The Eastern Healthcare Preparedness Coalition (EHPC) recently hosted a regional chemical and radiological tabletop exercise at the ECU Health Monroe Center with local and state partners, including those from hospitals, EMS, EastCare, public health, emergency management, hazmat teams from the Williamston Regional Response Team, and specialists from the 42nd Weapons of Mass Destruction Civil Support Team.
The tabletop exercise – intended to help ensure joint response coordination in response to a large-scale chemical or radiological event – included a brief training session followed by a plausible scenario that led to discussion of possible outcomes and discovery of gaps in preparedness planning.
Following the exercise, an after-action plan will be developed, followed by measures to ensure areas of opportunity are addressed.
The goal, according to event organizers, is to ensure all agencies are best prepared to serve the community.
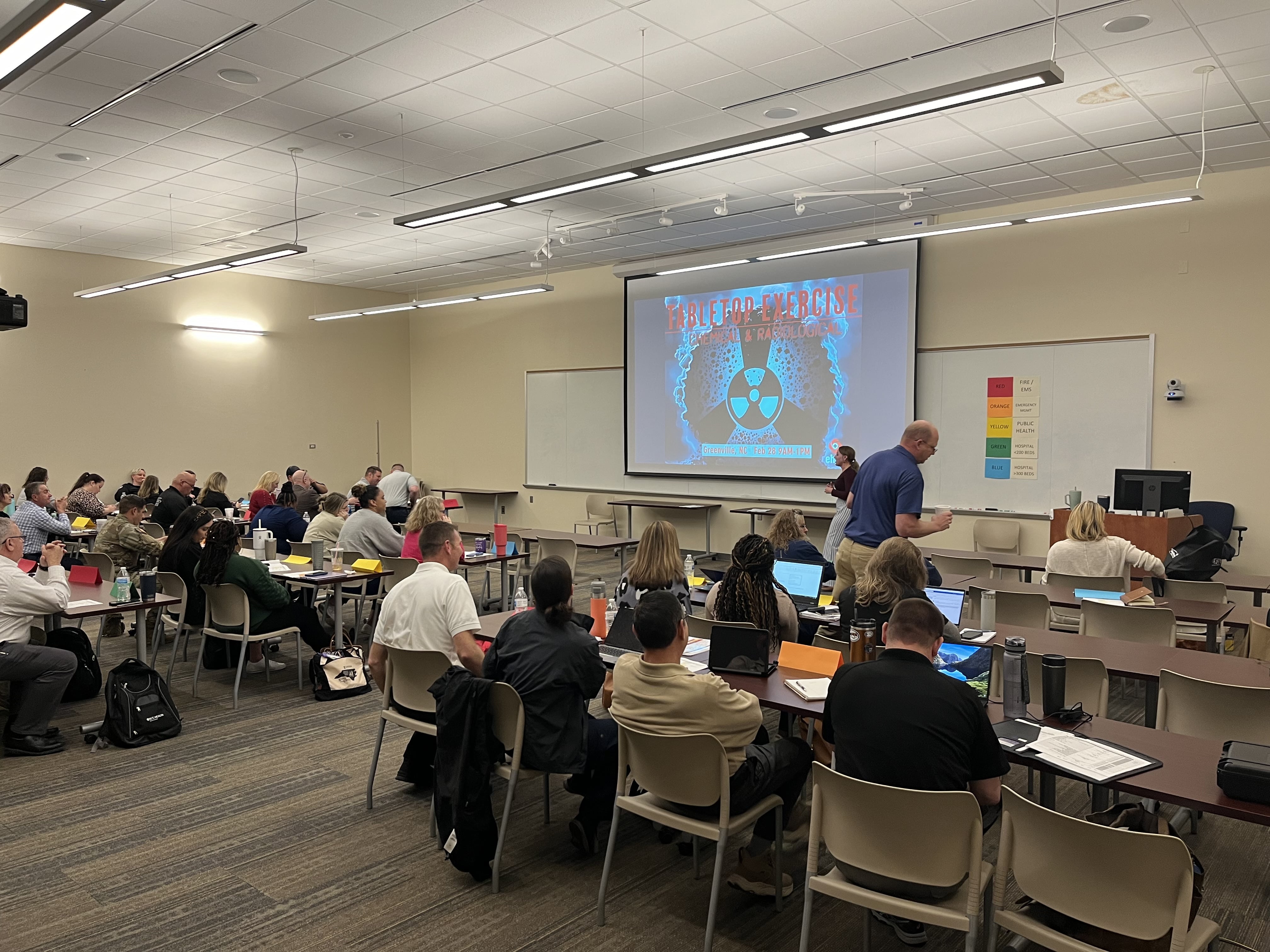
“The tabletop was a fantastic opportunity to collaborate with partners and learn more about regional capabilities available to respond to a radiological incident,” said Christa Radford, Industrial Hygiene Consultant – Eastern Region at the North Carolina Department of Health and Human Services Public Health Preparedness and Response. “EHPC did a great job planning this exercise and bringing the correct response partners together for an extremely successful event.”
EHPC is a multidisciplinary team of medical and nonmedical professionals, established to provide mobile medical support for short and long term disasters or catastrophic events in eastern North Carolina. Roles in which the EHPC can provide support include set up and provision of a mobile field treatment facility, regional and state logistics support, and community alternate care site support.
As the leading health care provider in eastern North Carolina, ECU Health supports EHPC’s mission, in close partnership with other regional and statewide emergency response partners. These partnerships are essential to helping ensure communities across the East have access to high-quality resources and health care, particularly in the event of a disaster situation.
“I feel this exercise was crucial for our disaster preparedness and response,” said Nat Gladding, manager of Hospital Operations at ECU Health Beaufort Hospital. “It helped us assess our readiness, opportunities, and improve coordination between emergency response agencies. The exercise simulated a real-life scenario, allowing agencies the opportunity to practice their regional response to a disaster of this nature. Participation in disaster drills and exercises promote enhancement of our response for the communities of eastern North Carolina.”
