Younger people are increasingly suffering from strokes according to medical experts at ECU Heath. While risk of stroke increases with age, health care teams have seen an increase in strokes in young people, partly due to a combination of COVID-19, an increase in consuming processed, sugary and fatty foods as well as smoking and vaping.
“With COVID-19, we have noticed an increase in strokes, especially in younger populations,” said Dr. Shailesh Male, stroke medical director, ECU Health Medical Center. “During the peak of the pandemic, my colleagues and I noticed that young patients who do not have vascular risk factors were having strokes. COVID-19, like other infections, increases the risk of forming blood clots and, in turn, can lead to higher risk of strokes.”
Strokes are considered the heart attack of the brain. A stroke occurs when a blood clot compromises blood flow to the brain. This leads to loss of brain function, manifesting in symptoms including: weakness or numbness on one side of your body, slurred speech or difficulty understanding others, blindness in one or both eyes, dizziness and/or a severe headache.
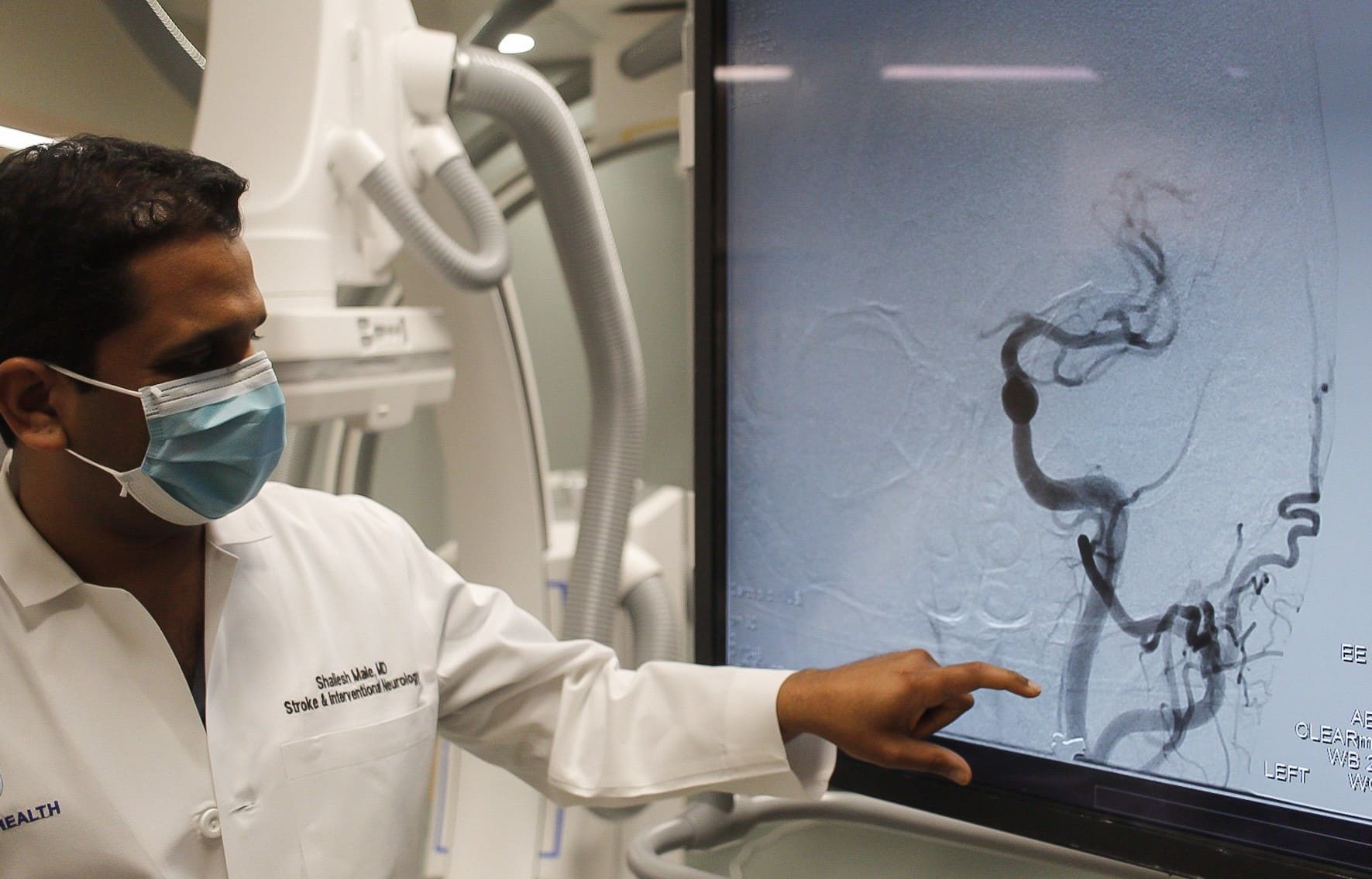
Risk factors for stroke can be broken down into two categories: modifiable and non-modifiable.
“We like to focus on the modifiable risk factors, the ones that you can change,” said Dr. Male. “These include hypertension, cholesterol, diabetes, smoking, physical inactivity and obesity.”
The increase in younger people having strokes are mostly attributed to modifiable risk factors. The rise in popularity of e-cigarettes and vaping has largely been in younger populations. Smoking reduces the amount of oxygen in the blood, makes the heart beat faster and raises blood pressure. Additionally, younger people are generally less healthy than previous generations in terms of diet and exercise.
“Processed, fatty and sugary foods are increasingly becoming a regular part of our diets at a younger age,” said Dr. Male. “This combined with an inactive lifestyle increases almost all risk factors including obesity, diabetes, high blood sugar, hypertension and high cholesterol.”
Non-modifiable risk factors include older age, gender (men face higher risk of stroke), family history, genetics and even race. According to The Office of Minority Health, African Americans are 50 percent more likely to have a stroke than non-Hispanic whites adult counterparts and 70 percent more likely to die from a stroke.
“African Americans have higher incidences of hypertension, diabetes and high cholesterol, which in combination, increases the risk of strokes,” said Dr. Male.
It is important to discuss risk factors with your primary care provider. If you have had a stroke, your doctor may prescribe preventative medications to address risk factors like blood thinners, cholesterol medication or blood pressure medication. Additionally, lifestyle changes such as exercising more and eating healthier foods are proven to lower your risk of stroke.
“With great treatment options now widely available, it is important to remember, time is of the essence,” said Dr. Male. “The sooner we implement treatment, the better the odds that the patient will recover to their baseline. The benefit of early treatment is preventing long-term disability.”
