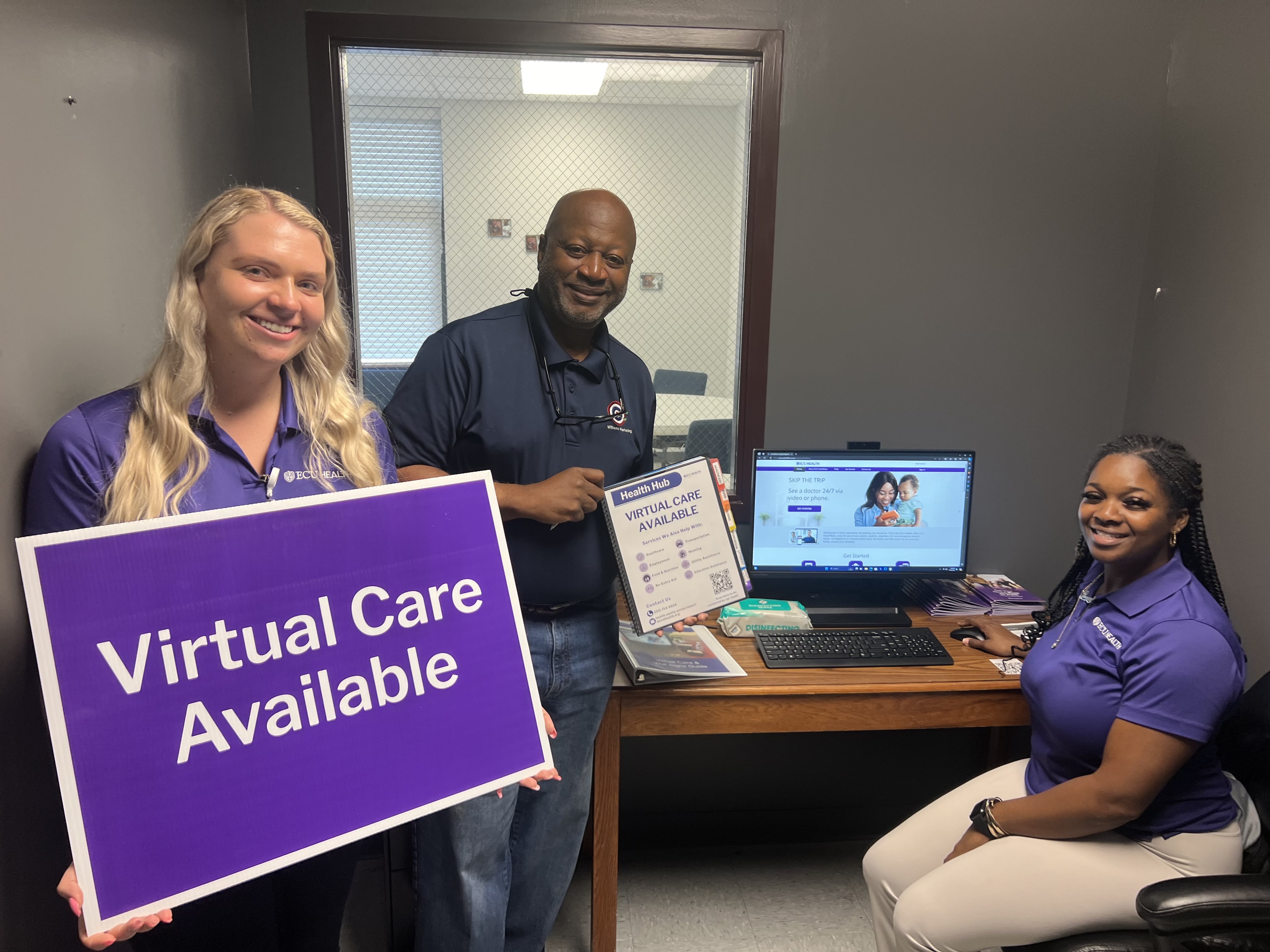
The hubs serve dual purposes. First, they provide access to virtual care, which is particularly vital in areas where individuals might otherwise visit emergency departments for non-urgent issues. By educating the community about virtual care options, Health Hubs help people get appropriate care quickly and more efficiently. Second, Health Hubs offer a gateway to community resources, addressing social determinants of health such as food insecurity, housing and employment.