Manteo, NC – March 21, 2024 – Outer Banks Health celebrated a significant milestone on March 19 as it broke ground for the expansion of its Family Medicine practice in Manteo. The groundbreaking ceremony was a momentous occasion coinciding with the 22nd anniversary of the opening of The Outer Banks Health Hospital on March 19, 2002.
The expansion project aims to double the size of the existing building, creating a 7,500-square-foot facility dedicated to providing primary care services to the community. With more than 16,000 primary care patients currently served by Outer Banks Health, the Manteo practice stands as the second largest in Dare County, with 3,600 patients, second only to the organization’s primary care practice in Kitty Hawk.
Ronnie Sloan, FACHE, president of Outer Banks Health, expressed gratitude for the opportunity to enhance health care services in Dare County, stating, “We have been fortunate enough over the last year and a half or so to recruit six additional providers to Dare County for primary care.”
![Manteo_Primary_Care_Groundbreaking_Expansion-900x600 Pictured Tess Judge, Outer Banks Health board chair, Lynne Miles, FACHE, administrator of regional operations, Walter Holton, MD [retired], Barbara Holton, and Ronnie Sloan, FACHE, president.](https://www.ecuhealth.org/wp-content/uploads/2024/03/Manteo_Primary_Care_Groundbreaking_Expansion-900x600-1.jpg)
Sloan also highlighted the visionary leadership of Walter Holton, MD, one of the first full-time physicians in Dare County.
“You know, at the end of the day, we couldn’t do any of this without this man here, this physician, Dr. Holton, who came here in 1974 and worked here for 40-plus years and then turned over the reins,” Sloan said. “He had this vision himself. I’ve seen it on paper, to expand this clinic one day.”
The new building’s entrance will face the highway, and is being built to enhance accessibility for individuals with physical disabilities, a crucial aspect of Outer Banks Health’s dedication to ensuring access to care for all members of the community.
Outer Banks Health remains steadfast in its commitment to the community. The expansion of the Family Medicine practice in Manteo along with the recent opening of the state-of-the-art Cowell Cancer Center, reflects Outer Banks Health’s ongoing commitment to advancing health care delivery and meeting the evolving needs of the residents and visitors of Dare County and the surrounding region.
For more information about Outer Banks Health and its services, please visit www.outerbankshealth.org. To find a primary care provider, call the Primary Care Access line at 252-449-4540.
The VAD (Ventricular Assist Device) program at ECU Health Medical Center has recently undergone its fourth successful Joint Commission survey, receiving exceptional praise.
As the largest health care accrediting body in the nation, the Joint Commission emphasizes patient safety and quality of care. The Joint Commission surveys the program’s compliance every two years with more than 40 standards organized into six different chapters in the disease-specific care manual.
ECU Health Medical Center’s VAD program is led by a team committed to providing cutting-edge care for patients relying on ventricular assist devices. A ventricular assist device is a surgically implanted device that helps in the functioning of the heart‘s pumping mechanism. At the Medical Center, VAD patients are often cared for in the following specialized units: CVICU, CIU, CICU, ED and Medical Rehab.

The surveyors highlighted the VAD program’s holistic approach to patient care, acknowledging the dedication of the multidisciplinary team.
“The survey holds our VAD program accountable and ensures that we are providing the highest quality and safest care possible to our patients,” said VAD Coordinator Andrea Matthews. Reflecting on her own participation in the program, Matthews shared her appreciation. “Having the opportunity to be involved in this program and care for this specialized patient population is truly an honor.”
VAD Coordinator Emily Knight echoed this sentiment and emphasized that the resilience of patients and their families is what makes her job rewarding. Knight shared that she’s excited to see what the future holds for the program.
“I am thankful that ECU Health is able to provide this care and treatment close to home for the patients of eastern North Carolina,” Knight said. “I am excited to see the program grow and evolve to reach more patients in our community.”
Since its inception in 2017, ECU Health’s VAD program has grown significantly. The program has successfully implanted 71 left ventricular assist devices (LVAD) and currently cares for 43 patients. Courtney Saunders, advanced heart failure cardiologist, expressed her gratitude for the exceptional individuals within the VAD team who play a crucial role in the program’s success.
“It has evolved into the program it is through the individuals recognized by the surveyor developing a gold standard of LVAD care,” Saunders said. The surveyors specifically highlighted Dr. Tae Joon Lee, Dr. Kari Kirian and Terrani Moore.
Jay Briley, ECU Health Medical Center president, joined the surveyors in commending the team for their hard work in this achievement.
“The Joint Commission survey results demonstrate the program’s dedication to excellence, teamwork and patient-centered care,” Briley said. “Congratulations to all the teams involved in the successful survey.”

ECU Health, Safe Kids Pitt County, Pitt County Coalition on Substance Use (PCCSU) and Pitt County Sheriff’s Office teamed up to host Operation Medicine Drop, an event where the public can dispose of expired, unused, or unwanted prescription drugs or over-the-counter medications. The event at ECU Health Wellness Center on Tuesday, March 19, collected over 200 pounds of medication to be incinerated.
“Operation Medicine Drop began with Safe Kids and this event a resource for us to protect our waterways because we do not want families to flush medications because it will go into our water systems,” said Ellen Walston, Injury Prevention Program coordinator at ECU Health. “It also was a way to keep children safe. Children are curious. They want to learn the world. They are curious climbers, they will pull a drawer out and step in it to be able to reach whatever they are looking for, so we really want to emphasize safe storage. Up, away and out of sight.”
Operation Medicine Drop serves to protect our children, our community and our waters. More than 67,000 children go to an emergency room for medicine poisoning each year, according to a study by Safe Kids Worldwide.