If a stroke is not caught quick enough, long-term disability and health issues are possible. Most commonly, patients may lose strength on one side of their body or have problems speaking.
The acronym B.E. F.A.S.T. can help quickly identify the signs and symptoms that you or a loved one may be experiencing a stroke:
- B – Balance problems
- E – Eye issues like blindness or seeing doubles
- F – Face drooping
- A – Arm weakness
- S – Speech slurring
- T – Time to call 911
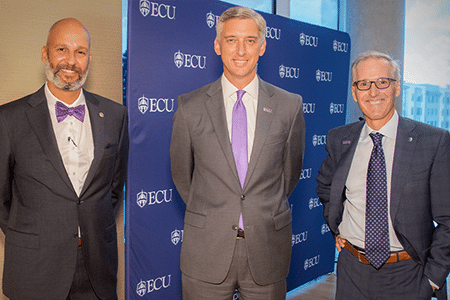
Dr. Mike Waldrum, ECU Health CEO and dean of the Brody School of Medicine at East Carolina University was recently named to Business North Carolina’s 2022 Power List. ECU Chancellor Dr. Philip Rogers was also named to Business North Carolina’s 2022 Power List in the Education section.
This yearly list names the most influential leaders in the state of North Carolina across various industries. The awarded leaders are nominated for this list based on their influence as strong leaders.
“This recognition represents the tireless work ECU Health team members do every day to serve the region and educate the future physicians for North Carolina,” said Dr. Waldrum. “At ECU Health, we strive to become a national model for rural health delivery by providing high-quality care to the region we proudly call home. Our regional health care organization, combined with the Brody School of Medicine, strengthens our shared mission to improve the health and well-being of eastern North Carolina. ECU Health will continue to innovate and provide high-quality care to those we serve.”

We are proud to have strong leadership moving ECU Health forward to meet the joint mission of improving the health and well-being of eastern North Carolina by training the providers of tomorrow, collaborating with community partners to solve complex issues and bringing clinical innovations that improve the lives of those who proudly call this region home.
To read the Business NC Power 100 List article, please visit https://businessnc.com/2022-power-list/.
It’s a natural evolution for two organizations that have worked together for years.
“This announcement has been 40 years in the making,” said Dr. Michael Waldrum, Vidant Health CEO and dean of East Carolina University’s Brody School of Medicine.
“We are super excited for this name change, said Vidant team member Carol Ramirez, RN. “I think it’s going to be a really, really good change for eastern North Carolina.”
“This is not a moment to sit idle,” said ECU Chancellor Philip Rogers, upon the announcement of the joint operating agreement in January 2022. “It is instead a moment to launch an innovative solution for rural health care delivery and education in eastern North Carolina. And that is exactly what we aspire to do with this announcement.”
With a logo reveal that followed in April and a transition to ECU Health that will begin in May, it is an exciting time for eastern North Carolina.
“As with any change, there is a lot of angst about ‘what’s the future for me as an individual within the organization,’” said Jason Higginson, executive dean of the Brody School of Medicine at ECU. “I think one of the key things, our guiding principal, is the people within the organization are equally important to achieving the mission as anything. So, as we look to the future, we are trying to ensure that everyone in the organization is valued and that their contributions are honored.”
It’s a process that will take months to complete. The Vidant Health logo will be phased out over the next two years, replaced by ECU Health on everything from building signage and vehicles to organizational websites and social media channels.
“There is a plan to roll that out,” said Dr. Waldrum at the logo announcement in April. “And today we are showing the brand but beginning in May you’ll start seeing that happen and that will evolve over time.”
These changes will unfold across hundreds of locations in 29 counties. A visual unveiling of a forward-focused partnership benefitting those who serve — and are served by — the health system and the Brody School of Medicine.
“I think it’s awesome that two of the biggest entities here in town have collaborated to support and help the whole eastern North Carolina,” said Vidant team member and social worker Robinque Willis-Brown. “So together, I know they can make a great difference.”
In 2000, Millie Shinn developed an ulcer on her right heel. A complication of Shinn’s Type 1 diabetes, the ulcer continued to grow, requiring Shinn to seek treatment and ultimately, a heel reconstruction.
When that did not heal properly, she said she knew amputation was a possibility, though she wasn’t willing to accept it yet. Fast forward to February of 2002 and Shinn was still in bandages from the surgery. After a trip to the Emergency Department, Shinn met with her doctors and they decided it was time to amputate her right leg below the knee.
“My husband was with me and even the nurse that was taking care of me, we were all just bawling before the surgery,” Shinn said of her experience before her first amputation at Vidant Medical Center (VMC). “It was not something that I thought would happen to me … I really wasn’t sure what to expect.”

She said she was motivated after her first surgery to get moving and was lucky to have the opportunity to use an early post-operative prosthesis, or EPOP, which helped her to get out of bed and moving around on a prosthetic limb sooner than she would have without one.
The EPOP was used while she was still healing and about three months after her first surgery, she was fitted with a permanent prosthetic limb. In September of the same year, ulcers began to show up on her left foot. She knew right away how it would end.
She asked what her options were and her providers told her they could continue to clean her ulcers and try to heal her foot for as long as possible. But she told the doctors to move ahead with amputation again.
“I said, ‘I’ve done fine with one fake leg, I’ll be fine with two.’ And that’s what we did,” Shinn said. “It was not circulation issues, it was nerve issues. Circulation was always good I just didn’t have any feeling and had lots of nerve damage.”
Her left leg amputation was also a below-the-knee amputation and she said, like her first amputation, she recovered quickly. Since she knew what to expect the second time around it was not as traumatic an experience—for her. It wasn’t as easy for her son to accept, and at that time, there was not an amputee support group in eastern North Carolina.
Eastern North Carolina Amputee Support Group

Vidant’s amputee support group, officially called Eastern North Carolina Amputee Support Group, came together for the first time in March of 2006 thanks in large part to Shinn and Helen Houston, an occupational therapy clinical specialist at Vidant Medical Center.
Shinn, who lives nearly two hours away from Greenville and made the drive monthly to help lead the support group, said the first meeting had about eight people. The numbers and traditions have grown along the way, and 16 years later the group continues to meet. COVID-19 means they connect virtually on the third Monday of each month from 4:30 to 5:30 p.m.
Shinn said she estimates that nearly 500 people have joined a meeting a one time or another. She has seen the importance of the meetings for her fellow amputees, especially those in the early stages.
“I think it’s very important because they can see us and realize that there is a life afterwards,” Shinn said. “Yes, it has changed my life and yes this is like a death in your family and a death to you because you’ve actually lost a part of yourself. It’s going to be a part of your life, but it doesn’t have to be a controlling part of your life.”
