Tony Parker has always been an active runner and has long supported the Greenville running and biking community. When he collapsed near the finish line of a 5K road race due to cardiac arrest, quick action saved his life.
Tony was scheduled to run the half marathon that morning back in March of 2021, but backed down to the 5K after his knee started bothering him. It also gave him the chance to run alongside his wife, Delia. It turned out to be a life-saving choice.
“If it weren’t for Delia and the fact that she knows CPR, I wouldn’t be here today,” Parker said. “And if it weren’t for the city of Greenville and the rescue paramedic squads with their AED (automated external defibrillator), I wouldn’t be here today.”
He said he remembers running ahead of his group, including his wife, in the last stretch of the run since his knee was feeling better than anticipated. He patted a young runner on the back to encourage them and then he collapsed.
Delia, a dental assistant with the Department of Veterans Affairs, was required to take CPR courses every three months as part of her job training. That morning, her training paid off in a way she never imagined.
“I got up to the corner and I heard somebody shouting, ‘Man down.’ And when I turned the corner, I was like, that’s Tony,” Delia said.
Delia yelled for someone to call 911 and checked her husband for a pulse, but found none. So she started CPR.
“No one tells you when you’re training on a mannequin that you’ll hear crunching. No one tells you on a mannequin that it’s a different feeling when you’re pushing on somebody’s chest. And it was a little freaky when I first did it, but I was able to stay where I was and to do the compressions,” Delia said. “Someone, ‘Angel,’ as he liked to call them, came up and said, ‘Can I help you?’ They took over and I did some breaths for him.”
Tony and Delia still have not been able to track down the mystery “Angel” from that morning who helped them with CPR.
Shortly after, paramedics arrived and took over. They told Delia that Tony had been revived and he was on his way to ECU Health Medical Center. Paramedics could quickly identify Tony and his wife because he was wearing a road ID, which gives paramedics information on a person, should an emergency event occur. Tony and Delia said they encourage people in their running and biking groups to wear a road ID for these situations.
Delia met Tony at the hospital and some tension was relieved when Tony greeted her with his nickname for her – “Hiya, toots.”
Tony spent about a week at the hospital while the care team ran tests and navigated next steps for the Parker family. They said their time at the hospital and in clinics since has been reassuring and helpful as Tony adjusted to his new normal.
“The care there was incredible. When I say care, I mean that as the word of choice. They really care about what they’re doing and they make sure that they take care of you,” Tony said. “For somebody with a personality like mine, they make sure I don’t try to overdo it right away. The follow up has been spectacular. They stay in contact with my primary care doctor so we’re all on the same page as to what’s going on. ECU Health has been incredible.”
Dr. Christopher Gregory, an interventional cardiologist with ECU Health, said cardiac arrest can come on with no symptoms in some patients and out-of-hospital cardiac arrests are very uncommon to survive due to how quickly care is needed in these cases. Though they may seem similar, Dr. Gregory said it’s important to know the difference between a heart attack and cardiac arrest.
“Heart attacks are when the blood flow to the heart, because of blockages in the arteries, generally speaking, that feed the heart, is impaired,” Dr. Gregory said. “That causes the heart muscle to be stressed, strain or even die – that’s a heart attack. Cardiac arrest is when the heart itself stops. Sometimes heart attacks cause cardiac arrest, but they are completely different.”
Today, Tony is back out walking, running and biking as often as possible. He’s involved in groups of athletes that have experienced heart attacks, cardiac arrest or other heart health challenges and he said this has given him a great perspective on his own journey. As an advocate, Tony meets with groups around the state to stress the importance of road IDs, greater access to AEDs and the need to stay active throughout your life.