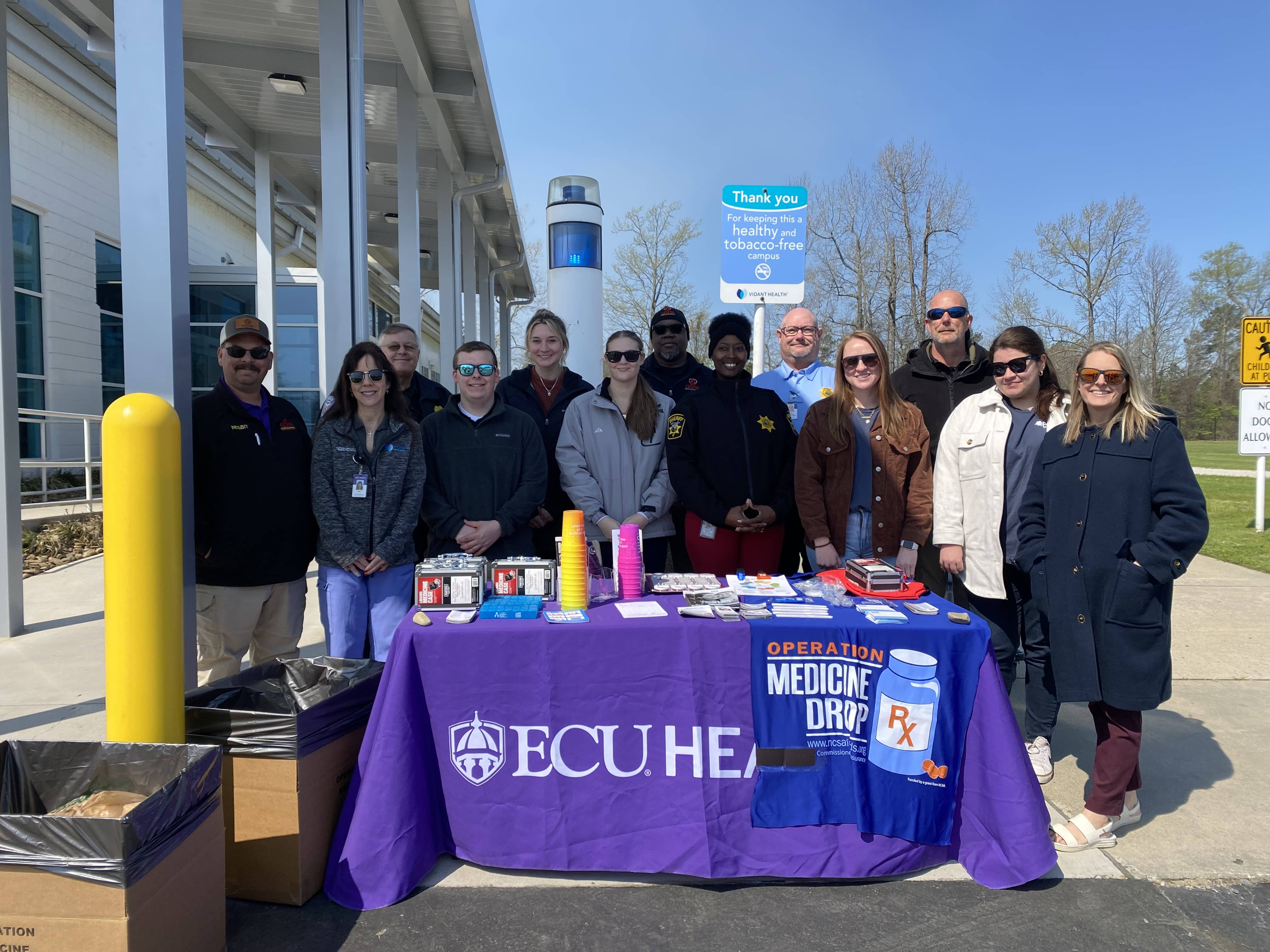
Operation Medicine Drop offers the public a free and convenient option for disposing of their prescription and over-the-counter medications to protect their families and the environment. Since 2010, Operation Medicine Drop campaigns have successfully incinerated more than 266 million pills collected through permanent drop boxes and more than 4,000 events across North Carolina.
“Medication disposal events are a great way to keep the community safe,” said Lillie Malpass, executive director at PCCSU. “Safe storage and disposal keep these medications out of unintended hands of youth and children. We were really happy to partner with community organizations to provide resources for the community, including lockboxes for medications.”
According to Walston, most local sheriff’s offices and police departments and some fire departments maintain permanent medication drop boxes for those who missed the event.
Operation Medicine Drop is a partnership between Safe Kids North Carolina, the North Carolina Department of Justice, the Drug Enforcement Agency and the State Bureau of Investigation.
ECU Health’s Eastern Carolina Injury Prevention Program (ECIPP), through funding by the North Carolina Department of Health and Human Services (NCDHHS), hosted a youth mental health conference for professionals across the state. The event, “Light the Flame: Igniting Hope for North Carolina’s Youth” drew over 250 attendees from a variety of professions including teachers, coaches, school counselors and mental health professionals.
Some of the topics covered included supporting the mental health and well-being of yourself and others, clinical assessment and intervention, safe firearm storage to prevent suicide by firearms, substance use, social media in connection to youth mental health.
“In our youth, suicide stands as the second leading cause of death, with a staggering 31% increase in suicide attempts in 2021,” said Dr. Shannon Longshore, medical director, ECIPP, pediatric trauma surgeon, ECU Health. “There’s an urgency in all of us who work with kids to find solutions and take care of them. We have to focus on prevention rather than recovery and treatment, and conferences like these can help us begin to move the needle.”

While the event drew attendees from across the state, most came from right here in eastern North Carolina.