“Each hub features a community resource guidebook, organized into tabs for different social needs, filled with contact information and details on various agencies and services available in the area,” said Perkins.
Health Hubs are located at local churches, businesses and organizations, and a designated Health Hub ambassador serves as the community’s point of contact. These ambassadors help residents connect with virtual care services and navigate the resources available to them. The hubs are equipped with necessary devices, including a computer with a webcam and microphone, and vital sign monitors like blood pressure cuffs, pulse oximeters and thermometers. This equipment allows individuals to have virtual visits on-site if they don’t have access to the technology at home.
Three new locations were added in July 2024, bringing the total amount of Health Hubs to 21. Health Hubs are open to everyone in the community. Residents can walk in during designated hours to learn more about virtual care or access community resources. The virtual care service, ECU Health Now, is available for anyone throughout eastern North Carolina and can be accessed on a computer or mobile phone. It is free to register and make an account, and it only costs $55 per visit when you speak with a provider, which is often less than a typical insurance co-pay or Emergency Department visit.
“The Health Hub initiative represents a significant step toward making health care more accessible and addressing broader social needs,” said Perkins. “By partnering with local organizations and connecting individuals with vital resources, Health Hubs are making a real difference in the communities they serve.”
As ECU Health continues in its journey toward leading positive changes in support of the health and well-being in the communities it proudly serves, its impact can be seen – and tasted – in the health system’s nine hospital cafeterias where Food and Nutrition team members create delicious and healthy food options for patients and visitors.
With a focus on plant-forward meals that support health, well-being and a healing experience, the Food and Nutrition team has been instrumental in ECU Health’s team member and community-focused Blue Zones initiatives, which recently won the North Carolina Hospital Association’s 2024 Highsmith Award for Innovation.
The four Blue Zones initiatives implemented by ECU Health include the Team Member Blue Zones Challenge, Plant-Forward Meals for patients and team members, Wellness Center Blue Zones, and targeted initiatives in Bertie, Chowan and Dare County. ECU Health is prioritizing the community and engaging in partnerships with local foodbanks and churches to spread the word of the initiative – and make sure the community knows that healthy, plant-forward food is not only nutrient-dense, but also delicious.

None of it would be possible without the expertise of the Food and Nutrition team. With nearly 300 Food and Nutrition team members helping prepare nearly three and a half million healthy and delicious meals at ECU Health locations across the region, this team is making healthy food accessible to patients, families and team members. On any given day, the ECU Health Food and Nutrition team prepares a menu inspired by international cuisines which heavily feature plant-based ingredients: Tandoori chicken, chipotle chicken tacos, sushi, to name just a few.
“It’s hard to describe how fortunate we are at ECU Health to have such an incredible Food and Nutrition team, which is truly at the heart of our work to encourage healthier lifestyles through the Blue Zones initiatives,” said ECU Health Chief Well-being Officer Dr. Christina Bowen. “Our team members and communities benefit from the amazing work they do. Their passion for creating meals that not only taste good, but are also good for you, is a critically important part of the positive change we are leading in eastern North Carolina.”
Greenville, N.C. – The American Heart Association/American Stroke Association has awarded all nine ECU Health hospitals Get With the Guidelines® achievement awards for their work in treating stroke, diabetes, cardiac arrest, heart attack and heart failure. These awards recognize the health system’s commitment to following up-to-date, research-based guidelines for the treatment of heart disease, diabetes and stroke, ultimately leading to more lives saved, shorter recovery times and fewer readmissions to the hospital.