Houston said she has loved her time participating in the group and looks forward to the meeting each month and interacting with people she now considers family. Houston has also helped lead the group since its inception.
She said the conversations each month are inspiring to her and a reminder of why she chose a career in therapy.
“It’s my responsibility, together with recreational therapy, to bring the people that have had recent amputations and are in rehab right now to the group,” Houston said. “We let them see other people that are a little further along than them and let them ask questions. I can answer their questions all day, but I have two legs, so my experience carries limited weight.”
The group frequently has guest speakers including doctors, massage therapists, highway patrol officers, politicians and prosthetists. Shinn said sometimes people will join the group just once to get a few answers to questions that they have and will not return, but she said that as long as people are getting the help they need, the group feels like it is doing its job.
Houston and Shinn both recalled how meaningful it is to include caregivers, family and friends of amputees in the support group sessions. They even shared that in a few cases, after an amputee has passed, spouses and friends continue to attend the sessions to share their insights and past experiences with the group.
“It’s really neat and it’s become like a family,” Houston said. “For me, who is from South Africa, and who doesn’t have family here, to see the same people every month for 16 years, they know me better than I know myself. We’ve been through all kinds of stuff together.”
Occupational Therapy Month
Along with Limb Loss and Limb Difference Awareness Month, April is also Occupational Therapy Month. While occupational therapists play crucial roles in many areas across the health system, supporting amputees is a special responsibility.
Houston said in the acute care setting, occupational therapists are often the first people helping to get amputees out of bed. From there, it’s about teaching patients how to do all the things they are used to doing, but in a different way. This includes bathing, dressing, grooming, transferring to and from a toilet, and to and from a tub.
She said patients typically need three months for their wounds to heal and their residual limb to be shaped, before they get a prosthetic limb. They would initially be at a wheelchair level—or wheelchair and walker level—for some time during their recovery.
“In inpatient rehab, amputees practice self-care tasks, but they also address what we call instrumental activities of daily living,” Houston said. “That is not just self-care but also taking care of the things in your environment. So that would be things like cooking, grocery shopping, money management, medication management, yardwork and starting to access the community, including returning to driving.”
She described the stages after this as getting people back to doing whatever occupied their time before their amputation and educating them on different ways to do so. Houston mentioned a study of healthy adults that showed it takes at least two days to regain strength from each day spent lying in bed.
“That’s for someone who has not had surgery and has not had anything wrong with them,” Houston said. “So here at Vidant we help to get patients up the day after surgery. You’re trying to prevent blood clots, and help them mentally adjust to their new life. The longer you lay there and are fearful of ‘How am I going to get up and how am I going to do this?’ the bigger the mountain seems.”
Houston said her experiences with amputees are often the most inspiring.
“It’s really neat. It’s an honor to be part of their journey,” Houston said. “To be a part of one of the patient’s hardest times in their lives and be able to support them and show them a little further down the road, makes coming to work every day extremely rewarding. To be able to show them that they’re not the only ones in their current situation and to help them to problem solve how they’re able to get back to doing whatever is important to them – that is why I became an occupational therapist.”
Resources
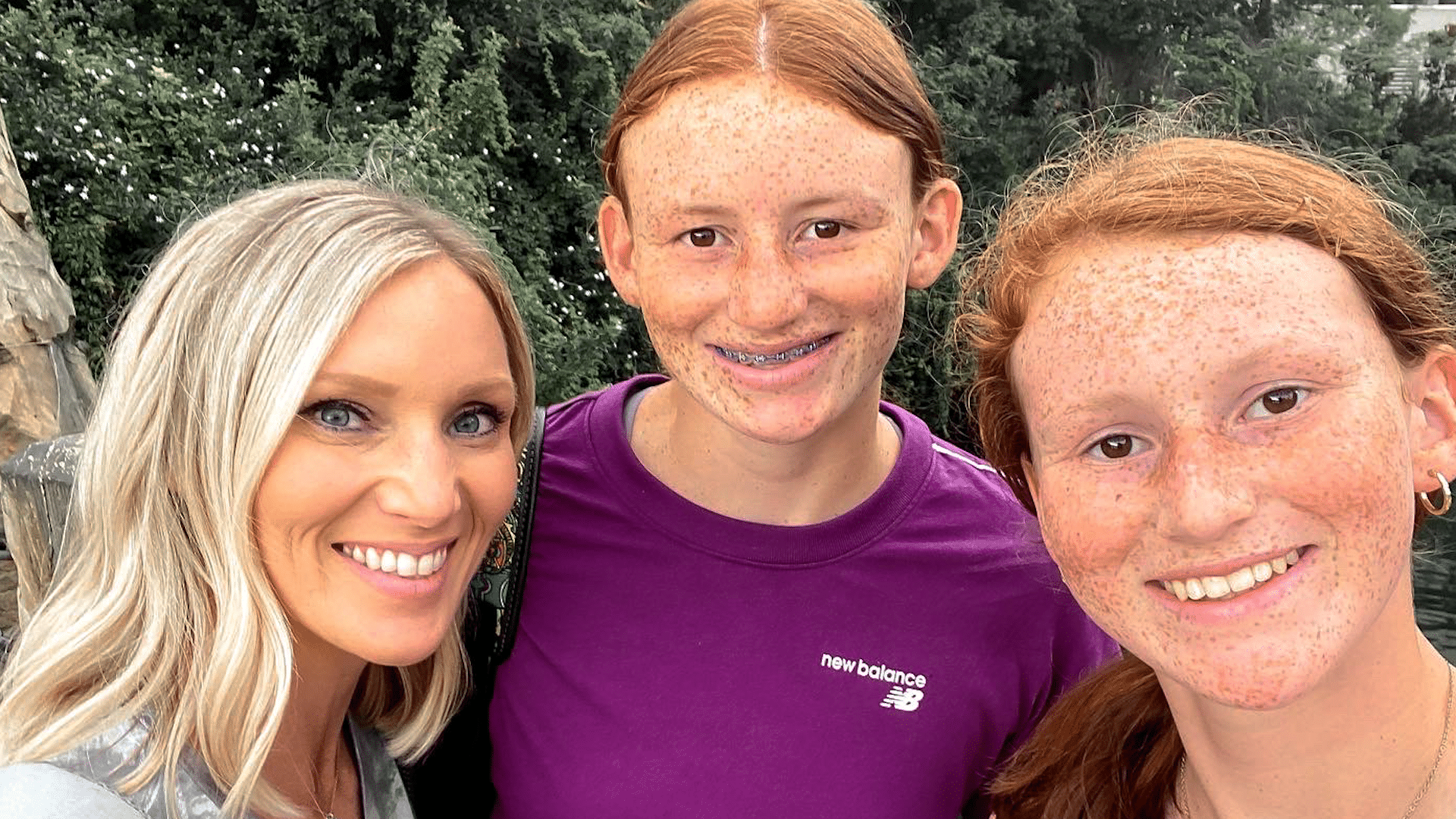
It started out as a typical holiday weekend for Dana Parker and her two daughters.