“I would rather be an active participant in life than a passive participant and I’ve seen the difference it’s made in the lives of people around me,” Tony said. “My father was very active and his quality of life was excellent. He did have a stroke that impacted him, but he was still walking and getting out there. He played senior games basketball at 86 years old. So when you see the difference, you understand.”
Learn more about ECU Health Heart & Vascular Care.
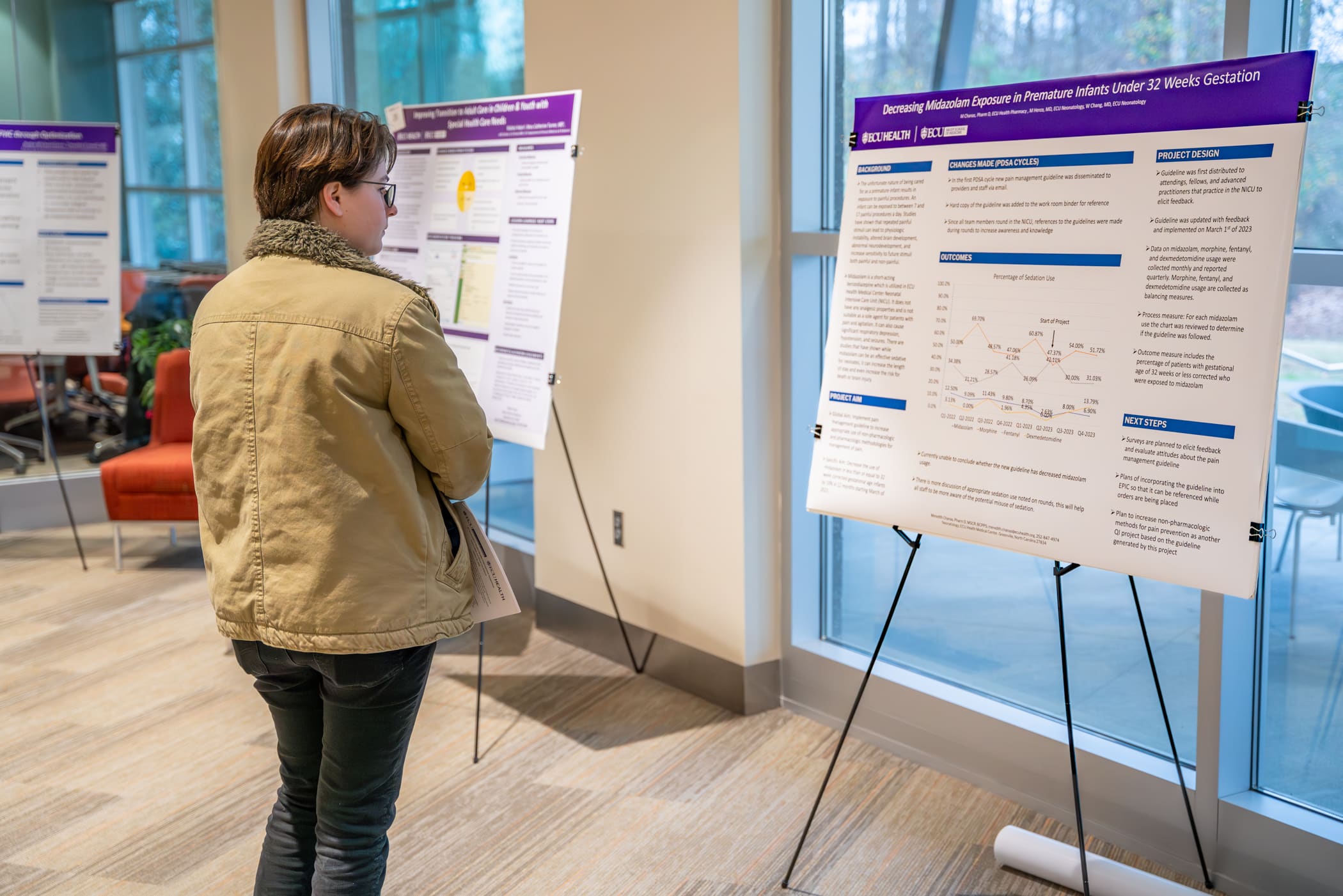
Each year, the ECU Health Quality Improvement Symposium brings together a diverse group of academic and community physicians, health professionals, health care teams, residents, fellows and students from the Brody School of Medicine at East Carolina University to present their work to an audience of peers and health system leaders.
On Wednesday, Jan. 31, ECU Health and ECU’s Brody School of Medicine hosted the eighth annual event at Eastern AHEC. This year’s event was held in-person and virtually, and showcased more than 40 projects related to quality improvement, patient safety, population health and interprofessional practice.
The day kicked off with opening remarks from Dr. Mike Waldrum, CEO of ECU Health and Dean of Brody School of Medicine. After welcoming attendees to the event, Dr. Waldrum expressed his pride in the symposium’s contributions, highlighting the collaborative efforts of teams in addressing regional challenges.

“When I look at these posters and our presenters, I see multidisciplinary, diverse teams coming together to educate, engage in dialogue and drive quality improvement for ECU Health and the patients we serve. I am incredibly proud of our team members and students for their commitment to addressing the immense challenges we face as a region,” Dr. Waldrum said.
Following the opening remarks, selected presenters who were chosen from an application process that took place in late-2023, shared their work with the audience of 178 in-person and virtual attendees.
Presentations were categorized into podium presentations, poster presentations, and works-in-progress poster presentations. Awards for the top three podium and poster presentations were announced in the early afternoon.
PODIUM PRESENTATION:
- Outstanding podium presentation: Erin Atwood, MD, MEd, Department of Pediatrics, Division of Endocrinology, Brody School of Medicine, “Increasing Counseling about the Risk of Hypoglycemia Associated with Alcohol Consumption and Insulin use for Adolescent Patients with Diabetes at the ECU Health Pediatric Diabetes Clinic”
- Honorable mention: Jennifer Stahl, MD, Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Brody School of Medicine, “Right Care at the Right Location: Tele ICU Project”
- Honorable mention: Benjamin Copeland, MD, Department of Pediatrics, Brody School of Medicine, “Improving Mental Health Access for Children in Foster Care in Eastern North Carolina”
QUICK SHOT PODIUM PRESENTATION:
- Outstanding quick shot podium presentation: Juan Guillen-Hernandez, MD, Department of Pediatrics, Brody School of Medicine, “Reducing Unplanned Extubations in the Neonatal Intensive Care Unit”
- Honorable mention: Juli Forbes, MSN, RN, ECU Health Beaufort Hospital, a Campus of ECU Health Medical Center, “Improving Efficiency and Staff Satisfaction in the Operating Room Through a Revised Block Scheduling Framework at a Rural Community Hospital”
- Honorable mention: Titilola Babatunde, BS, MS4, LINC Scholar, Brody School of Medicine, “Improving Documentation of a Pediatric Early Warning Score in the Electronic Health Record”
- Honorable mention: Kate Knowles, MSN, RN, CNL, Management, ECU Health Duplin, “Back to the Basics: Hand Hygiene”
POSTER PRESENTATION:
- First place: John “JC” Rowe IV, MD, Department of Obstetrics and Gynecology, Brody School of Medicine, “Optimizing Outcomes for Patients with First Trimester Bleeding”
- Second place: Gabriella Boccia, MHA, Administrative Fellow, ECU Health, “Improving Sick Visit Clinic Access at ECU Health Physicians Adult and Pediatric Health Care”
- Third place: Stephanie Smith, MSN, RN, ACM-RN, Maynard Children’s Hospital, ECU Health Medical Center, “Improving Fall Risk Identification in Pediatric Patients”
With a total of 15 podium presentations and 29 poster presentations, symposium attendees gained insights into a variety of Quality-related projects. Dr. Waldrum emphasized the importance of what these presentations can offer.
“These presentations cover complex health care problems and this symposium enables us to think deeply about how we can tackle important issues facing our region,” Dr. Waldrum said. “It is always gratifying to see our team members and students come together to demonstrate their expertise and showcase the passion they have for the work they do.”