“This is a great opportunity to provide further education and a chance for professionals from across the state to network and share experiences,” said Breanna Culler prevention coordinator, ECIPP. “Having this event in Greenville allows us the opportunity to bring resources home.”
Multiple vendors attended the event to connect attendees with resources, including Youth Mental Health First Aid, Rural Opportunities Institute, 988 Suicide & Crisis Lifeline, NC School Health Training Center, Resources for Resilience and more.
On March 15, medical students across the country celebrated Match Day as they learned where they will spend their residency training as they continue in their physician journey. Locally, all 79 students in the Brody School of Medicine at East Carolina University Class of 2024 matched, including 14 who will stay in eastern North Carolina to continue their training at ECU Health Medical Center.
Dr. Jason Higginson, chief health officer of ECU Health and executive dean at Brody, said the match statistics of this class reflect Brody’s commitment to leading the way in training primary care providers for the state, as more than half of the medical students matched in North Carolina and 43 of the 78 matched into primary care residencies.
“We have a 100% match rate, well above the national rate, which is also a testament to our faculty and staff,” Higginson said. “About 50% of our graduates are staying in North Carolina, which is our primary mission, and about 20% are staying locally. They are great kids. It’s one of our best classes ever.”

William Taylor matched with ECU Health’s Family Medicine Residency. Taylor is also an ECU alumnus in both undergraduate and soon-to-be medical school. He said growing up in a smaller town made him connect with the needs of eastern North Carolina.
“It has grown a lot now, but when I was growing up, Garner didn’t have as many resources as a big city like Raleigh, and I wanted to impact people in small communities like where I grew up,” said Taylor. “Greenville is my second home, and I want to learn to treat people in North Carolina and eastern North Carolina and make an impact on this area.”
Taylor is excited to continue in Greenville and complete his residency in family medicine and continue to build relationships with patients across the region.
“I want to do family medicine because it gets you closest to the patient where you can build those relationships and interactions over long periods of time and make a real impact on patients and their lives and their families,” said Taylor.
Growing up in eastern North Carolina made the Match Day moment of opening their envelopes even more exciting for a couple of ECU Health matches from Brody.
Nolan Davis is from Duplin County and has fond memories growing up in a small town being close to his family. His mother, Bernice, said Davis made a poster in the second grade that showed he wanted to attend Brody and become a doctor in eastern North Carolina. Davis is one step closer to that goal after matching with his number one choice, internal medicine – pediatrics at ECU Health.
“Eastern North Carolina is a wonderful region, and it’s underserved,” said Davis. “My family lives here, good people live here that all deserve high-quality health care, and Brody is good at getting us to do that. I have seen how hard it is to get a doctor in a small town, and I want to be part of the solution. I was born and raised in eastern North Carolina, and I plan to practice here after residency.”
Marsha Hairr is from Sampson County and matched to ECU Health’s Physical Medicine and Rehabilitation Residency program.
She said her personal experience with physical therapy growing up drove her interest in that area of medicine and her upbringing makes it a joy to serve the region.
“I grew up in a very small town and rural area,” Hairr said. “Even though Greenville and ECU Health is a bit bigger than where I grew up, it still has a rural vibe. It feels like home and I feel so honored that I can continue my training here and meet the mission of fellow eastern North Carolinians.”
For Julia Horiates, who matched into ECU Health’s Emergency Medicine Residency program, the opportunity to continue serving eastern North Carolina in the fast-paced world of the Emergency Department was a dream come true.
She spent most of her childhood in eastern North Carolina and has worked and volunteered as an EMS in Pitt and Greene counties for about 10 years. As a 2017 graduate from ECU and an upcoming Brody graduate, Horiates is proud to be a “triple Pirate.”

“I’ve hit the trifecta now, undergrad, medical school and residency,” Horiates said. “Giving back to a rural community and being involved here still is so special to me. That’s one of the main reasons I wanted to stay. I’ve been able to see how much this community has grown and how much of an impact ECU and ECU Health have had on this community. Being able to be a part of this, and a physician in this community is so important to me.”
Keeping bright minds in eastern North Carolina has long been a priority for ECU Health CEO and Brody Dean Dr. Michael Waldrum. He said a Brody education uniquely prepares future physicians to provide high-quality rural health care, and the training they receive can have an immense impact across the rural region ECU Health serves.
Dr. Waldrum said he’s not surprised that so many Brody graduates find their calling in eastern North Carolina.
“I like to think that all physicians share a common passion for wanting to make a positive difference in the lives of the people they serve,” said Dr. Waldrum. “Brody students get to spend four years here in eastern North Carolina learning about medicine, connecting with our community and experiencing first-hand the immense impact they can have on rural populations. We’re proud to know that many of our Brody students go on to make a difference in communities across the country, but we’re especially proud when we get to see it happen right here in eastern North Carolina at ECU Health.”
Learn more about Match Day for the Class of 2024 here.
Like many health care organizations across the nation, ECU Health is facing an immense challenge: solving the growing health care workforce shortage.
Through community partnerships, the health system is doing its part to grow its workforce, starting right here in eastern North Carolina.
On March 14 at ECU Health Medical Center, students from several local high schools participated in the Health Sciences Academy event “Chat with a Doc.” Nine physicians from various specialties within ECU Health spoke to the students about their responsibilities, the diverse opportunities in the health care field and the rewarding experiences that come from caring for the people of our communities.
Each physician gave a brief overview of their specialty, and students had the opportunity to ask questions along the way. Dr. Matthew Ledoux, Pediatrician in Chief at Maynard Children’s Hospital, shared his insights as a health care provider with the students.

“I was so excited to participate in ‘Chat with a Doc’. I loved talking about the amazing and incredibly diverse opportunities in medicine. I hope the students were just as excited to hear about the opportunity to spend the rest of their lives helping, supporting and healing members of our community. I can’t imagine doing anything other than practicing pediatrics here in eastern North Carolina.”