“We had plans to go hang out with my family the next day, for a cookout,” Dana said, about their plans last summer. “Fourth of July is a big holiday in our family.”
But overnight, those plans for a celebration quickly changed.
“I woke up a few times the next morning and thought, ‘Man, the house is really quiet. I’m surprised the girls aren’t up yet,’” Dana said.
Next came a horrifying discovery, as Dana found her oldest daughter Parker unresponsive on their living room floor.
“She’s just covered in vomit. She had definitely aspirated, I can hear it gurgling in her lungs,” Dana said, as she recounted the experience that day. “Her body is cold, I mean it is cold, stiff, she’s not responsive at all.”
Dana then finds herself reeling as first responders hone in on a possible cause. “They just kept saying, ‘Do you think it could be an overdose?’ They’re hooking her up to all these things and they just keep going back, like ‘Ma’am, she’s young, she’s healthy, all of these symptoms point to an overdose,’” she said.
Evidence found on Parker’s cell phone confirmed those suspicions. “In the course of about 25 minutes, she consumed almost 26 shots of alcohol,” Dana said.
“Depending on how old you are, how much you weigh, how much alcohol you’re ingesting, every child is different in terms of the effect it’s going to have on you,” Nicole Belcher, PA-C, a physician assistant at the James and Connie Maynard Children’s Hospital at ECU Health Medical Center (VMC).
In Parker’s case, she consumed enough alcohol for the care team at the Children’s Emergency Department at VMC to warn of an unknown outcome.
“They said, ‘At this point we don’t know if she’ll wake up. And if she does we have no idea what condition she’ll be in,’” Dana said. “She was already on borrowed time. I mean, it is literally by the grace of God that she was even still breathing at that point.”
Breathing then – and thriving now. While minor nerve issues persist, the multi-sport student athlete has made nearly a full recovery. And Dana is grateful for the care her daughter received.
“The little things that they do mean more than what they realize. Just the little kind words and taking the time to ask the questions and to say, ‘Hey, are you ok? Is there anything I can get you?’ I would just love to say ‘thank you,’” Dana said.
Now Dana wants other parents to learn from her family’s experience, and to consider how they talk to their children about the dangers of drinking.
“In her eyes, maybe she was drinking responsibly. She wasn’t out on the street, she wasn’t at a party, she wasn’t driving, you know – she’s in the comfort of her own home. She gets curious, she wants to experiment,” Dana said.
Experts agree.
“Bottom line, is to have the conversation. I think the earlier we walk about it, the better,” said Belcher. “The reality is, they are going to learn it from you, or they’re going to see it on social media, they’re going to see it on television, they are going to see it on the movies. Being able to have that open communication and being able to model safe behaviors with alcohol is the most important thing.”
Resources
April is Alcohol Awareness Month. If you or a loved one needs support, resources or treatment, the Substance Abuse and Mental Health Services Administration (SAMHSA) can help.
SAMHSA’s National Helpline is free, confidential and accessible 24 hours a day, seven days a week: 1-800-662-HELP.
They also offer an online treatment locator: https://findtreatment.samhsa.gov/
Watch more ECU Health News videos
For the first time since 2019, one of East Carolina University’s most exciting annual events returned to an in-person format Friday when 82 fourth-year medical students learned where they will be spending the next three to seven years completing residency training.
Surrounded by their family and friends during the Match Day event in ECU’s Health Sciences Student Center, the students simultaneously opened envelopes containing the location and medical specialty they will practice.
In staying true to the Brody School of Medicine’s mission to increase the number of primary care physicians who serve North Carolina, especially in rural and underserved areas, 61% of this year’s students matched into primary care residencies. And 35% of the class matched into residency programs in North Carolina.
“We continue to excel in our mission,” said Dr. Michael Waldrum, dean of the Brody School of Medicine and CEO of Vidant Health. “So this a special day filled with excitement, optimism and pride in what these students have accomplished and where they’re going. We trained them and now they’re ready to go.”

For Waldrum, the Match Day event was special on a personal level.
Not only was this his first Match Day as Brody’s dean, his college roommate’s son, Mark McAlister, was one of the Brody students who matched this week.
Before McAlister chose a medical school, his father reached out to Waldrum — who was still years away from becoming Brody’s dean — to ask his opinion on which medical school to choose.
Waldrum recommended Brody because he considered it the highest value medical school in the nation and would provide him with quality preparation for any career path he chose.
Four years later, McAlister said he was glad he followed that advice.
“As fourth-year students we started to learn what good work goes on here, in terms of patient care and learning. And it felt like this was a spot where we could continue to excel as professionals and develop our careers,” he said.
That advice also helped McAlister meet his soon-to-be wife, Jacqueline Poston, who was the first classmate he met at Brody.
On Friday, McAlister and Poston learned that they both matched at ECU Health Medical Center and ECU in Greenville.
“Our priority was staying together and being part of a good program, so we are lucky that we got both of those things,” said Poston, who will be training in internal medicine-pediatrics. “We’ve grown so much as medical students here and I can’t wait to see how much more we grow as residents. It’s an amazing place to be, so we’re really happy.”

Improving accessibility for all patients
K’Shylah Whitehurst knew that wherever she matched, home is right here waiting.
Whitehurst, a Greenville native and ECU chemistry graduate, wants to eventually practice in Pitt County with her family close by and the special patient base she spent years preparing to care for — children.
On Friday afternoon, she opened her envelope, read it and then flipped it over to show her family that she will complete a residency in pediatrics at University of North Carolina Hospitals in Chapel Hill. As she hugged one of her grandmothers, the tears began to flow and continued with each hug as she went down the row of her family members in attendance.
“I’m so excited. I’ll be close to home. My family will still be nearby. This is one of my top programs, so I’m really, really happy. I’m so excited to continue on this next chapter,” she said. “This will be my first time living outside of Greenville, but it’s not too far so that’s fine.”
Whitehurst said she looks forward to returning to eastern North Carolina after residency to care for children in this region.