The symposium closed with two concurrent education sessions led by ECU Health team members:
- Patient Safety, Reliability Science and Root Cause Analysis Application presented by Susan Ingram, MSN, RN CPHQ, Director of Patient Safety
- Fostering Psychological Safety for Team and Quality Outcomes presented by Randy Cobb, DSL, ACC, CPCC, Director of Organizational and Leadership Development
To learn more about the symposium and view a list of presentations, click here.
Dr. Niti Singh Armistead, the chief quality officer and chief clinical officer at ECU Health in Greenville, keeps making the right career choices.
In college at George Mason University, she switched her major from engineering to physics and pre-medicine after she discovered that there were loans available to pay for medical school. “I appreciate what programmers do every day, but I realized that my own joy was working in the medical field,” she says.
After graduating from the University of Maryland School of Medicine, she specialized in anesthesiology, thinking her physics background would be helpful. She switched to internal medicine because she found the long-term relationships with patients more enduring and satisfying.
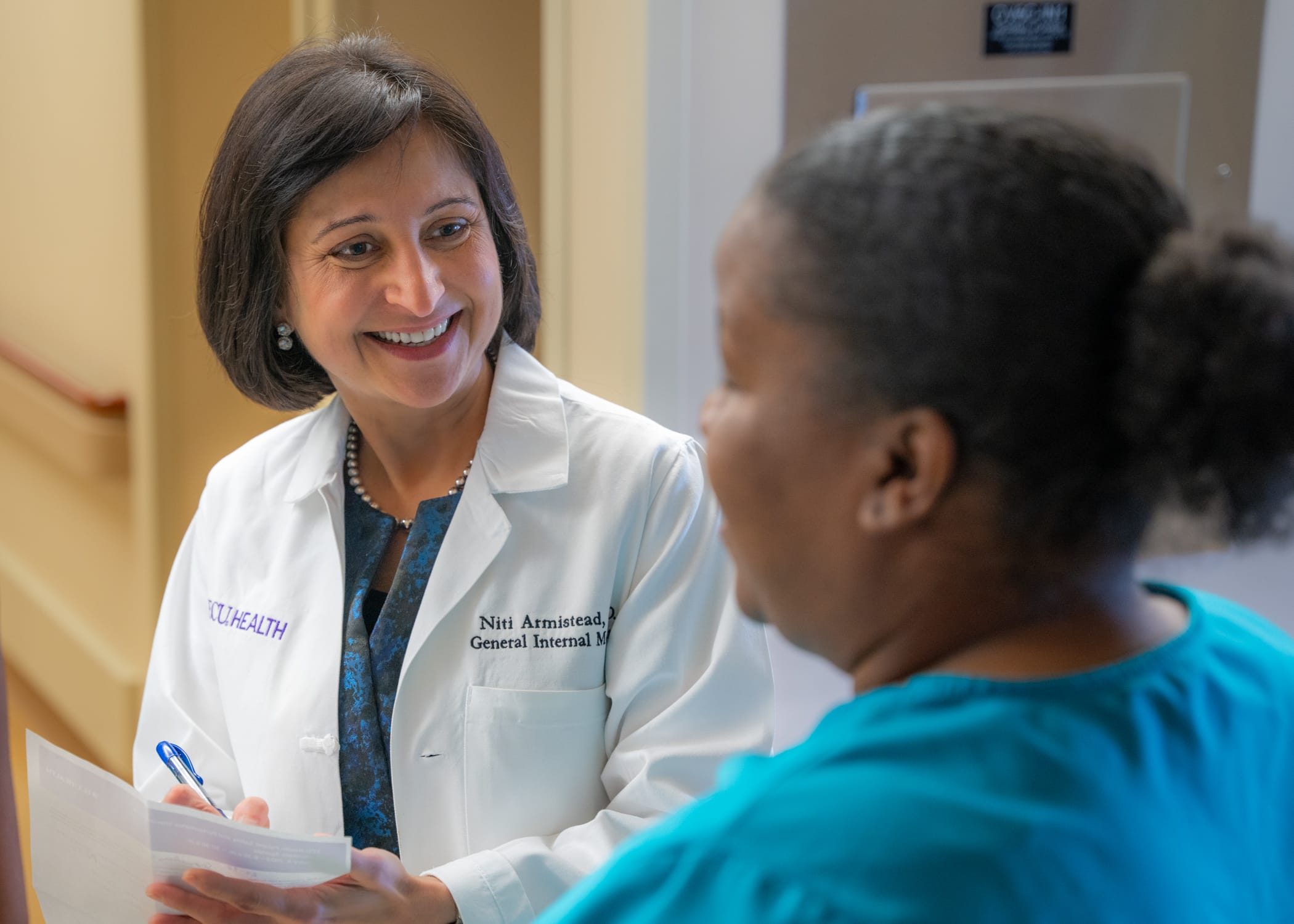
Now, at ECU Health, she’s focused on acute care and still sees patients on a regular basis. She took on administrative roles in 2018 and 2019 before the start of the COVID-19 pandemic, successfully helping steer the healthcare system during a challenging time.
“None of us knew what we were in for,” says Armistead. “For me, it all just kind of came together. How do you support an already underserved population? How do you rise to the occasion as the only healthcare system east of I-95 with an academic arm to do it all, to build the infrastructure for the testing and to educate the community? Those were the kind of interventions I got to lead.”
Read the full story in Business North Carolina.
ECU’s clinical laboratory science students — who after graduation run the nation’s medical labs in hospitals, for public health offices and in the pharmaceutical and biotech industry — got a huge boost recently with the acquisition of a new device that automates the process for identifying blood types.
Funding for the new system, some $6,600, came in part from the American Society for Clinical Pathology and the ECU Medical and Health Science Foundation’s CLS Priority fund.
The instrument, known as the Ortho Clinical Diagnostics workstation, replaces a laborious process of mixing blood samples with reagents by hand to allow laboratory professionals to quickly and accurately establish blood types and identify donated blood that can be safely transfused to a recipient.