“ECU Health is honored to receive national recognition from the American Heart Association for our unwavering commitment to providing top-tier care to eastern North Carolina,” said Teresa Anderson, PhD, RN, NE-BC, senior vice president of quality at ECU Health. “These achievements reflect the dedication and expertise of our teams who work tirelessly every day to deliver the best possible care to our patients across the health system. By adhering to the latest research-based guidelines, we are not only improving patient outcomes but also advancing our mission to improve the health and well-being of the communities we serve.”
ECU Health recognitions include:

ECU Health Beaufort Hospital – A Campus of ECU Health Medical Center
- Get With the Guidelines – Stroke Gold Plus with Target: Type 2 Diabetes Honor Roll
- Get With the Guidelines – Coronary Artery Disease Rural STEMI Silver
- Get With the Guidelines – Stroke Rural Silver
- Get With the Guidelines – Stroke Rural Bronze
ECU Health Bertie Hospital
- Get With the Guidelines – Coronary Artery Disease Rural STEMI Bronze
ECU Health Chowan Hospital
- Get With the Guidelines – Coronary Artery Disease Rural STEMI Silver
ECU Health Duplin Hospital
- Get With the Guidelines – Coronary Artery Disease Rural STEMI Silver
- Get With the Guidelines – Stroke Gold Plus with Target: Type 2 Diabetes Honor Roll
- Get With the Guidelines – Stroke Rural Silver
- Get With the Guidelines – Stroke Rural Bronze
ECU Health Edgecombe Hospital
- Get With the Guidelines – Coronary Artery Disease STEMI Referring Center Bronze
- Get With the Guidelines – Stroke Rural Bronze
- Get With the Guidelines – Stroke Gold Plus with Target: Type 2 Diabetes Honor Roll
ECU Health Medical Center
- Get With the Guidelines – Resuscitation Gold Neonate/Infant
- Get With the Guidelines – Resuscitation Gold Pediatric
- Get With the Guidelines – Resuscitation Bronze Newly Born
- Get With the Guidelines – Stroke Gold Plus with Target: Stroke Honor Roll Elite Plus, Target: Stroke Advanced Therapy and Target: Type 2 Diabetes Honor Roll
- Get With the Guidelines – Coronary Artery Disease STEMI Receiving Center Gold with Target: Type 2 Diabetes Honor Roll
- Get With the Guidelines – Coronary Artery Disease NSTEMI Gold with Target: Type 2 Diabetes Honor Roll
ECU Health North Hospital
- Get With the Guidelines – Stroke Gold Plus with Target: Type 2 Diabetes Honor Roll
- Get With the Guidelines – Coronary Artery Disease STEMI Rural Silver
- Get With the Guidelines – Stroke Rural Bronze
ECU Health Roanoke-Chowan Hospital
- Get With the Guidelines – Coronary Artery Disease Rural STEMI Silver
- Get With the Guidelines – Stroke Rural Silver
- Get With the Guidelines – Stroke Rural Bronze
Outer Banks Health Hospital
- Get With the Guidelines – Stroke Gold Plus
- Get With the Guidelines – Stroke Rural Silver
- Get With the Guidelines – Stroke Rural Bronze
“Providing high-quality care close to home is essential, especially in regions like eastern North Carolina, where rates of stroke, diabetes and heart disease are significantly higher,” said Dr. Niti Armistead, chief quality officer at ECU Health. “Having access to specialized treatment and adhering to evidence-based guidelines locally ensures that patients receive the best possible care without the added stress of traveling long distances, which can make a critical difference in recovery and overall health outcomes. Get With the Guidelines programs align with our mission of improving the health and well-being of eastern North Carolina by putting proven knowledge and guidelines to work on a daily basis. Patients across our region can take heart knowing that all our hospitals are available to provide them with exceptional care.”