“One of the main reasons I decided to go into pediatrics was how resilient children are. Most of the time the children that we’ve seen in the hospital here at Vidant are going through the scariest times of their lives,” she said. “Caring for children not only involves nurturing relationships with my patients, but also gaining the trust of parents to care for their little ones. I’m so excited to start my career as a pediatrician.”
Whitehurst, a first-generation college student who knew she wanted to be a doctor by the time she was 8 years old, said Brody’s focus on serving the underserved and ensuring a diverse student body made the difference for her.
“I love the fact that year after year, the school works to have the most diverse student body. Now that I’ve reached the end of my four years of medical school, I know that I 100% made the right decision to come to Brody,” she said. “The connections that I was able to form with the faculty here is something that I will forever be grateful for.”
During her Brody experience, Whitehurst was selected for the service-learning distinction track, a four-year program that encourages students to work extensively with medically underserved, marginalized and rural populations throughout medical school. She volunteered at the Lucille Gorham Intergenerational Community Center and worked with Brody’s Department of Pediatrics to improve resource accessibility to patients. She also earned an ethnic and rural health disparities graduate certificate through the track.
Whitehurst also had the opportunity to participate in a national research project, “WE CARE Project-Reducing Socioeconomic Disparities in Health at Pediatric Visits,” which studies social determinants of health and works to increase patient access to resources. Whitehurst used a special database to learn about resources in Pitt County.
“Through participating in the WE CARE Project, I was able to learn about what resources are available for patients here in Pitt County,” she said. “When treating a patient, it’s so important to remember that they are a human being first. Ensuring that their basic needs such as food security and electricity in their homes are met are so significant toward the patients being able to even consider making it to a yearly doctor’s appointment. I do feel better equipped to consider every aspect of a patient’s life to provide the best treatment for them.”
A calling answered
After graduating from the University of North Carolina at Chapel Hill with a degree in political science, Lumberton native Ross Masters worked in Washington, D.C., for a year in sales before realizing that career path was not the right fit for him.
He instead found his true calling in medicine after taking an EMT-Basic course back home in North Carolina. Shortly after completing the course, Masters witnessed a hit-and-run automobile crash and experienced the fulfillment of “knowing what to do and being useful” during a real-life emergency.
Masters went back to school to complete his medical school science prerequisites and earned a Brody Scholar award, which is ECU’s most prestigious scholarship.

On Friday, Masters and his fiancée, Camille Bauer, learned that they both matched to Vanderbilt University Medicine Center in Tennessee where Bauer will train in obstetrics-gynecology and Masters will train in psychiatry.
“It’s an indescribable feeling,” Masters said. “Brody has treated us fantastic. We have had access to awesome mentors. Everyone has been super supportive and prepared us well for residency. So we’re feeling great about what Brody has done for us and we’re feeling great about the future as well.”
When Masters arrived at Brody, he was drawn to family medicine because he wanted to help address some of the social determinants of health that he witnessed as an EMT. However, his focus changed after he took part in patient psychiatry education at Brody.
“We were sitting down with social workers, pharmacists and therapists and I felt I was able to provide that whole comprehensive treatment to patients through psychiatry,” he said.
For Masters and Bauer, Match Day represented a major life moment, but it will not be the only one before they start residency training.
“We got a successful couple’s match, which is what we really cared about today,” Bauer said. “We met our first year and started dating about six months later. And now we’re getting married next month.”
‘I want to walk alongside my patients’
Emmanuella Mensah’s journey from her hometown of Charlotte to the Brody School of Medicine has come full circle. After graduation, she will be returning to Charlotte for a family medicine residency with the Carolinas Medical Center Biddle Point Urban Track, where she will train to care for underserved populations.
Mensah’s parents, Ofori and Theresa Mensah, and siblings Gloria and Ofori Jr., all from Charlotte, along with friend and third-year medical student Merdi Lutete were with her on Friday. Her mom said she was so happy that her daughter would be returning home for residency.
“I feel blessed, and I feel good. Thank you Jesus,” Theresa said. “I can have my baby back.”
The residency location was Emmanuella’s top choice, and after reading the match letter, everything was still sinking in.
“I’m very excited and I’m very grateful to know that someone wanted to train me,” she said.
Mensah earned her undergraduate degree at UNC-Chapel Hill and completed Brody’s Summer Program for Future Doctors, which helped her decide that ECU would be a good fit for medical school.
“The magic of Brody is the medical students, and meeting students during that summer, I really felt at home, and I really wanted to be a part of that legacy,” Mensah said. “Brody has meant everything to me. Brody took a chance on me when no one else would take a chance on me, and they’ve been instrumental in my growth as a student.”
Born and raised in Ghana before moving to Charlotte at 10 years old, Mensah believes she can make a difference through family medicine in communities near and far.
“For me, there is no separation between the community and medicine — to take care of a person, you have to understand who they are and what they face when they step out of the clinic,” she said. “I came into medical school with a strong interest in family medicine because I want to provide valuable health care to underserved populations in North Carolina and in Ghana.”
Mensah used her participation in the medical education and distinction teaching track to explore narrative medicine — the use of stories to create a therapeutic alliance between patient and physician — in helping students develop empathy and listening skills. She wants to continue that exploration during her residency.
“We all carry our own stories, but how do doctors represent their patients’ stories accurately? This has been an interest that has developed here at Brody, and I look forward to seeing how it transforms during residency,” she said.
Mensah is also a co-founder of the I Am First organization at Brody, a group that provides first-generation medical students with mentorship from community physicians.
“Even though COVID-19 shut down the world before our first official meeting, due to the diligence of the team members, we were able to keep the organization going,” she said. “I am excited to see how I Am First will continue to grow as it seeks out more mentors and maintains our community.”
Mensah is also a member of the Gold Humanism Honor Society for her service to the community. Her penchant for service, medicine and improving the world led her where she is today.
“Although I am nervous for my next step in my journey, I believe Brody has prepared me well to handle the stress and pressures of residency,” she said. “I will always remember to keep the patient and myself first as I learn the intricacies of residency — extending grace where it is needed. Ultimately, I think Brody has prepared me to begin to effectively address both the science and art of medicine.”
Read more through ECU News Services.
Edenton, NC – March 17, 2022 – Dr. Michael Waldrum, CEO of Vidant Health and Dean of the Brody School of Medicine at East Carolina University, joined Vidant Chowan Hospital President Brian Harvill at the Edenton Rotary Club meeting Thursday to discuss the exciting future of ECU Health and the impact high-quality health care has on the vibrancy of eastern North Carolina.
The presentation to the Edenton Rotary Club is one of several planned this spring and summer to meet with community groups throughout the region.