Traditional blood analysis methods, which ECU’s Department of Clinical Laboratory Science chair Dr. Guyla Evans and her faculty peers still teach their students, involves mixing drops of blood with antibodies that register specific blood types. The process also registers Rh factor, proteins on the surface of some people’s blood cells that affect who can receive blood donations from whom.
Using the established test tube method is a time and attention intensive process.
“It can be kind of hard to teach students how to read the tubes because it’s subjective. You have to read the tubes right away, and there are a lot of steps,” said Michael Foster, a senior from Roanoke Rapids, who already works in the blood bank at ECU Health Medical Center in Greenville.
Using test tubes to identify blood samples is a tricky business: laboratory personnel must identify cell reactions by eye and they have a limited time to observe and interpret the results.
“The name of the game in blood banking is accuracy, but it’s also speed. You want to get it in the centrifuge and as soon as it’s ready to come out of the incubator and get it going,” Evans said.
The new system uses a cartridge, which requires less blood in the sampling process and has the advantage of leaving the sample readable by technicians for up to 24 hours. This allows laboratorians to double check their work or have a peer review their results.
An added benefit for the cartridge system is baked-in surety of the testing chemicals.
“You don’t have to worry about adding the wrong reagents because the cards are color-coded and the reagents are already added in,” Foster said.
Each cartridge may cost up to $25, which isn’t cheap, but Evans and Lorie Schwartz, a research technician and CLS instructor, both agree that the new system is at least as cost effective as traditional testing methods due to labor costs and the intangible benefit of assurance that the results are valid.
The new system is less mentally taxing for the medical laboratory scientist, Evans explained.
“In the blood bank, everything has to be carefully documented. Nothing is ever assumed or taken for granted—blood bankers trust no one, they believe no one,” Evans said. “If I’m going to do a cross match for two units, and the antibody screen and the blood typing, that’s 12 to 15 tubes that I have to label every time. It’s a lot faster to label one card or a couple of cards, depending on what testing you’re doing.”
The CLS department received the equipment in December, just a bit too late for the current class of students, including Foster, who will graduate in May. The seven graduating students were able to train on the gel microcolumn system during clinical rotations with ECU Health and Nash UNC Health, where they got hands-on experience.
Evans said the COVID-19 pandemic made teaching blood banking techniques very difficult because, while theory is crucial to understanding lab work, getting hands-on training is critical for learning.
Students who learned during the pandemic were dropped into the deep end during clinical rotations in working labs and had to put theory into practice, both with traditional test tube methods and the gel cartridge system.
“During clinicals, we went through quite a number of cards trying to figure out what antibodies were present in the blood because they would give us unknown samples and we would spend the entire eight hours trying to figure out what the sample was,” said Bryce Glover, a senior from Fayetteville. “If we went down the wrong path, that was one card wasted.”

Because they are eligible to work in clinical labs once their clinical rotations were completed, Foster, Glover and the other members of their cohort already have jobs in area labs.
“ECU Health and ECU’s commitment to incorporating the latest technologies into both health care delivery and hands-on training for our future workforce not only benefits students during their academic journey but also equips them with valuable skills that are highly sought after in the health care industry,” said Carolyn Merritt, ECU Health lab scientist.
“Keeping students up to date on the latest technologies, such as gel testing, is crucial for optimizing their limited time during clinical rotations. Our goal is to help prepare the next generation of high-quality health care professionals, and hands-on experience with innovative technology ensures our students are well equipped to provide important services once they enter the workforce,” Merritt said.
The advances in high tech equipment, combined with severe staffing shortages, have exacerbated what Evans sees a worrying trend — laboratory professionals aren’t seen on the hospital floors or interacting with nursing staff.
Being squirreled away in a windowless lab the majority of the workday means that medical laboratory scientists and technicians are often disconnected from their peers. Evans counsels her students to be part of the hospital and medical communities they will eventually be part of.
“They must make an effort to be seen as part of the hospital team because they usually aren’t seen,” Evans said.
While medical laboratory scientists might not be as visible as other members of the health care continuum, their role in diagnosing and treating patients can’t be overstated. With an expected need of nearly 17,000 more medical lab scientists nationwide by 2032, the critical skill set that Pirate graduates bring to hospitals and clinics is invaluable.
“When our students get into the clinical system, that’s when they really see the workflow and that last piece of their education comes together,” Evans said. “We’ve been really fortunate that our clinical sites, even though they know they’re dealing with personnel shortages, are taking students on which is extra work they don’t get compensated for. They’re doing it because they know it’s important and that is invaluable.”
Sharon and Steve McNally of New Bern have been married for more than 40 years. Now, Steve carries a little piece of his wife Sharon with him everywhere he goes.
Steve is diabetic and in 2015, he went through his first round of transplants at a hospital in their then-home state of Pennsylvania.
“It was supposed to have been a kidney and pancreas at the same time,” Steve said. “When they got me on the operating table, the pancreas wasn’t viable. So they said, ‘We’re going to do the kidney alone and we’ll get you a pancreas.’ What happened then was the hospital eventually became decertified and couldn’t do pancreas transplants anymore.”
Then, they joined the transplant list with a health system in Maryland and Steve received a pancreas transplant 30 days later. In the meantime, the new kidney had been damaged due to the lack of a functioning pancreas, but Steve said it was largely working fine until mid-2023. By that time, the McNallys had moved from Pennsylvania down to New Bern.