According to the American Heart Association/American Stroke Association, cardiovascular disease and stroke are the leading and fifth leading causes of death in the United States, respectively. On average, someone in the U.S. experiences a stroke every 40 seconds, with nearly 795,000 new or recurrent strokes occurring annually. Stroke claims approximately 140,000 lives each year, accounting for one out of every twenty deaths. The stroke death rate is even higher in eastern North Carolina, underscoring the critical need for preventive measures and rapid treatment. The state also faces a higher prevalence of diabetes and cardiovascular disease. Research indicates that patients experience better recovery outcomes when health care providers consistently adhere to treatment guidelines and programs like Get With the Guidelines.
“These awards show ECU Health’s commitment to caring for those in their community who need cardiovascular care,” said Donald Lloyd-Jones, chair of the American Heart Association Quality Oversight Committee and chair of the Department of Preventive Medicine at Northwestern Medicine. “By following the American Heart Association’s quality improvement protocols, ECU Health can help realize our shared vision of improved patient outcomes, fewer readmissions and lower mortality rates – a win for health care systems, families and communities.”
The summer break was no break for more than two dozen East Carolina University College of Nursing students who got to see what their post-graduation life could be like with a new student nurse extern program sponsored by ECU Health Medical Center in Greenville.
In the summer of 2023, shortly after an expansive academic-practice partnership agreement was signed between ECU Health and the College of Nursing, leaders from both organizations explored options to help expand the number of new graduates who could fill vacant nursing ranks across eastern North Carolina.
One of the initiatives the group quickly agreed on was an extern program: nursing students would be certified as nursing assistants and then work in a variety of care settings across the health system to gain practical experience before starting their final semesters of nursing school.

To be eligible for the extern program, student nurses would be required to complete Nurse Aide II certification, which all nursing students are eligible for, but not all take advantage of. Nurse Assistants are allowed to perform limited patient care activities as well as assist licensed health care workers with taking notes and uncomplicated wound care.
Dr. Jeanne Martin, chair of the baccalaureate nursing program, said the certification gave ECU Health leaders the confidence that the nursing students could “function within the scope of an NA II all the while learning the RN role with their preceptor.”
“During clinical experiences, students function under the licensure of their faculty and may administer meds or other skills not part of NA II certification,” Martin said.
While their practical role was limited, Martin stressed that the intangible skills the students learned – like how to comfort a patient and translate complex medical terminology and procedures to a patient’s families, was invaluable.
On July 9, the graduates of the first extern program gathered at the Monroe Center on the ECU Health campus to celebrate their accomplishments with their preceptors and the leaders who originated the program.
“I’m so grateful that you took this journey with us and congratulations. We appreciate the opportunity to partner with you on your professional journey,” Dr. Trish Baise, ECU Health’s chief nursing executive, said to the graduates during the ceremony. “Our goal is for you to be as prepared as you possibly can be as you transition into practice.”
Baise said she plans to expand and evolve the program so that more nursing students have an opportunity to gain valuable experience while still in school because nursing care is increasingly complicated and challenging.
Dr. Bim Akintade, dean of the College of Nursing, was an early proponent of the academic-practice partnership and said he is thrilled at the results the inaugural cohort of externs achieved during their eight-week experience.
“We are very thankful for ECU Health’s efforts to give our students a chance to learn some of the inner workings of their profession now, before they graduate. Once they are licensed and at the bedside, their nurse managers, and more importantly their patients, will rely on them to be ready on day one, and this experience puts them in an excellent position to be ready,” Akintade said.
Tracy Langston, ECU Health’s director of nursing professional development and innovation, was the medical center’s lead for the extern program and responsible for placing the students in their roles. She is most proud of the growth the student nurses achieved with developing their time management and communication skills.

“It’s been a phenomenal experience for our externs. They really increased their confidence as nurses, they are excited about the skills they were able to achieve and experience, and they’ll use that as they finish nursing school,” Langston said. “They spoke about how this program helped them work on their time management skills and prioritization as they prepare to hopefully join us as new graduate nurses after graduation.”