“Every time I visit Edenton, I’m reminded that Vidant Chowan is one of the most important parts of this community,” Dr. Waldrum said. “Edenton and the surrounding towns have a great hospital where they can deliver babies, receive high-quality care and build their sense of community. We value the role of rural hospitals and that is why it is so important for us to have conversations about how we can best deliver health care across the region.”

ECU Health – the joint enterprise between Vidant and Brody launching in the spring – was at the top of the agenda. Vidant Health enables the two organizations, which have worked collaboratively for years, to come together under a shared brand to provide streamlined care across the hospital system. A logo will be revealed in April and re-branding, which is expected to take months to complete, will begin in May.
Dr. Waldrum said ECU Health is the natural culmination of the two organization’s long partnership and shared mission of improving the health of eastern North Carolina. ECU Health will build on successful innovations such as the MOTHeRS Project, which is a grant-funded program through Vidant that connects mothers in rural areas to resources for nutrition, behavioral health needs and maternal fetal medicine resources. This program is beginning in Edenton and highlights the importance of collaboration to solve complex health issues in the region, Dr. Waldrum said.
“Having babies and being able to give birth here is really important to Edenton,” Dr. Waldrum said. “Babies that are born here are more likely to stay here when they grow up. We want to support that in an innovative way by providing access to care that meets the community’s need. The MOTHeRS Project is a great example of how Brody, Vidant and the future ECU Health will tackle complex challenges and bring a higher quality of care to the region.”
With Rotary Club members in attendance, Dr. Waldrum also spoke on the impact that access to care has on a community’s economic vibrancy. He shared that Vidant, which employs more than 13,500 team members, has a $4 billion economic impact on the region. Locally, Vidant Chowan has more than 500 team members and has a $61.3 million impact on the local economy. These numbers, Dr. Waldrum said, represent Vidant and the future ECU Health’s commitment to caring for the community.
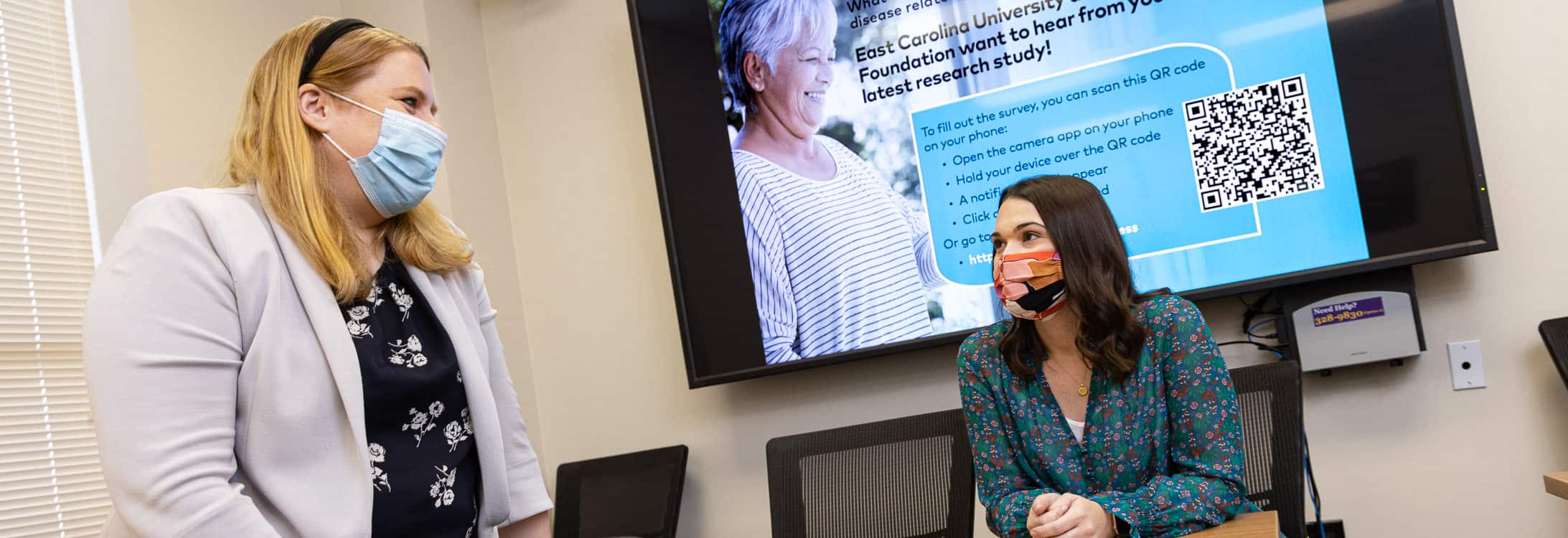
East Carolina University researchers are hoping to understand which resources are available to those with Parkinson’s disease (PD) in eastern North Carolina, how they are being utilized, and what types of services are most needed.
ECU College of Allied Health Sciences faculty members Dr. Kathrin Rothermich and Dr. Lauren Turbeville, along with cross-campus collaborator Dr. Jennifer Hodgson (Department of Human Development and Family Science), local individuals with Parkinson’s, and support from The Parkinson’s Foundation, are conducting a survey for individuals in eastern North Carolina with Parkinson’s disease.
They hope that with more precise data on the challenges that eastern North Carolinians with Parkinson’s face, they’ll be better positioned to lobby for those resources.
“This is really about how we can help them now with resources,” said Rothermich, an assistant professor in the Department of Communication Sciences and Disorders. “To do that, we really need to know what’s needed, what’s a priority, and what the biggest concerns are.”
Parkinson’s Disease (PD) is a neurodegenerative brain disorder that leads to uncontrollable movements, stiffness and difficulty with everyday activities like walking, balance, cognition, swallowing and speaking. It is challenging to diagnose and there is currently no known cure.
Approximately 60,000 people in the U.S. are diagnosed each year, and nearly 1 million people nationwide are living with PD, according to the Parkinson’s Foundation. But for those patients living in eastern North Carolina and other rural areas, the specialist treatment they need can be difficult to access, which also results in a lack of awareness about the other resources available to them.
“There’s not much east of Raleigh for people with PD in terms of a movement disorder specialist,” said Turbeville, an occupational therapist and assistant professor in the College of Allied Health Sciences’ Department of Occupational Therapy. “That’s typically who diagnoses and ideally treats them.”
Turbeville has witnessed first-hand the struggles that those with Parkinson’s often face in accessing the care they need — particularly when they live in rural areas.