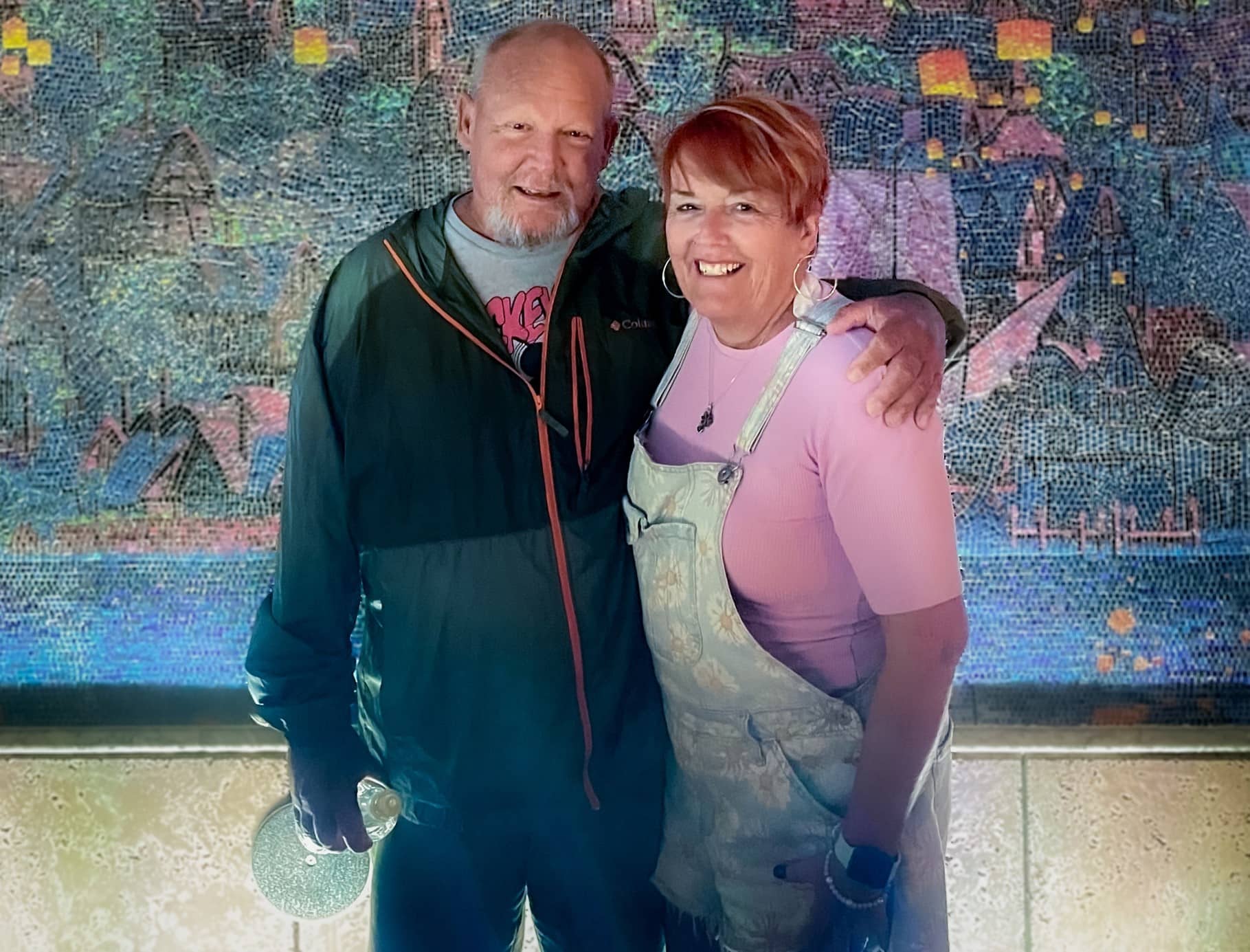
With Steve’s kidney function worsening, there was little time to spare. He could join another transplant list that may take eight to 10 years to find a donor, start dialysis or personally find a match to donate a kidney.
Sharon said she knew she had to step up for her husband and get tested to see if she could be a match.
“It wasn’t really hard for me because a lot of people say, ‘Oh my gosh, you’re so amazing’ or so this and that but I don’t really feel that way,” Sharon said. “I feel like we’ve been married 40 plus years. We have grandkids and kids together and how could you watch someone get more and more ill and not do something if you can? So I didn’t really think about it.”
Testing started for the two in June and preparation began right away. They found out in October they were a match and an ECU Health team performed the transplant on Nov. 7.
“I’m glad that this was something I could do,” Sharon said. “There’s a lot of people that probably couldn’t have, even if they wanted to.”
For Sharon’s part, she went home the next day while Steve stayed a couple extra days for monitoring before heading home. While they each needed some help early on after coming home, they were both happy to support each other, as they’ve been doing for more than four decades.
Dr. Margaret Romine, transplant surgeon at ECU Health, and Dr. David Leeser performed the transplant along with other members of the ECU Health transplant team. She said she was most proud that the team could take on a case like the McNallys, especially given Steve had been through a kidney and pancreas transplant previously.
“They had already been through a lot before even coming to us but they had such great attitudes and were great patients to care for,” Dr. Romine said. “We have such a great team and that really sets us apart from other programs. It’s not just about what the surgeon thinks – the nephrologists play a huge role. Our coordinators, nurses, pharmacists, social workers all play a huge role. We can’t do what we do without the entire team. Whenever we make a big decision to take on a patient like him, it’s done as a team.”
Steve and Sharon both said they were happy with their experience at ECU Health and shared appreciation for the care team that helped guide them through the process and into recovery.
Now, they are looking forward to a spring working outdoors, something they both love but missed out on last year.
Sharon said if she could share one message, it would be on the importance of organ donation.
“Organ donation is just such a wonderful thing. I mean, three different times it saved my husband,” Sharon said. “You know, a lot of people don’t want to do something like that even after they’re gone because it just it seems weird to them. But honestly, I think it’s a wonderful thing.”
NAGS HEAD, N.C. — Jan. 30, 2024 — Outer Banks Health is proud to announce the opening of the Carol S. and Edward D. Cowell, Jr. Cancer Center, a 15,000 square-foot, state-of-the-art facility made possible through the collaboration of Outer Banks Health, ECU Health, Chesapeake Regional Healthcare and the generous support of the Outer Banks community. The center opened its doors to patients on January 29, 2024.