During the ceremony, students recounted their experiences during the extern program.
Blair Beaulieu, a nursing student from Greenville, said working alongside the family medicine team gave her insights into the working life of a nurse that she just couldn’t get from textbooks and classroom lectures.
“This program allowed me to explore the various opportunities and interdisciplinary communication, walking information down to the laboratory, transferring patients who needed higher acuity needs of various floors — just seeing those inner workings of a hospital,” Beaulieu said.
Kiley Fisher almost missed the graduation ceremony and was dressed in grey scrubs, rather than Pirate nurse purple, having raced over from the hospital after helping with a birth.
Fisher credits her experience with reinforcing foundational skills — like drawing blood and placing Foley catheters — which gave her space to work on critical thinking and communication with all members of the care team.
“I can now not freak out when a patient asks a question that I don’t know the answer to and how to continue to look professional while saying I don’t know, let me find out for you,” Fisher said. “It’s reaffirmed that nursing is where I’m meant to be.”
Emma Campbell, a nursing student who worked in the ambulatory clinics, found her footing, and her voice, while working directly with patients.
“I was challenged to develop my interprofessional communication, my confidence in my interactions with patients,” Campbell said. “Working with family medicine clinics, I was able to improve in these areas substantially.”

Kinsey Cook, one of the student nurses, said the extern program forced her to gain new levels of self-confidence, largely because she wasn’t given a choice.
“I was shy and nervous around other team members, but I gained confidence throughout this program by answering the phone and assessing the plan of care with doctors. I was able to talk to pathology, labs, pharmacy, nutrition services, and I got to see more than just the nursing aspect of patient care,” Cook said.
Cook spoke with pride at learning to believe in herself in the clinical role, as well as advocating for the patients she interacted with, a skill fostered by spending time with a charge nurse in the unit to which she was assigned.
Ankita Das said her experience working with palliative care teams helped her to develop a set of skills that can’t be learned in the classroom — one-on-one interactions with patients and the loved ones in the room with them.
“During this externship I realized I needed to further develop, and learn more about, comforting patients, family members and what to say when their loved ones passed,” Das said. “I observed the chaplains’ interactions with the families — they were empathetic and always offered to talk about memories with family. They lent a shoulder to cry on and a listening ear, this helped me learn what to do and what to say when a patient passes.”
The program’s success has given its leaders hope for future iterations, and opportunities to expand student participation in the future across the health system’s locations in eastern North Carolina.
“One of the reasons for implementing a student nurse extern program is that it’s an excellent recruitment and retention tool,” Langston said. “This is just the start. We are looking forward to continuing our student nurse extern program in 2025, so students — get ready to apply in December.”
As part of its commitment to providing high-quality care to the people of eastern North Carolina, ECU Health now offers innovative advanced 3-D shoulder replacement surgery, providing a new solution for patients with complex shoulder joint damage. This cutting-edge procedure is designed to relieve pain and restore mobility for individuals suffering from conditions such as osteoarthritis, rotator cuff injuries and fractures.
According to Dr. Shawn Yeazell, ECU Health orthopedic surgeon, patients can sometimes have one or more shoulder replacements that failed or wore out, which leaves only a little bit of bone to work with, so traditional implants don’t work.
“We have an aging population, which is increasing the demand for orthopedic procedures like joint replacements,” said Dr. Yeazell. “We want our patients to live comfortably and to be able to do the things they love, so having the ability to provide complex procedures to relieve pain and joint immobility is crucial.”
Traditional shoulder replacement surgeries involve removing damaged bone and replacing it with standard metal and plastic parts. According to Dr. Yeazell, standard shoulder replacement parts work for most people who need a procedure. However, in cases where bone is missing or existing bone is poor quality, standard parts may not be sufficient.
“There’s a certain amount of bone that’s required for a traditional replacement,” said Dr. Yeazell. “The 3-D printed shoulder replacement surgery is a solution for those patients who would have no other option.”