The students also had the unique opportunity to tour several areas of the hospital and learn first-hand how they all work together to offer high-quality care for patients. The tours included the echocardiography, electrophysiology and catheterization laboratories at the medical center. Students also got to experience the emergency department, a mock operating room and trauma bays.
Lisa Lassiter, workforce development director for ECU Health, was one of the tour leaders. She expressed her excitement about the potential opportunities that an event like this could bring. “Students are our future, and we want to expose them to as many areas and roles throughout health care as possible so they can make an informed decision on their future career path. We are thankful to the physicians and departments who have given their time to make this event possible and help educate our youth.”
Melanie Thompson, a junior at J.H. Rose High School, shared her takeaways from the “Chat with a Doc” event. “It was great to see the doctors so passionate about what they do in their specialties. It was really nice to see that even though they have a stressful job, they love what they do and are passionate about treating patients here.”
Caleb Spruill, a senior at Pitt County Schools Early College, added that it was exciting to connect with the doctors on a real and personal level. “Not only are they passionate about treating patients, but they’re also just normal people. I’ve always put them on this pedestal, but they are normal people, just like us, who went to medical school and worked hard to achieve their goals. That’s inspiring to see.”
Both Melanie and Caleb shared their gratitude for the opportunities they received from the Health Sciences Academy. Melanie mentioned that the Academy has exposed her to a whole new world of medicine that she was previously unaware of, and it helped her realize that anyone can pursue a career in health care as long as they put in hard work. Caleb emphasized that it’s an excellent way to figure out which career path to take. “It’s a great opportunity for people who aren’t sure if they want to go into medicine. Events like this are foundational for understanding what health care is and learning about all of the different careers in this field. Everyone thinks it’s just doctors and nurses, but there’s so many things you can do.”
The “Chat with a Doc” event is another representation of ECU Health’s commitment to growing health care talent locally. Through the Health Sciences Academy, ECU Health partners with public schools to provide eastern North Carolina’s youth with the education and resources to pursue exciting and fulfilling futures in health care. During high school, Health Sciences Academy students complete a minimum of six courses that expose them to potential health care careers and prepare students to pursue college-level health science programs upon graduation. They participate in job shadowing, mentoring, internships, medical research opportunities, career exploration and volunteering.
The Pitt County Health Sciences Academy offers high school students the opportunity to explore different careers in health care and receive real experiences in the health care setting.

The program is a partnership between Pitt County Schools, Pitt Community College, East Carolina University, the Brody School of Medicine, Colleges of Allied Health Sciences, Engineering and Nursing at East Carolina University, School of Dental Medicine at East Carolina University, the Eastern Area Health Education Center and the Greenville-Pitt County Chamber of Commerce.
Nurses and child life staff from ECU Health went to Pactolus Global School on Tuesday, March 19, to host the Teddy Bear Hospital event as part of Pitt County Health Sciences Academy. This fun, interactive event aims to familiarize elementary-aged children with health care workers in a friendly environment.
Elementary school students donned scrubs and personal protective equipment (PPE) to bring their favorite stuffed animals to the Teddy Bear Hospital. Students assumed the role of parents responsible for the toy’s care, starting with checking their stuffed animal into the waiting room to be triaged. ECU Health nurses then examined the stuffed animals and gave them a diagnosis. Nursing staff provided a treatment plan to help the stuffed animal get better. Through this interactive process, ECU Health nurses and child life team members engaged with the children, fostering valuable interaction and promoting health during workshop sessions.
According to Reed Potts, coordinator of Pitt County Health Sciences Academy, the event serves a number of purposes including to increase the awareness of health care, reduce anxiety around doctor’s visits and introduce students to different health care careers.