This momentous occasion marks the culmination of years of dedication, perseverance, and community support. Outer Banks Health initiated the endeavor in 2015 with a vision to create a cutting-edge facility that would serve as a beacon of hope and healing for cancer patients on the Outer Banks and the surrounding region.
“The completion of the Cowell Cancer Center was made possible through the unwavering determination of the Outer Banks Health Development Council,” said Ronnie Sloan, FACHE, president of Outer Banks Health. “The council is comprised of dedicated individuals who share a passion for enhancing healthcare in the region and it played a pivotal role in bringing this ambitious project to fruition.”

Led by radiation oncologist, Charles Shelton, the new center boasts a dedicated team, including a director, radiation therapists, a radiation nurse, a genetics extender, a physicist, a dosimetrist, pharmacists and pharmacy technicians, LPNs and RNs, lab technicians, navigators, a social worker, a practice manager, and patient access representatives. While the search for a permanent medical oncologist continues, Dr. Michael Spiritos, formerly of Duke Health, has agreed to serve in that capacity on an interim basis along with Dr. John Barton. Katie Caton, FNP is also on staff as a permanent provider.
Of the 1300 critical access hospitals nationwide, Outer Banks Health Hospital is one of only eight accredited by the Commission on Cancer of the American College of Surgeons and is also distinguished as the only one in the country with an accredited breast program. This notable achievement reflects the commitment of Outer Banks Health to maintaining the highest standards of cancer care.
Outer Banks Health remains focused on expanding its list of services and programs to meet the evolving healthcare needs of the community. The organization’s goals include delivering excellent care locally and collaborating with health organizations throughout North Carolina and Virginia to ensure residents and visitors can access the best possible care.
For more information about the Cowell Cancer Center or to inquire about services, visit OuterBanksHealth.org/services/cancer-care or call (252) 449-7272.
Greenville, NC — Yaolin Zhou, MD, associate professor of Pathology and Laboratory Medicine at the Brody School of Medicine at East Carolina University, director of Quality and Test Utilization, and head of Molecular Pathology at ECU Health, was named to the 2023 Becker’s Hospital Review “Emerging Leaders: Provider Organization Leaders Under 40” list.
The Becker’s Hospital Review list recognizes up-and-coming leaders who are quickly rising through the ranks at their organizations, focusing on development, innovation, and improved outcomes.
The “Emerging Leaders: Provider Organization Leaders Under 40” list honors leaders who are 40 years old or younger for their commitment to optimizing health care. The Becker’s Hospital Review editorial team accepted nominations for this list and curated it to highlight the accomplishments of these rising stars.
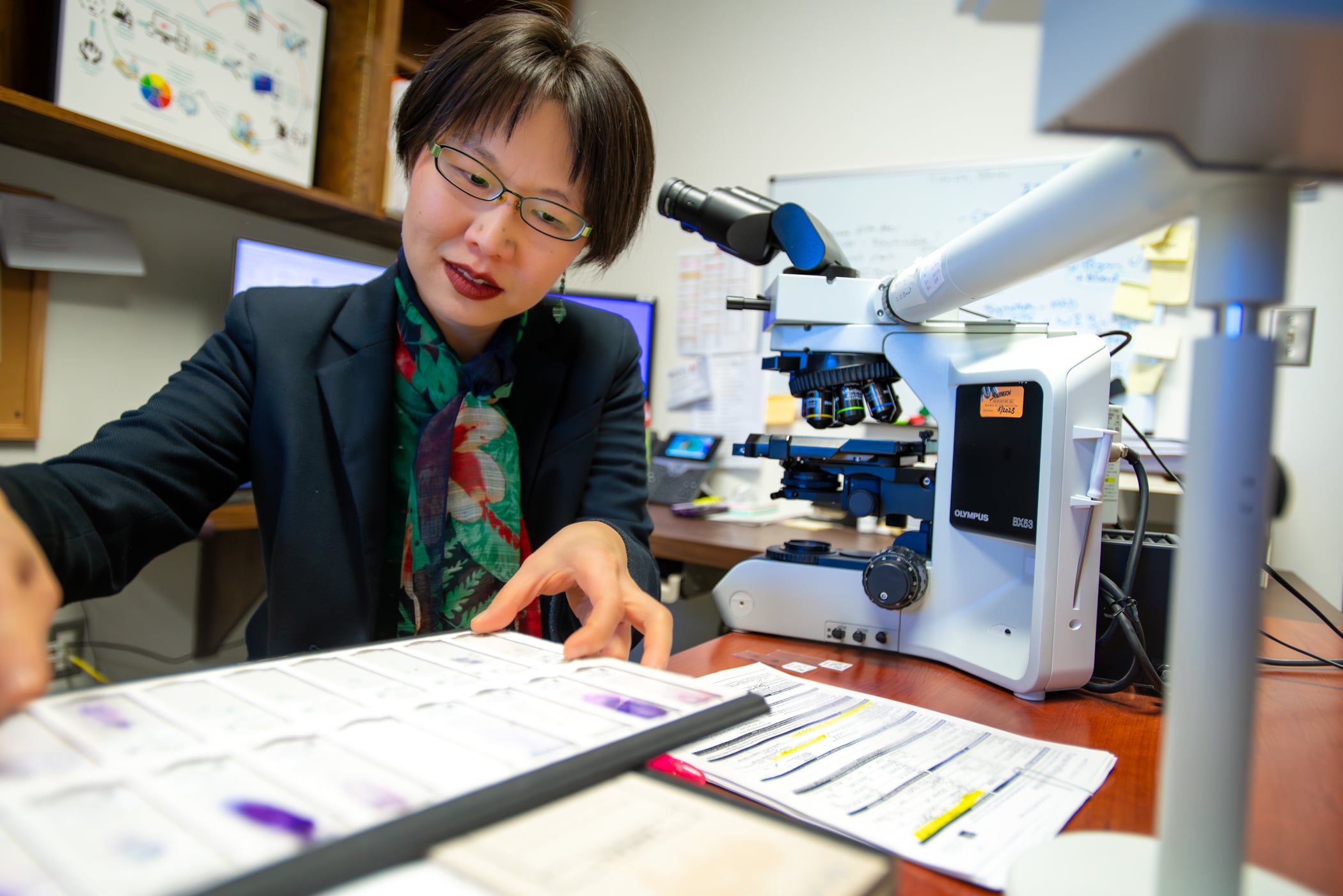
Dr. Zhou trained at some of the most prestigious institutions in the world and chose to come to ECU Health to help address some of the most challenging problems in health care delivery. As the only molecular pathologist in ECU Health’s 29-county service area, she provides expertise that benefits more than 1.4 million individuals in the region.