The 3-D shoulder replacement process begins with doctors performing CT scans of the patient’s shoulder. These scans are then sent to an outside vendor, which creates 3D-printed joint replacements custom-fitted to the patient’s anatomy. This personalized approach allows orthopedists to perform surgeries with greater precision and effectiveness.

“Being able to perform cutting-edge procedures like 3-D joint replacement surgeries close to home is critical in caring for our region,” said Dr. Yeazell.
By offering 3-D shoulder replacement surgery, ECU Health is enhancing the quality of life for patients with complex shoulder conditions, ensuring they can continue to enjoy their daily activities pain-free. Dr. Yeazell is the first surgeon to bring the Zimmer Biomet 3-D custom Vault Reconstruction System (VRS) implant and associated technology to the ECU Health System.
To learn more about ECU Health’s orthopedic services, visit www.ecuhealth.org/ortho.
Dr. Audy Whitman wears a few hats: he is the program director for the Rural Family Medicine Residency program at the Brody School of Medicine at East Carolina University; an assistant clinical professor in the Brody School of Medicine’s department of family medicine; and physician at ECU Wound Healing clinic. Balancing multiple roles and responsibilities is nothing new to the eastern North Carolina native, whose resume also includes a stint as a farmer.
“I am from a small town called Seven Springs, N.C. It was and is a farming community,” Dr. Whitman said. “Growing up, I worked on my grandparent’s farm. I worked in chicken houses and hog houses; I’ve cropped tobacco; I’ve driven tractors for harvest.”
It was that hard work, in part, that motivated him to pursue a career in medicine.
“Farming is backbreaking and grueling work,” he said. “There’s no more powerful motivator in the universe to pursue higher education than standing in a tobacco field in later summer, with 99% humidity, no shade and 100-degree temperatures. Your hands are soaked in tobacco gum, and the nicotine is soaking into your skin, so you feel nauseated all the time. I’m not saying it’s not good work to do, but it motivated me to do other things.”
Another inspiration came from his small town’s family physician, Dr. Paul Bennett.
“He was a Med-Peds (internal medicine and pediatrics) doctor by training, but he did everything a family medicine physician would do in a rural community,” Dr. Whitman explained. “He took me under his wing and talked to me about a future career in medicine.”
After high school, Dr. Whitman found himself at East Carolina University where he completed two undergraduate degrees in biology and anthropology and a master’s in cellular biology. Prior to his career in medicine, Dr. Whitman was a regulatory specialist for the North Carolina Department of Agriculture and Consumer Services, in the agency’s Food and Drug Protection division, as well as a contract inspector for the U.S. Department of Agriculture and the U.S. Food and Drug Administration (FDA). In his FDA role, he earned a special citation from the U.S. FDA Commissioner for his work on a nationwide food recall.
“I also worked for the North Carolina Community College System as a pre-health science instructor at Lenoir Community College in Kinston,” he said. “I got tired of my students calling me ‘doctor’ when I hadn’t earned that moniker, so I got serious about the idea of going into medicine. Dr. Bennett told me I should go into family practice, so he helped put me on that trajectory.”
Dr. Whitman attended the Brody School of Medicine, and in 2017, he joined the Department of Family Medicine faculty. In 2020, he was made the program director for the Rural Family Medicine Residency program.
“My detail-oriented work ethic and my ties to rural eastern North Carolina are why I was asked to head up that program,” Dr. Whitman said.
Those ties to eastern North Carolina included experiencing hurricanes that significantly impacted his hometown.
“People not from around here won’t remember hurricanes Fran or Floyd, but I recall vividly that my town flooded very severely over the years from hurricanes, and especially from those two,” he said“I recall sitting on my back deck and realizing our community was an island, and people couldn’t go anywhere.”
He also realized that the elderly and sick had nowhere to go to seek medical care.
“It provided a buy-in for me that we need doctors in these rural communities for events like this when you’re truly isolated and need boots on the ground,” Dr. Whitman said. “That experience played a role in getting the rural program up and running and productive.”