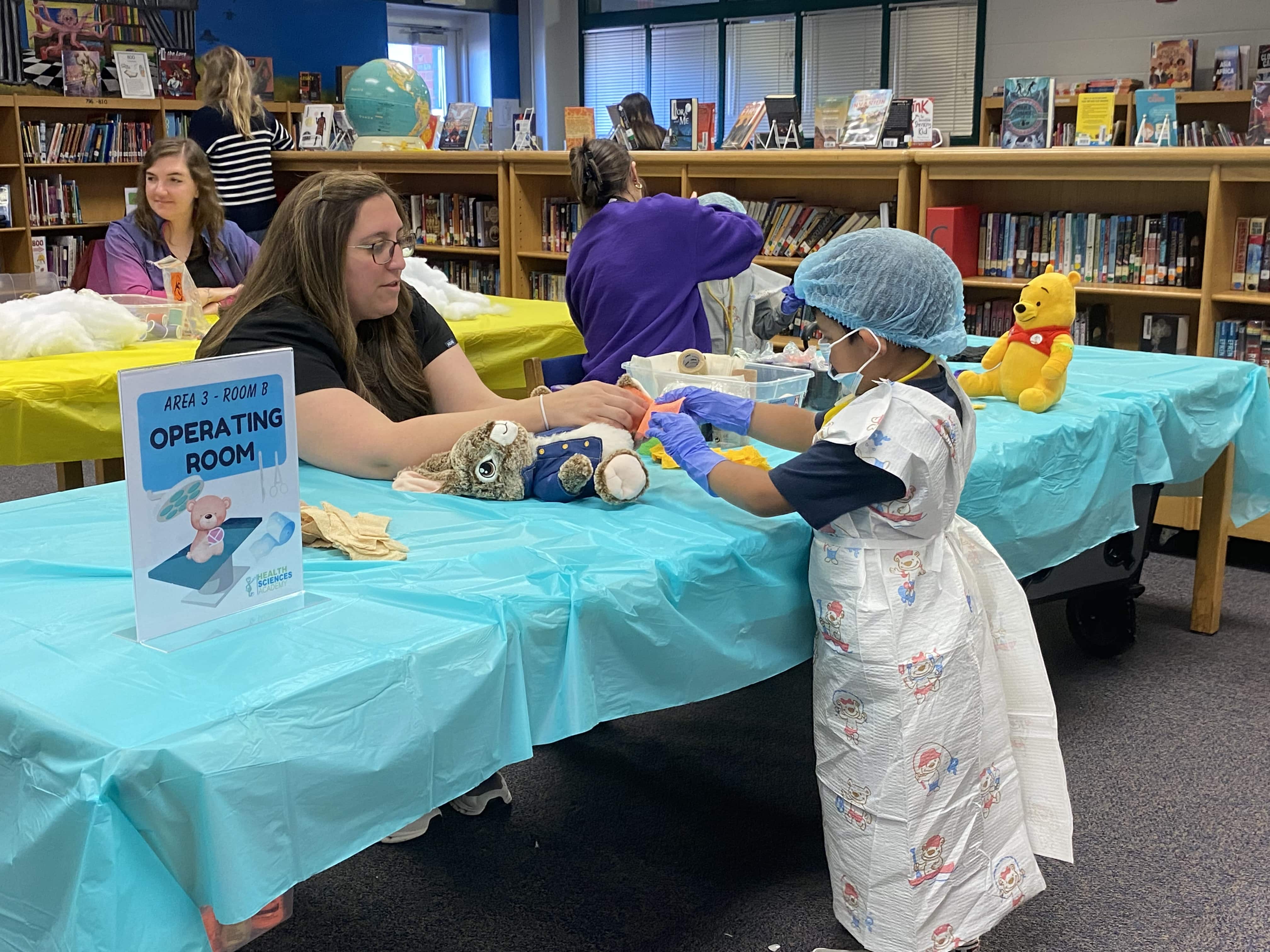
“They’re having an absolute blast,” said Potts. “You never know, we may have a couple of nurses and doctors in here who wind up taking care of us one day.”
Nancy Turner, workforce development consultant, ECU Health, said students have really been engaged with the event and enjoyed the process.
“Students are learning all about health care process as if they are at a doctor’s office or even a hospital,” said Turner. “The students have been great. We’re talking to them after their rotations, and they’re excited to share how our nurses helped their stuffed animals ‘get better’ whether it be with a cast or a band-aid.”
While this may be the first exposure to health care careers for some students, it will not be the last. ECU Health team members, in partnership with Health Sciences Academy, participate in a number of career exploratory events with middle school and high school students including job shadowing, career fairs and “Chat with a Doc.”
“The most important thing is we are able to reach out to students of all ages,” said Turner. “We expose students to health care careers starting in elementary school and continue in middle school and high school letting them know that there a lot of different careers in health care. We’re letting students know there is a health care role for anybody and everybody.”
The Pitt County Health Sciences Academy is a partnership between ECU Health, Pitt County Schools, Pitt Community College, East Carolina University, the Brody School of Medicine, Colleges of Allied Health Sciences, Engineering and Nursing at East Carolina University, School of Dental Medicine at East Carolina University, the Eastern Area Health Education Center and the Greenville-Pitt County Chamber of Commerce.
A standing-room-only crowd packed the Bertie County Community Meeting Space for a robust event on March 19, aimed at getting Medicaid-eligible community members in Bertie and Washington counties enrolled to receive the health insurance they need to live their healthiest lives.
With voices like Gov. Roy Cooper, NCDHHS Sec. Kody Kinsley and ECU Health Bertie, Chowan and Roanoke-Chowan hospitals President Brian Harvill and others providing insight and perspective into the importance of Medicaid expansion, the message was consistent and clear: Medicaid expansion benefits rural communities.
“I know rural North Carolina, and I know what a room full of people who are on a mission looks like,” Gov. Cooper said. “People in rural North Carolina are benefitting from Medicaid expansion and what you’re doing is making a difference.”
The event was hosted by Care4Carolina, a statewide community coalition-building organization that has worked toward shrinking the insurance coverage gap for more than 10 years.

With Medicaid expansion now a reality in North Carolina, Care4Carolina is partnering closely with community organizations in eastern North Carolina, including ECU Health, to help spread the word, provide resources and increase Medicaid enrollment, which helps community members get the comprehensive care they need to better manage their health and overall wellness.
Since Medicaid expansion launched Dec. 1, 2023, nearly 400,000 people have enrolled, providing them and their families affordable health care coverage. Access to coverage ensures patients can receive important medications, access to care and peace of mind needed to live vibrant lives. The impact of Medicaid expansion is even more profound in rural communities where 40% of North Carolina’s population lives. Those living in rural communities face disproportionate incidences of chronic diseases like asthma, diabetes and heart disease, which worsen if not treated. With coverage, these impacted individuals can better manage their conditions.
“Medicaid expansion, more often than not, is here to help rural North Carolina,” said Sec. Kinsley, noting that 70% of those who benefit from Medicaid expansion come from working families. “People in rural communities are 3-to-4 times more likely to be uninsured. Now, with Medicaid expansion, people aren’t just getting covered, they’re getting care.”
Medicaid expansion has long been a priority for ECU Health, which serves 1.4 million people throughout the 29 rural counties that comprise eastern North Carolina. As a mission-driven organization, it proudly serves all community members regardless of their ability to pay. Still, at a time when rural hospitals across the country are struggling to maintain services, ECU Health’s priority is ensuring access to health insurance and access to high-quality care that drives healthy outcomes. That is why ECU Health leaders like Harvill are committed to community partnerships that help drive the mission of improving the health and well-being of the region.