“ECU Health is proud to have Dr. Zhou, a nationally recognized molecular test utilization expert, whose work exemplifies the vital connection between research, education and effective health care delivery,” said Dr. Michael Waldrum, ECU Health CEO and dean of the Brody School of Medicine. “Dr. Zhou’s expertise shapes innovative clinical solutions, addressing unique barriers in rural populations. I am grateful for leaders like Dr. Zhou who are helping to create a healthier present and future for eastern North Carolina.”
Since her arrival in 2020, Dr. Zhou established an innovative molecular consultation service, focused primarily on pre- and post-testing review, to ensure cancer patients receive appropriate molecular tests and treatment. In 2023, she secured a $250,000 industry-funded quality improvement grant to expand her molecular consultation services across practices in eastern North Carolina’s rural 29-county region. This grant aims to identify and address health care disparities in cancer care, ultimately improving patient outcomes.
In addition to her molecular expertise, Dr. Zhou is an internationally recognized quality improvement and test utilization expert. In 2020, she partnered with clinical colleagues to establish a health system-wide initiative to reduce daily repeat lab tests, achieving a 15 to 25 percent reduction in unnecessary repeat daily testing throughout the system. For this multi-specialty and multi-disciplinary collaboration, Dr. Zhou and her team were honored with the prestigious American Society for Clinical Pathology Choosing Wisely Champion Award.
Dr. Zhou is active as a teaching and clinical faculty member and a bioethics and quality improvement instructor at Brody and for ECU Health. She also represents eastern North Carolina on the board of directors for the Association for Molecular Pathology (AMP), the world’s largest association for molecular professionals. Dr. Zhou recently authored an invited guest editorial in the Journal of Molecular Diagnostics, the official AMP journal. This editorial, based on her grant work, presents a national solution to reduce barriers in precision oncology.
“As a cancer survivor myself, I strive to bring quality and equitable cancer care to those I am honored to serve,” said Dr. Zhou. “All patients deserve high-quality and guideline-recommended cancer treatment. Through this recognition, I hope we can bring greater visibility to how we are addressing disparities in cancer care in our patients. Through collaborative efforts, we can develop solutions for providing equitable cancer care on a broader scale – and it starts here in eastern North Carolina.”
NAGS HEAD — About a decade ago, the Outer Banks community suffered higher cancer mortality rates than the state and nation. Not only has that trend reversed, but now for the first time, local cancer patients can receive all their services under one roof.
Over 275 people attended the ribbon-cutting and open house on Jan. 24 for the Carol S. and Edward D. Cowell, Jr. Cancer Center. Located at 4927 S. Croatan Highway in Nags Head, it opens its doors to patients on Jan. 29.
“In 2012, Outer Banks Health didn’t have a cancer services program at all, and we were trailing the state and we were trailing the nation when it came to cancer mortality for all cancers…and we wanted to change that dynamic,” Ronnie Sloan, president of Outer Banks Health, said during brief event remarks.

The Outer Banks’ cancer mortality rate was about 6% and 7% higher than the nation and the state, respectively, Sloan said in an interview at the event.
Now, local cancer mortality rates are 6-7% lower than the state and country. The 5-year mortality for breast cancer rate dropped 50% in recent years. Even as cancer mortality rates have steadily declined across the country, “we’ve outpaced that,” Sloan said.
Carol Cowell cut the ribbon at Wednesday’s event. She made the namesake donation to the Carol S. and Edward D. Cowell, Jr. Cancer Center in Nags Head in honor of her late husband and in appreciation of the local community.
Originally from Brooklyn, New York, Cowell said in an interview that she is a cancer survivor who received treatment in Elizabeth City in 2005. The Outer Banks didn’t offer cancer services then, but she was greatly impressed by “the community sense that you got” from local health care professionals and from the community at large.
Fundraising for the center was similarly a community effort.
“This has been just an amazing journey,” Tess Judge said during her event remarks. Judge is chair of the board of directors for Outer Banks Health and co-chaired the fundraising team with Cindy Thornsvard.
Judge said she lost her mother and a son-in-law to cancer, and her daughter-in-law is struggling with it now, “so cancer services and the wonderful team we have here is just so special not only to me but to many.”
Fundraising for the center began during COVID, and their original goal of $4 million was bumped up to $6 million as the costs of building supplies soared.
According to Sloan, nearly $6.5 million has been raised for the center.
“We did that because of all of you, and the tremendous support this community has given to this cancer center,” Judge said.
Stephanie Anderson, a community member who had lost people to cancer, hiked the entire Appalachian Trail last year and raised about $10,000 for the center in the process, said Jennifer Schwartzenberg, director of community outreach and development for Outer Banks Health.
The journey to the center
Outer Banks Health hired its first director of cancer services in 2012, said Sloan, who came aboard in mid-2011.
“In 2013, the board of trustees made a fantastic decision,” Sloan said during his public remarks. They chose to purchase the radiation therapy center that was closing about two miles north of the hospital.
“We didn’t want our community to have to drive two hours each way” for treatment, he said.