Now, Dr. Whitman is proud of the Rural Family Medicine program’s growth and its impact on rural communities like Seven Springs.

“I help train the next generation of family physicians to care for the people of eastern North Carolina and play an active role in designing systems to address health care disparities in our rural communities,” he said. “It’s fulfilling and rewarding work, and it’s an honor I don’t take lightly.”
Because of his efforts, resident physicians and graduates effect meaningful change across the region.
“When you have a patient come in for a 15-minute appointment, they often have a laundry list of other things to address because this is the one trip to the doctor they get this month,” Dr. Whitman explained. “In these cases, I think about my grandma. How would I want her treated? With these rural program residents, they are taking care of my flesh and blood.”
Without the various roles he’s held over his career, Dr. Whitman said he wouldn’t be the clinician, educator or advocate he is today.
“I’ve had both blue-collar and white-collar jobs. I’ve worked in the unforgiving elements of brutal eastern North Carolina summer heat and in positions where the health and safety of our population were dependent on the actions of me and my colleagues,” he said. “I have worked jobs in which I had the honor to educate and provide eastern North Carolinians the tools to broaden their minds and their career prospects. Through all these experiences, I have gained an appreciation for meeting people where they are and treating people with respect. They have made me who I am and compel me to do the work I do today.”
Dr. John Catanzaro, professor and chief of the Division of Cardiology at the Brody School of Medicine at East Carolina University and director of the East Carolina Heart Institute at ECU Health Medical Center, was recently honored with the prestigious Dr. John “Jack” Rose Distinguished Professorship, recognizing his significant contributions to improving health care delivery, excellence in clinical medicine, administration and academic advancement, including formation of the first Clinical Cardiac Electrophysiology Fellowship at ECU Health.
The Rose Professorship, established by ECU Health and East Carolina University through the ECU Health Foundation and state funds, honors Dr. Rose, a renowned cardiologist and professor. This endowed title supports the director of the East Carolina Heart Institute recognizes Dr. Rose’s exceptional contributions to cardiology and medical humanitarian work. Dr. Rose, who joined ECU Health in 1982 and the Brody School of Medicine in 1990, is celebrated for his dedication to patient care, teaching, and community service. Recipients of this professorship are expected to embody his ideals and passion for teaching, inspiring future generations of medical professionals.

“It’s an honor to be named to the Rose Professorship,” said Dr. Catanzaro. “This title not only recognizes Dr. Jack Rose’s work and legacy, which is focused on humanitarianism and the humanistic qualities of medicine, but it also allows me to highlight and continue his remarkable contributions. As program director, I perform hands-on teaching with trainees during cardiac procedures as well as teach didactic sessions. My primary role is to train the next generation of electrophysiologists to increase access to the patients of eastern North Carolina while maintaining a high standard of excellence in administration and leadership. This professorship is an opportunity to advance Dr. Rose’s legacy of teaching, administration and leadership, ensuring that his impact endures in these areas.”
Dr. Catanzaro completed his Doctor of Medicine with distinction in research at SUNY Downstate Medical Center, followed by an internal medicine residency and cardiovascular disease fellowship at North Shore University Hospital and a clinical cardiac electrophysiology fellowship at The Johns Hopkins Hospital. He also holds an MBA from the University of Florida. He is a Fellow of the American College of Cardiology, Heart Rhythm Society European Heart Rhythm Society and European Society of Cardiology. Dr. Catanzaro is actively involved with the Heart Rhythm Society’s Atrial Fibrillation Stroke Prevention Task Force and serves as vice chair of their Quality Improvement Committee. Nationally recognized for his work, Dr. Catanzaro has delivered invited presentations and chaired panels in the U.S., France, Italy, Germany, England, Romania and more. He also performed recorded procedures for the Heart Rhythm Society Scientific Sessions.