“Sustainability in rural communities is a constant discussion in our organization,” said Harvill. “When you think about Medicaid expansion, think about access to care, which leads to better overall community health in rural areas. When residents are healthier, they are more likely to participate actively in the workforce, contributing to the economic and social well-being of the community. Our work to help improve the communities we serve is rooted in partnerships. We are so thankful for the opportunity to add to the conversation alongside the important state leaders who helped Medicaid expansion a reality and the local leaders who are helping make sure it benefits those right here in our rural communities.”

In a ceremony more festive than formal, fourth-year medical students in the Brody School of Medicine at East Carolina University learned March 15 where they will spend the next three to seven years completing residency training.
This year, 100% of Brody’s 79 members of the Class of 2024 — which began its medical school journey during the COVID-19 pandemic — matched with a residency program.
The traditional event is arguably the pinnacle of the medical school experience for Brody students.
Before they opened their envelopes to reveal their next stop, the students were presented to the audience of family, friends and members of the Brody community to strains of music they each selected as they marched — or danced — across the stage in the ballroom of ECU’s Main Campus Student Center.

“Match Day is such a special time for these students from the Brody School of Medicine, all of whom have worked incredibly hard to reach this exciting moment,” said Dr. Michael Waldrum, dean of Brody and CEO of ECU Health. “Our medical students, by virtue of the education they receive here at Brody, are uniquely prepared to provide high-quality, human-centered care to the patients they will soon serve as part of their residency training and beyond. I want to extend a heartfelt congratulations to the Brody Class of 2024. We are grateful for the positive impact they will have on the lives of so many.”
Dr. Jason Higginson, executive dean of the Brody School of Medicine, said the class of 2024 represents Brody’s mission — a diverse group of students who come from all parts of the state, who will largely return to serve North Carolina as doctors.
“We have a 100% match rate, well above the national rate, which is also a testament to our faculty and staff,” Higginson said. “About 50% of our graduates are staying in North Carolina, which is our primary mission, and about 20% are staying locally.”
One of Brody’s secondary missions is getting future doctors to practice primary care, and half of the class of 2024 have committed to being on the front lines of health care.
“They are great kids. It’s one of our best classes ever,” Higginson said.
A perfect match
Before he even knew the mission carved out by the Brody School of Medicine to reach underserved patients and address health disparities, Connor Haycox was intent on improving lives.
During his undergraduate years at Davidson College, Haycox volunteered and interacted with patients from underserved communities and saw himself as a future physician to help bridge gaps in care.
“I wanted to go into medicine to help address that,” said Haycox, a native of Chapin, South Carolina. “I could see myself as a primary care physician; I figured I could do the most good for people on the front lines.”
Haycox matched in family medicine at ECU Health.
“I know this is where I’m supposed to be,” he said.
After college, Haycox spent two years completing a MedServe fellowship — an AmeriCorps program through which fellows assist in key primary care services and engage in community health work including outreach, education and other projects that impact community health. During the fellowship, Haycox worked in a rural family medicine practice in Benson, North Carolina, where he witnessed “the breadth of the problems patients presented,” he said. “I wanted to be able to meet them in their particular situation and help them maximize their health goals. I really started to see myself in that role.”
By the time Haycox was ready to take on medical school, he knew Brody was the place for him. His goals and his philosophy naturally aligned with the school’s mission, making it a perfect fit.
“The mission of Brody to develop family medicine doctors to serve the state was really a natural transition for me,” he said. “It just made the whole process that much more streamlined. I saw myself here from the start.”
Haycox sees himself serving eastern North Carolina long term — especially since his wife, Dr. Natalie Malpass, a 2022 Brody graduate, is completing a family medicine residency with ECU Health. The two met during Haycox’s stint in Benson, and that experience has cemented his view of medicine as part of teamwork and partnership.
“I think it’s invaluable to have a partner in medicine,” Haycox said. “It’s such a challenging field and an emotional investment, and I feel like having someone to be able to talk to about the things you see has helped me professionally, but it’s more just being able to walk through life with someone who understands.”
Working with the Benson clinic to respond shortly before medical school to help the team coordinate the practice as a COVID-19 testing site also showed him the importance of taking unforeseen circumstances and transforming them into something meaningful.
“Medicine is personal, and we adapt,” Haycox said. “We do that because we need to for our patients. The pandemic was a whole learning process, and it taught me that we may not have all the answers, but we can learn with our patients how to best come out.”
Navigating the pandemic with his classmates also taught him lessons about adaptation, appreciation and taking advantage of opportunities that presented themselves over the years. Haycox served as an anatomy tutor and was part of Brody’s Medical Education and Teaching Distinction Track cohort — which prepares students to be effective medical educators and develops their interest in academic medicine.
“I can see myself going into academic medicine in the future, so I wanted to develop those skills,” he said.
As for the culmination of his Brody experience, Haycox is excited to celebrate his next step alongside his family. For him, Match Day is the beginning of a new adventure in primary care and family medicine.
“Medical school is a long haul, so I’m excited to celebrate with my family,” he said. “Today, all of this kind of becomes more real.”
From motherhood and maternal medicine
For most medical students, finding out where they will complete their residency during Match Day is plenty to celebrate. For Ahoua Dembele, that’s just the start of the day’s festivities as her family is in town for an equally joyous celebration: a baby shower for her third child, due in just four weeks.
Dembele moved with her family from her home in Ivory Coast to Senegal, then attended boarding school in France. She returned to Africa’s north coast, this time Tunisia, with her family for six years before finally settling in Charlotte after graduating high school in 2011.
When Dembele arrived in the States, she had some measure of command of a number of languages – French, Arabic and an understanding her first language, Dyula, a dialect of Mande, but she didn’t speak English. She enrolled at Central Piedmont Community College for a crash course in a new language and started her educational journey.
After a few years at the community college and managing a pizza restaurant, she transferred to UNC Charlotte, where she graduated with a degree in biology because she was always fascinated with science.