“My dad has Parkinson’s and my granddad had Parkinson’s,” she said. “My dad lives in South Carolina and has someone drive him three hours to Charleston to see a movement disorder specialist once every six months. He’s lucky because he has me and I’m an OT, but other people don’t have that luxury and are missing out on a lot of opportunities for other specialties.”
Similarly, because there are no movement disorder specialists in the eastern part of North Carolina, patients often must find help to make long journeys to those appointments.
There are, however, other allied health professionals in the East trained to help manage a person’s PD symptoms — including physical therapists, occupational therapists and speech-language pathologists. Because patients lack a go-to specialist or center in the region, they’re not always aware of these resources available to them that are often covered by their insurance, and it’s difficult to track whether PD patients are able to access the other resources they need.
Rothermich and Turbeville hope that their survey — which they said should take about 10-15 minutes to complete — will lead to those answers and guide their next steps toward lobbying for the most needed resources.
“PD is certainly not the only disease where people struggle finding care in this region, just because it’s so spread out, and also there’s a lot of socioeconomic insecurities and health literacy issues. All of these things come into play,” Rothermich said. “I think there are some communities we’re just not reaching right now, especially marginalized minorities that are not currently connected to PD support groups.”
“Regional transformation is at the heart of ECU’s mission,” College of Allied Health Sciences Dean Dr. Robert Orlikoff said. “Our focus on diagnosis, treatment, care and rehabilitation for the underserved helps empower individuals, families, and communities in the East lead better lives with more options and opportunities. Access to quality interprofessional health care, such as needed by those with Parkinson’s, will be key to this important effort.”
As ECU and Vidant Health partner to create Vidant Health in an effort to provide more comprehensive care and better service throughout the East, Rothermich and Turbeville think the time is right to explore these questions in more detail.
“Vidant Health will be a national model for academic rural health care and will pave the way for unique opportunities to quickly translate this kind of important research into improved health care delivery to those in need,” said Dr. Michael Waldrum, dean of ECU’s Brody School of Medicine and CEO of Vidant Health. “This shared focus on tackling the complex health care challenges of eastern North Carolina will better enable us to identify, address and advocate for the health needs of all residents in the East.”
If you’d like more information about this research, visit the ECU Social Communication and Neuroscience Lab website online. If you’re interested in helping or getting involved with this initiative, please contact Dr. Kathrin Rothermich ([email protected]) or Dr. Lauren Turbeville ([email protected]).
Greenville, NC – March 14, 2022 – As Vidant continues to respond to the evolving COVID-19 pandemic across North Carolina, we are taking steps to ensure the safety of all. Vidant remains vigilant with its screening process for all visitors, entry requirements and visitor restrictions by department.
In response to decreased community spread, Vidant is carefully expanding visitation across the system, including for COVID-positive patients. Effective 8 a.m. Wednesday, March 16, Vidant will adopt the below visitor guidelines. Visitors must wear surgical masks provided at screening stations or personal N95/KN95 masks as long as they are clean, intact, without a valve and have no visible gaps.

Despite the encouraging trend of cases, it remains vitally important for community members to continue to practicing safety measures such as washing hands, wearing a mask and avoiding large gatherings.
For the latest information on Vidant’s visitor restrictions, please visit VidantHealth.com/VisitingVidant.
This is an evolving situation, and Vidant continues to monitor the spread and examine local data, including COVID-19 cases in our region and in hospitals, and will adjust visitation restrictions accordingly.
Vidant strongly encourages visitors to consider virtual visitation options such as FaceTime and phone calls. Assistance with virtual visits, including iPads for patients without the necessary technology, is available on request. Virtual visitation is the safest way to stay connected with a loved one.
Patients should limit their belongings to a few key items and refer to the below tips:
- Bring your phone, tablet or other electronic device to connect with family members
- Limit clothing to clean undergarments and one outfit for discharge
- Wear or pack non-slip shoes
For the latest information on Vidant’s visitor restrictions, please visit VidantHealth.com/VisitingVidant.
February may be American Heart Month, but it is important to be aware of heart health all year long. During the pandemic, many people may have delayed or postponed heart screenings, which can negatively impact their health. Nearly a quarter of deaths in the United States are caused by heart disease. Although this is a staggering statistic, heart disease is often preventable with lifestyle modifications and medicines.
There are key factors that impact heart health that everyone should be aware of to maintain a healthy cardiovascular system. Risk factors are conditions that heighten your risk of heart attack, stroke and death. Some, like aging and genetics, can’t be controlled, but others can:
- Elevated blood pressure, or hypertension, is sometimes referred to as a silent killer because it doesn’t cause symptoms and accounts for most cardiovascular deaths because of its prevalence.
- Cholesterol levels, especially LDL — the bad cholesterol — can play a key role in buildup of plaque and blockages inside our blood vessels, increasing the risk of stroke and heart attack. About one third of US adults have a high LDL level (>130mg/dl). When it comes to cholesterol and blood pressure, lower is better.
- Diabetes is a major risk factor for heart disease that is heavily influenced by lifestyle. About 12% of adults in the U.S. are diabetic, and an alarming 30% are pre-diabetic. Aggressive control of blood pressure and cholesterol is especially important in diabetics.
- Smoking is a leading preventable cause of disease, disability and death (cardiac and otherwise) in the U.S. Almost one third of coronary deaths are related to smoking and second-hand exposure.
One of the most important ways to prevent heart disease is to control your risk factors and adopt a healthy lifestyle throughout life.