Dr. Catanzaro wanted to transition to an administrative role to broaden his impact beyond individual patients to the entire region and the cardiology division.
“We thought he was the best person for the future of cardiology,” said Dr. Mark Iannettoni, W. Randolph Chitwood, Jr, MD, Distinguished Chair in Cardiovascular Sciences, Brody School of Medicine at ECU and chief, Cardiovascular Service Line at the East Carolina Heart Institute at ECU Health Medical Center. “Dr. Catanzaro possesses a highly entrepreneurial spirit, bringing significant innovation to ECU Health. He has developed new techniques and devices in electrophysiology, advancing our capabilities in device management and patient care.”
The Rose Professorship comes with an endowment, managed by the university, to support ongoing and future initiatives in medical education and innovation. The endowment provides approximately $64,000 annually to advance the cardiology division’s educational and innovative efforts, supporting activities such as purchasing educational equipment, facilitating attendance at conferences, and other educational pursuits.
“The professorship facilitates innovation within the field by providing the necessary funding for new initiatives, such as introducing new devices,” said Dr. Catanzaro. “The goal is to use a certain amount of the endowment each year to support these innovations and to produce more trained physicians for the region. This helps establish our institution as a center of excellence and makes our advancements known.”
Dr. Catanzaro utilized part of the endowment to establish a two-year Electrophysiology Fellowship, admitting one fellow per year, starting this year. Electrophysiologists treat heart rhythm disorders and heart failure with electric devices inserted into the heart. As part of the fellowship, doctors will learn about pacemakers, defibrillators, implantation, ablations, leadless pacemakers, and left atrial appendage closure devices.
“This was one of the fastest fellowships from concept to establishment that we’ve ever done, which just goes to show you how much drive Dr. Catanzaro has,” said Dr. Herb Garrison, former associate dean for ECU’s Brody School of Medicine Graduate Medical Education. “It typically takes two to three years to establish a new residency or fellowship, and we did this in less than a year. That was a record time. And part of that had to do with Dr. Catanzaro and Alyson Riddick, who did an excellent job putting the application together.”
Dr. Jan Lopes is the first fellow in the Electrophysiology Fellowship at ECU Health. He learned about the new program through his cardiology fellowship leader in El Paso, Texas, and decided to join the fellowship because of Dr. Catanzaro’s strong vision for the program.
“Dr. Catanzaro’s enthusiasm for the program and education, along with the opportunity to shape the program for future fellows, attracted me to the fellowship,” said Dr. Lopes. “Despite being a new program, it feels well-established and highly developed. I feel incredibly supported in my role and am receiving top-tier training that rivals what is offered at major medical centers nationwide. We are utilizing cutting-edge technology and performing the latest procedures here at the medical center.”
Training doctors like Dr. Lopes with the latest technology and procedures is important for the future of health care. The need for well-trained electrophysiologists is increasing across the nation and here in eastern North Carolina, according to Dr. Garrison.

“The incidence of arrhythmias, along with the need for pacemakers and defibrillators, is rising as the population ages, making it a critical area of focus,” said Dr. Garrison. “Establishing residencies and fellowships serves two main purposes: recruiting top-tier faculty and creating a pipeline of skilled electrophysiologists. Faculty are attracted to institutions with trainees, and enhancing our program with excellent faculty was a strategic move by Dr. Catanzaro. This initiative ensures we have the necessary capability and qualified physicians to meet the growing demand for electrophysiology services.”
With the increasing demand for physicians and electrophysiologists trained to treat rural patients, Dr. Catanzaro’s efforts at ECU Health is paying off in the form of improved recruitment efforts.
“Dr. Catanzaro has successfully attracted numerous cardiologists,” said Dr. Iannettoni. “He has excelled at developing divisions within the cardiology department and navigating the integration of academia and medicine. His efforts have resulted in many of our graduates choosing to stay with us, which is a significant benefit of our program. We’re proud to retain our own trainees, ensuring continuity and excellence in our team.”