Dr. Charles Shelton, a radiation oncologist, began working at Outer Banks Health — then called The Outer Banks Hospital — in 2014, and he leads the cancer services team, Wendy Kelly, marketing director for Outer Banks Health, said in an email.
Shelton set a goal of creating and maintaining an accredited cancer program to reduce the high cancer mortality rate among residents of Dare and Currituck counties, Kelly said.
“It’s been a dream of this organization since 2015 to build a facility that would allow patients to receive the highest-quality, compassionate cancer care all under one roof right here on the Outer Banks,” Kelly said.
Supported by its two partners, ECU Health and Chesapeake Regional Healthcare, along with the generosity of the local community, “that dream is now a reality,” she said.
In 2016, the Commission on Cancer of The American College of Surgeons granted a “Three-Year Accreditation with a Commendation” to The Outer Banks Hospital, which the facility has “proudly maintained” since that time, according to Kelly.
“Additionally, we are one of only eight critical access hospitals in the nation with this accreditation, and the only one nationally to have an accredited breast care program,” she added.
Outer Banks Health is one of 20 critical access hospitals in North Carolina, which have 25 beds or fewer and receive cost-based reimbursement, according to the North Carolina Division of Health and Human Services website.
“Outer Banks Health is an approved Medicare and Medicaid provider and participates with most commercial insurance companies,” Kelly said.
Sloan said that the new “comprehensive center” allows them to offer the “best care possible.”
The entire cancer team can quickly make decisions about patients in consult with one another as “concerns pop up,” and having the dedicated center eliminates the need for patients to go from the first to second floor of the hospital for care, then across the busy bypass for radiation treatment, he said.
Kelly expressed gratitude for all the community support of the center, which included the over 275 people who attended the event on Wednesday.
In addition to Shelton, the cancer services team also includes a director, three radiation therapists, a radiation nurse, a genetics extender, a physicist, a dosimetrist, a licensed practical nurse, 11 registered nurses, a nurse navigator, a financial navigator, a lay navigator, a social worker, a practice manager and three front desk monitors, according to Kelly.
“Our search continues for a permanent medical oncologist, and in the interim Dr. Michael Spiritos, formerly of Duke Health, has agreed to serve in that capacity,” Kelly said in her email. “Additionally, Dr. John Barton serves as a medical oncologist at the center.”
“Congratulations Outer Banks Health on this much-needed and impressive expansion,” Robert DeFazio, chairman of the board of directors for the Outer Banks Chamber of Commerce, said during his event remarks.
Greenville, N.C. – As part of its continued evolution to become the national model for rural academic health care, ECU Health today announced new leadership roles and responsibilities intended to further enhance the organization’s transformation as a rural health care leader.
Effective Feb. 5:
- Brian Floyd, RN, MBA, will dedicate his efforts to his role as ECU Health’s chief operating officer (COO), providing strategic oversight of the health system enterprise and its day-to-day operations. He will have heightened focus on creating seamless interoperability within the health system and ensuring we are operating, performing and providing care as one team.
- Jay Briley, MHA, FACHE, current president of ECU Health Community Hospitals, will transition to president at ECU Health Medical Center, reporting directly to Floyd as COO.
- Van Smith, MBA, MSHA, current executive vice president of ECU Health Medical Center, will transition to president of ECU Health Community Hospitals, reporting directly to Floyd as COO.
Additionally, Tara Stroud, DNP, APRN, NNP-BC, NEA-BC, current senior administrator of Children’s Services at Maynard Children’s Hospital, will become vice president for Maynard Children’s Hospital, Women’s Service Lines and Community Health Programs upon Kim Crickmore’s retirement departure date of Feb. 26.
“These leaders’ unique expertise in driving operational and clinical excellence, financial stewardship and leading complex health care environments are at the forefront of these proposed – and ultimately enthusiastically embraced – leadership appointments,” said Dr. Michael Waldrum, CEO of ECU Health and dean of the Brody School of Medicine at East Carolina University. “I look forward to working closely with these leaders and remain focused on steering the enterprise toward our vision, including strengthening our academic mission, advancing our synergies as well continuing to build partnerships across the state.”

Brian Floyd

Jay Briley

Van Smith

Tara Stroud
Frostbite isn’t the only concern with the frigid temperatures expected in eastern North Carolina this weekend.
“You can’t smell it. You can’t see it. You can’t taste it,” said ECU Health Chief for the Division of Medical Toxicology Dr. Jason Hack
Dr. Hack said carbon monoxide poisoning can sicken people when their furnaces malfunction or they use other means to heat their homes.

He said that includes, “HVAC, our heaters in our home. Portable heaters, propane portable heaters that some people might bring in, or if they lose their electricity because of an ice storm or something along those lines, they might want to bring in a generator out of the storm or close to the home.”
Dr. Hack also said people should never sit in a running car to escape the cold if the heat is out at their home.
“Some people would tend to sit in their car and turn on turn on their vehicle while it’s still in their attached garage,” he said, “Even with the door open, these can be sources of enough carbon monoxide to injure or even, unfortunately, kill people within the home itself.”
It’s not a good idea, but a dangerous one, to use the gas stove in your kitchen to warm up the house. Dr. Hack said, “It could be producing low levels of carbon monoxide that might accumulate.”
And the symptoms of carbon monoxide poisoning can be non-specific.
“It can look like a lot of other things,” he said, “Such as weakness or dizziness. Some people complain of some shortness of breath. Headache is one of the most common presenting symptoms of carbon monoxide. Confusion. Some people actually complain of chest pain or palpitations and fainting.”
Dr. Hack said the best defense is a working carbon monoxide detector in every bedroom and living space in the house; he recommends that people to make sure the batteries are fresh and they’re working properly before the cold air arrives this weekend.
According to the National Institutes of Health, about 1,200 people die in the U.S. from accidental CO poisoning annually and more than 100,000 people visit the emergency department each year.