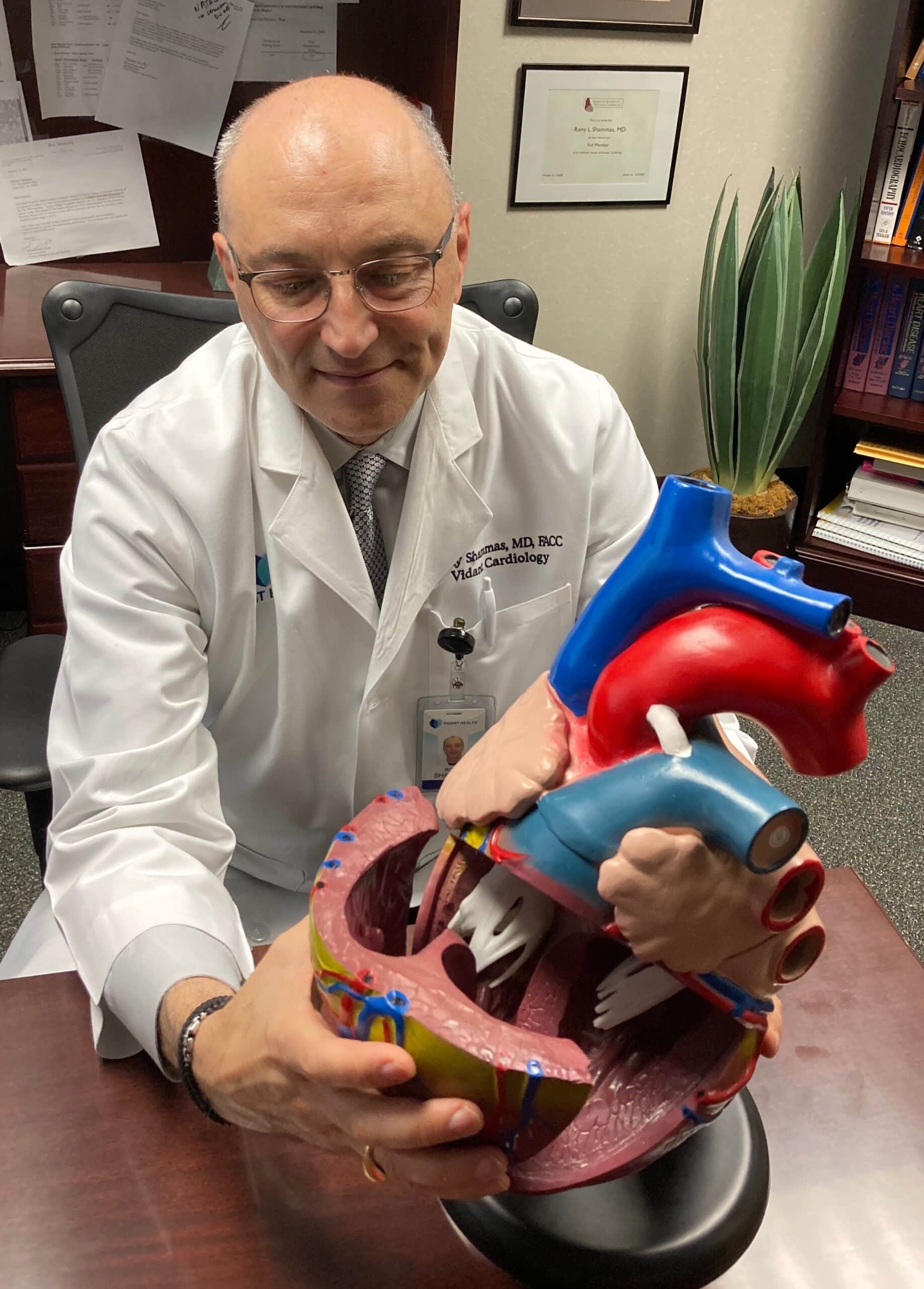
“An ounce of prevention is worth a pound of cure. Being proactive about your heart health is the best way to prevent and manage heart disease,” said Dr. Rony Shammas, interventional cardiologist and hypertension specialist for Vidant Health. “Plaque buildup in the blood vessels starts early on in life, even in our teens, so it is important to address your risk factors and adopt a healthy lifestyle as soon as you can.”
Positive changes in lifestyle that make an impact on heart health include:
- Diet: Eating a well-balanced diet that is rich in fruits, vegetables, nuts, legumes and whole-grains, and low in salt, saturated and trans fats, red meat and sweets and sugar-sweetened beverages promotes good heart health.
- Exercise (Physical Activity): The American Heart Association recommends at least 150 minutes per week of moderate intensity exercise. Almost half of adults do not meet the minimum recommendations for exercise. The American Heart Association recommends at least 150 minutes per week of moderate intensity exercise (i.e., brisk walking).
- Limit alcohol: If you don’t drink, don’t start. Otherwise, keep it to a minimum and don’t exceed one drink a day if you are a woman and two drinks a day for men ( 1 drink= 12oz beer, 5oz wine or 1.5 oz liquor)
- Managing stress: Some stress is good, but excessive stress can be damaging to the body. Breathing techniques, meditation, owning a pet and practicing yoga can help deal with stress.
Depending on your particular risk profile, your health care provider will decide if there is a need for medication to treat blood pressure, cholesterol and diabetes alongside lifestyle changes. If your doctor recommends medication, make sure you take it as prescribed.
Dr. Shammas advises that if you or a loved one suspect you may be having a heart attack or stroke, call 911. Immediate intervention can save your life and reduce your risk of disability. On the other hand, If you are having less acute but concerning symptoms seek medical attention early. After listening to your story and performing an exam, your doctor may order one of several diagnostic tests to decide if your symptoms are related to heart disease.
“Everybody wants to stay off my operating table, and these tips are key for heart disease prevention and helping minimize harmful conditions,” said Dr. Michael Bates, chief and clinical professor of cardiothoracic surgery at the Brody School of Medicine at East Carolina University and ECU Health Medical Center.
When someone is experiencing concerning symptoms, it is key to seek medical attention early. Patients are offered several diagnostic tests when they report symptoms like severe chest pains.
Noninvasive tests can be performed early in a patient’s heart history to look for signs of heart issues. Some of these include a stress test, an exercise stress test performed on a treadmill, which shows how your heart works during physical activity. During this time, your heart rate, blood pressure and the heart’s electrical signals will be monitored. Other noninvasive tests include an echocardiogram, which checks how the heart chambers and valves are pumping blood through your heart.
If heart surgery is needed, today’s advancement in surgical treatments have resulted in less invasive procedures and much faster recovery time than even ten years ago. Some surgeries can be performed through smaller incisions in the body with cameras. Robotic surgery also helps to make less invasive surgeries possible.
There are several less invasive surgeries for the heart. Bypasses can now be performed with assistance from robotic surgery through a smaller incision in the body. Cardiac catheterizations are used to repair the heart valves without making an incision in the chest cavity; instead, the procedure can be performed through arteries and veins.
“Bringing Vidant Health and the Brody School of Medicine together as Vidant Health will continue to extend our mission as a leader in rural health care,” Dr. Bates said. “This collaboration of excellence and combined resources will create even more advancements in our work in cardiac and vascular care.”
Dr. Shammas believes eastern North Carolina’s future is bright because of the outlook for Vidant Health.
“Ultimately, our hope is to make hearts healthier throughout the region and moving forward as Vidant Health strengthens our commitment and mission to bring the best in research and care to the communities we call home,” he said.
One of the most important things you can do for your heart health is to see your provider for screenings and check-ups, which are key to preventing problems before they arise. For more information about cardiovascular resources at Vidant Health, including treatments and technologies, visit www.ecuhealth.org and the Heart & Vascular Care section of the website.