She soon had her first son and worked for a while as a medical assistant in a doctor’s office in Charlotte.
Dembele was accepted as a medical student at Brody just before the COVID-19 pandemic complicated just about every aspect of life – especially education. The disconnected learning was tough, but she excelled, especially in light of having her second son just before starting school and getting married to her long-time partner who was frequently out of the country for business.
“I started medical school when my oldest was 2 or 3 and my youngest was 1. Daycare regulations were a little weird and my school was, too. We couldn’t go to Brody because of COVID, so I had to find ways to study,” Dembele said.
Her mother stayed with her to help with the boys and when her husband was home “he would do everything so that I could find places to study, but it was hard because they still need their mom, so I had to find ways to at least do bedtime every day.”
Dembele matched to undertake her residency in obstetrics and gynecology at ECU Health. She wants to make a difference in the lives of mothers and babies, especially after witnessing health conditions in eastern North Carolina through her clinical rotations. She hopes to sub-specialize in maternal and fetal medicine.

“Something about pregnancy has always attracted me. It’s miraculous, phenomenal, that a body can do that,” Dembele said. “It’s mind blowing. I’ve seen a lot of deliveries, but I’m always amazed, every time, even at my own.”
She credits Dr. Jill Sutton, a clinical associate professor at Brody who specializes in obstetrics and gynecology, with invigorating her desire to focus on pregnancy and women’s health.
“The first time she taught us she was so bubbly, so excited and so joyful when she was talking about pregnancy,” Dembele remembered. “Her enthusiasm, her devotion. I was like, ‘Oh my God, this is who I want to be.’ She’s been a mentor for a long time, and I hope to stay here and continue to train with her.”
At Match Day, Dembele was joined by her husband, her boys and her mother, who traveled from Wisconsin, where they now live. She beamed with pride amidst a family that had travelled so far, and made real sacrifices, to stand with Ahoula as she tore open the envelope that revealed where the next few years of their lives would play out.
Dembele will have a few weeks with her newest child before starting residency as she and her husband planned — calculated — the pregnancy meticulously.
She is a scientist, after all.
‘That’s the kind of doctor I want to be’
The few minutes it takes for the National Resident Matching Program’s mathematical algorithm to match applicants and programs across the country can be daunting for many medical students to think about — but for Emmalee Todd, reflecting on those fateful moments feels a bit zen.

“I think that no matter where I end up, I will find a way to be happy and fulfilled and feel like I’m moving in the direction I want to move in,” Todd said. “I feel like regardless of where I have ended up, I’ve been able to find my own path in that setting.”
And they will do it again.
Todd, who crossed the stage to the inspiring lyrics of Shakira’s “Try Everything” from the movie “Zootopia,” was joined by their parents and girlfriend Friday as they opened their envelope to reveal that they matched in internal medicine and pediatrics — known as “med-peds” — at the University of Maryland.
“I’m really excited,” Todd said. “Maryland made a really good impression on me. I’m excited for it.”
Todd’s journey through medical school was inspired by leadership experiences, bonding with fellow students and learning to adjust to what comes in ways that ensured not only success but a lesson to carry with them into the next chapter. A member of Brody’s first class to begin medical school under “pivoted” protocol because of the COVID-19 pandemic, Todd said their class made up for lost time later.
“For most of us, 2020 was pretty lonely,” they said. “We were thrown into this whole new level of work and new level of stress, and we wanted to be able to lean on our classmates.”
The Class of 2024 leaned into the changes, however, and started forming bonds as they interacted during some classes and labs and outside of school. Those bonds have stood the test of time and have been a vital part of Todd’s experience — which really began when they were an undergraduate at Northeastern University in Boston studying behavioral neuroscience.
Todd became an emergency medical technician and got a firsthand look at medical care — after getting a taste of the health care field over the years from their mother, Dr. Karen Todd, a pediatrician and Brody alumna herself. That exposure, coupled with making friends from all over the country and world, helped lead Todd toward a career in health care.
“I was meeting people from places I’d never been before,” they said.
After working for two years as a medical assistant, Todd brought that same energy to Brody, where they could see themselves as part of a smaller class.
“It really came down to the vibes,” they said. “It was one of the few places I interviewed where I felt a connection to the people, students and faculty right away. I could see myself here.”
Todd has thrived, taking on leadership roles including class diversity representative, executive treasurer and vice chair on the Medical Student Council, an elected organization that represents the medical student body as a voice in education, political and social interests.
“I got nominated our first year and decided I was going to run,” Todd said. “I got elected, and there I was. When you’re asked for your input, it’s because someone thinks your input is valuable. It is an honor, the trust [my classmates] have placed in me to be a voice for my class, to speak up and advocate for changes, policies and guidelines that are going to improve or rectify parts of our experience.”
Todd, who was drawn to med-peds because of an experience during a third-year rotation.
“I was trying to be open-minded, though I initially thought I wanted to do emergency medicine,” Todd said. “During my internal medicine rotation, I spent two weeks in the med-peds clinic and fell in love with the feel of it, with the attendings and residents and their personalities and the way they thought about medicine and approaching their patients. The more I got to interact with them, the more it reinforced that that’s the kind of doctor I want to be. They were passionate about trying to do the right thing for their patients.”
Drawing upon every memory and experience they gained along the way — from undergrad to Match Day — Todd is ready to embrace the next step and to take advantage of all the lessons waiting on the horizon.
“I thought when I was in undergrad that I wanted to get my Ph.D.,” they said. “I love neuroscience; I loved feeling like I was on the cutting edge of the frontier of knowledge, pushing into something that people have never known about before. But the more I got into the clinical environment, I really liked the detective work aspect of medicine, the team feel of it. All of the members of the health care team bring their own skills to the table but have the same goal, which is making the patient better.”